
Учебники / Operative Techniques in Laryngology Rosen 2008
.pdf
|
Chapter 40 |
259 |
Fig. 40.3 The paraglottic space is connected between the posterior cartilage border and the ML window
to avoid perforation of this delicate mucosa. The pyriform |
Fig. 40.4 Posterior “cookie-bite” window is created with a Kerrison |
rongeur |
|
mucosa can be seen extending anteriorly onto the poste- |
|
rior cricoarytenoid (PCA) muscle. To aid in its identifica- |
|
tion, the patient is asked to blow against pursed lips (“blow |
|
out the birthday candles”), which results in distension and |
|
easy identification of the pyriform mucosa. The mucosa |
|
is grasped and dissected posteriorly, using blunt dissec- |
|
tion with a Kitner (Fig. 40.6). The pyriform can then be |
|
shielded under a Sewell retractor (Fig. 40.7). |
|
8.The muscular process can then be identified using a number of landmarks. The muscular process is usually at the same vertical height of the vocal fold and found by tracing the fibers of the PCA muscle anterior/superiorly to its tendinous insertion (Fig. 40.8). The muscular process is small (about the size of a grain of rice), but can be palpated. In addition, if the cricothyroid joint is separated as in step 6b, then this can be used as a nearby landmark, as the muscular process can be reliably found within 1 cm above this point. By grasping the muscular process with a toothed forceps, and rotating the arytenoid (anteriorly), one should be able to easily rotate the arytenoid into a medial position while confirming this with the endolaryngeal image on the monitor (Fig. 40.9).
9.In order to obtain a secure purchase on the muscular process, a 4-0 monofilament suture (double armed) is passed through the lateral edge of the muscular process in a figure of eight fashion (Fig. 40.10).
10.Both needles are brought through the dissected paraglottic space into the medialization window, taking great care
not to inadvertently catch any tissue with the needle tips, Fig. 40.5 Alternately, the cricothyroid joint can be divided for poste-
which could adversely affect the vector of pull for the AA stitch. Generally, the needles are passes with the dull end as the leading edge (Fig. 40.11).
11.One of the needles is passed through the cartilage anterior to the medialization window, using a 1-mm wire-passing drill bit if the cartilage is calcified (Fig. 40.12). The other needle is passed underneath the inferior strut and is secured anteriorly through the anterior cricothyroid membrane (Fig. 40.13).
12.The two ends of the suture are then clamped with hemostats. The sutures are gently pulled anteriorly to adduct the
rior exposure
arytenoid, and the effect on the voice is tested by having the patient count from 1 to 10. In addition, at this time the effects of medialization, using the previously mentioned depth gauge instrument are tested both in isolation, and with the addition of tension of the AA suture.
13.Once the implant is created, it is placed through the window, taking care to keep the AA suture lines deep to the implant (Fig. 40.14).

260 |
Arytenoid Adduction |
|
Fig. 40.6 The pyriform mucosa is dissected posteriorly using a Kitner
40
Fig. 40.7 Axial representation of larynx after posterior pyriform mucosa dissection/protection with Sewell retractor
Fig. 40.8 Muscular process of the arytenoid is identified
Fig. 40.10 A 4-0 double-armed Prolene suture is passed through the muscular process in a figure of eight fashion
Fig. 40.9 Axial representation of manual traction on the muscular process to demonstrate adduction of the vocal fold

|
Chapter 40 |
261 |
Fig. 40.11 Passage of the suture through the ML window
Fig. 40.12 A 1-mm wire-passing drill bit is used to create an anterior passage for one arm of the AA suture near the midline
Fig. 40.13 After successful passage of both arms of the AA suture through the midline
Fig. 40.15 Final tying of a surgeon’s knot over the thyroid ala |
Fig. 40.14 Axial representation of AA sutures deep to ML implant |

262 |
Arytenoid Adduction |
14. |
Finally, the AA suture tension is adjusted and the knot is |
|
secured over the anterior thyroid cartilage, again assessing |
|
the voice. In general, only a small amount of tension is |
|
required for this (Fig. 40.15). |
15. |
Sternohyoid muscle is re-attached. Wound is closed in lay- |
|
ers. Drain is placed at the surgeons discretion. |
40.6 Postoperative Care
|
|
and Complications |
|
Postoperatively, care should encompass: |
|
|
■ Overnight, 23-hours observation |
|
|
■ |
Pain management |
|
■ Intravenous corticosteroids at 8-hour intervals (Decad- |
|
|
|
ron, 8 mg, then 4 mg) |
|
■ Elevation of the head of bed |
|
|
■ A return to clinic is scheduled 2–4 weeks after surgery |
|
40 |
■ In general, the patient’s voice is poor within 6–8 hours |
|
|
after surgery, due to edema. |
|
■An additional corticosteroid taper may be warranted on discharge from the hospital.
Complications and common surgical errors include laryngeal edema with airway compromise, which is more common with framework surgery that involves AA. The additional retraction and dissection necessary for exposure and manipulation of the arytenoid complex results in increased paraglottic and arytenoid edema post operatively. Additional corticosteroids may be warranted in patients undergoing ML and AA.
Pharyngocutaneous fistula is a possible complication with AA, although it is quite uncommon. Careful handling of the pyriform mucosa and protection of the mucosa with a retractor should prevent this complication. If an injury to the mucosa is suspected, then the field can be irrigated and the patient instructed to perform the Valsalva maneuver. If air bubbles occur during this maneuver, then the pyriform mucosa should be repaired with absorbable suture, and the patient should be retested for air leakage. One should consider whether it is prodent to proceed with the ML and/or AA at this point.
Excessive tension on the AA suture can create over-rotation of the arytenoid and worsening of the voice. The tension needed on this suture is actually minimal in most cases; therefore, the surgeon should err on the side of light tension on the AA suture.
Key Points
■Arytenoid adduction (AA) is a framework surgery where the pull of the LCA muscle is recreated to achieve vocal fold repositioning. The physiologic effects of AA include the following:
■Lowers the position of the vocal process
■Medializes and stabilizes the vocal process
■Lengthens the vocal fold
■Rotates the arytenoid cartilage
■AA is used as an adjuvant surgical treatment along with ML in cases of vocal fold paralysis where one of the following occurs:
■Posterior glottic gap/lateralized vocal fold during phonation
■Vertical height differences between vocal folds (generally the paralyzed vocal fold is superiorly located)
■Severely foreshortened vocal fold
■Inability to achieve good voice intraoperatively with ML alone
■AA requires a posterior dissection technique separate from ML, where either a posterior window in created in the thyroid ala, or the cricothyroid joint is divided to allow outward retraction of the posterior thyroid ala.
■The pyriform mucosa must be dissected off the muscular process of the arytenoid to allow proper exposure of this structure.
■A double-armed needle is secured at the muscular process of the arytenoid and passed anteriorly near the midline of the thyroid ala to recreate the pull of the LCA muscle. The sutures lie deep to the medialization implant.
■The needles from the AA sutures should be passed through the paraglottic space carefully (dull end as the leading edge) to avoid picking up soft tissue, which may change the vector of pull.
■Only mild–moderate tension is required on the AA suture to achieve desirable arytenoid positioning.
Selected Bibliography
1McCulloch TM, Hoffman HT, Andrews BT et al (2000) Arytenoid adduction combined with Gore-Tex medialization thyroplasty. Laryngoscope 110:1306–1311
2Woo P. Arytenoid adduction and medialization laryngoplasty (2000) Otolaryngol Clin N Am 33:817–839
3Noordzij JP, Perrault DF, Woo P (1998) Biomechanics of combined arytenoids adduction and medialization laryngoplasty in an ex vivo canine model. Otol Head Neck Surg 119:634–642
4Woodson GE, Picerno R, Yeung D et al (2000) Arytenoid adduction: controlling vertical position. Ann Otol Rhinol Laryngol 109:360–364
5Isshiki G (1978) Arytenoid adduction for unilateral vocal cord paralysis. Arch Otolaryngol 104:555–558
6Miller FR, Bryant GL, Netterville JL (1999) Arytenoid adduction in vocal fold paralysis. Oper Tech Otolaryngol Head Neck Surg 10:36–41
Chapter 41
Cricothyroid Subluxation |
41 |
|
41.1 Fundamental and Related Chapters |
41.4 Surgical Equipment |
Please see Chaps. 5, 36, 37, 38, 39, and 40 for further information.
41.2Disease Characteristics and Differential Diagnosis
Cricothyroid subluxation was developed by Steve Zeitels to address the problems of a shortened vocal fold frequently seen in unilateral vocal fold paralysis. The concept of the procedure is to lengthen the vocal fold by increasing the distance from the cricoarytenoid joint (cricoid) to the anterior commissure (thyroid cartilage) by subluxating the cricothyroid joint on the side of the unilateral vocal fold paralysis. This results in a rotation of the anterior commissure away from the midline in a direction contralateral to the side of the unilateral vocal fold paralysis.
Cricothyroid subluxation is an adjunct procedure to medialization laryngoplasty. This can be done with arytenoid adduction also, but is typically used with medialization laryngoplasty. Cricothyroid subluxation addresses the commonly seen problem of a shortened vocal fold associated with unilateral vocal fold paralysis. The only other procedure that can lengthen a paralyzed vocal fold is arytenoid adduction (see Chap. 40, “Arytenoid Adduction”).
41.3Surgical Indications and Contraindications
Indications for cricothyroid subluxation involve:
■Unilateral vocal fold paralysis associated with vocal fold shortening with resultant glottal insufficiency and reduced pitch range (preoperative assessment)
■Poor pitch range and/or significantly shortened vocal fold, as seen on endoscopy during medialization laryngoplasty after adequate implant positioning (intraoperative)
Contraindications include present or impending laryngeal fracture of thyroid ala from the associated medialization laryngoplasty procedure.
Surgical equipment needed for cricothyroid subluxation comprises:
■See “Surgical Equipment” sections in Chaps. 38, “Si-
lastic Medialization Laryngoplasty for® Unilateral Vocal Fold Paralysis” and 39, “GORE-TEX Medialization Laryngoplasty.”
■Right-angle clamp (vascular clamp)
■2-0 Prolene suture with narrow diameter, semicircle needle
■Surgical headlight
41.5Surgical Procedure
1.Cricothyroid subluxation is done as a planned procedure in conjunction with medialization laryngoplasty, or done immediately after a medialization laryngoplasty due to a restricted pitch range despite a well-positioned medialization laryngoplasty implant.
2.Further dissection than what is typically performed for a medialization laryngoplasty approach alone is required. Complete skeletonization of the inferior cornu of the thyroid cartilage should be performed using electric cautery or cold steel instrumentation. This will involve removal of the cricothyroid muscle immediately anterior and inferior to the inferior cornu and release of the inferior constrictor muscle off the posterior aspect of the inferior cornu. The recurrent laryngeal nerve is at risk in this region; thus, it is wise to keep dissection close to the inferior cornu of the thyroid cartilage to avoid deinnervation of the immobile but partially reinnervated vocal fold.
3.Soft tissue overlying the superior and inferior aspect of the cricoid cartilage at the midline should be removed.
4.Separation of the cricothyroid joint
This can be done using a scissors or a cottle elevator. Care should be taken during this step not to fracture the inferior cornu. The use of scissors to separate the cricothyroid joint is most likely less traumatic to the inferior cornu. The blades of the scissors are placed up against the posterior, lateral aspect of the cricoid cartilage to allow the tips of the scissors to be positioned on either side of the cricothyroid joint (Fig. 41.1).
5.After separation of the cricothyroid joint, care should be taken to insure the inferior cornu of the thyroid cartilage is completely free of any soft tissue attachments.

264 |
Cricothyroid Subluxation |
|
41
Fig. 41.1 Separation of cricothyroid joint with scissors
6.A 2-0 Prolene suture is then passed around the neck of the inferior cornu. This can be done with a relatively narrow diameter, semicircle needle, or by using a right-angled clamp (vascular clamp) to pass the free end of the suture around the neck of the inferior cornu. The suture should be positioned as superior as possible on the neck of the inferior cornu and then tied with relatively equal lengths of the suture on both sides of the knot.
7.The arm of the suture with the needle is then passed underneath the cricoid cartilage anteriorly at the midline. Care should be taken not to fracture the cricoid cartilage and to pass the needle in a submucosal plane under the anterior aspect of the cricoid ring (Fig. 41.2).
8.The free end of the suture tied at the inferior cornu is then tied to the end of the suture passed underneath the anterior cricoid cartilage. The voice and vocal fold length (endoscopically) should be evaluated as tension is applied to the knot (Fig. 41.3). Typically, only moderate tension is required to position the inferior cornu into an anterior, subluxated position. This anterior subluxation of the inferior, cornu of the thyroid cartilage results in vocal fold lengthening and an expanded pitch range (Fig. 41.4). Once an optimal tension is found (predominantly by perceptual voice assessment), the suture is secured with several surgical knots.
Fig. 41.2 Placement of cricothyroid subluxation suture submucosally at the midline of the anterior cricoid cartilage
41.6Postoperative Care and Complications
Postoperative care is identical to that of medialization laryngoplasty. The reader is referred to Chaps. 38, “Silastic Medialization Laryngoplasty for Unilateral Vocal Fold Paralysis” and 39, “GORE-TEX® Medialization Laryngoplasty” for details.
Complications involve:
■Fracture of the inferior cornu
■To remedy this complication, a suture can be placed through the thyroid cartilage near the fracture line and then be used in a similar fashion as described above to complete the cricothyroid subluxation.
■Fracture of the main aspect of the thyroid cartilage ala
■If fractures of the thyroid cartilage ala occur, then all fractures should be reduced and secured with either suture or plating and the cricothyroid subluxation procedure should be aborted (see Chap. 44, “Repair of Laryngeal Fracture”).

Chapter 41 265
Key Points
■ Cricothyroid subluxation is an adjunctive procedure to medialization laryngoplasty which lengthens the shortened vocal fold associated with unilateral vocal fold paralysis.
■ Cricothyroid subluxation rotates the anterior commissure attachment of the vocal fold away from the cricoarytenoid joint, thus lengthening the vocal fold.
■ Care should be taken not to fracture the inferior cornu of the thyroid cartilage during the procedure.
■ Excessive tension applied to the suture securing the cricothyroid subluxation position may worsen voice quality.
Bibliography
1 Zeitels SM (2000) New procedures for paralytic dysphonia: adduction arytenopexy, Goretex medialization laryngoplasty, and cricothyroid subluxation. Otolaryngol Clin North Am 33:841–854
2 Zeitels SM, Hillman RE, Desloge RB, Bunting GA (1999) Cricothyroid subluxation: a new innovation for enhancing the voice with laryngoplastic phonosurgery. Ann Otol Rhinol Laryngol 108:1126–1131
Fig. 41.3 Suture fixation of cricothyroid subluxation
Fig. 41.4 Axial view of vocal fold position before and after cricothyroid subluxation

Chapter 42 |
|
Translaryngeal Removal |
42 |
of Teflon Granuloma |
42.1Fundamental and Related Chapters
Please see Chaps. 24, 36, 37, 38, and 40 for further information.
42.2Disease Characteristics and Differential Diagnosis
In every Teflon injection, an inflammatory response to the Teflon occurs. In most cases, the inflammatory response remains localized, and no significant clinical complications are noted. However, there is a risk of clinically evident expansile granuloma formation in these patients if long-term follow up (10 years or more) is used. Often this occurs years after the initial injection, after a prolonged period of good voice. Anecdotal
evidence suggests that subsequent laryngeal trauma (i. e., intubation) may contribute to growth of the granuloma.
Teflon granuloma is typically a submucosal smooth mass that presents as a bulge in the false vocal cord, ventricular mucosa, and/or the true vocal fold. The granuloma may grow inferiorly resulting in a subglottic bulge as well. Videostroboscopy is quite consistent in these patients, revealing a stiff, nonvibratory vocal fold mass. This is due to either a mass effect (stretching of vocal fold mucosa with dampening of wave) or, more commonly, the infiltration of the granuloma into the lamina propria and/or mucosa. Glottic incompetence is commonly present, secondary to the mass lesion. Occasionally, the patient’s airway is compromised, especially if the granuloma is subglottic.
It is helpful to obtain a CT scan of the neck with contrast to assess the location of the Teflon and extent of granuloma formation. In this way, superficial Teflon granulomas can be distinguished from more extensive granulomas, which guides the surgeon in choosing the appropriate approach (endoscopic, see Chap. 24 “Endoscopic Management of Teflon Granuloma”) versus the external approach described in this chapter). Typical CT appearance is a brightly enhancing, fairly well-circum- scribed mass in the paraglottic space.
42.3Surgical Indications and Contraindications
Indications include:
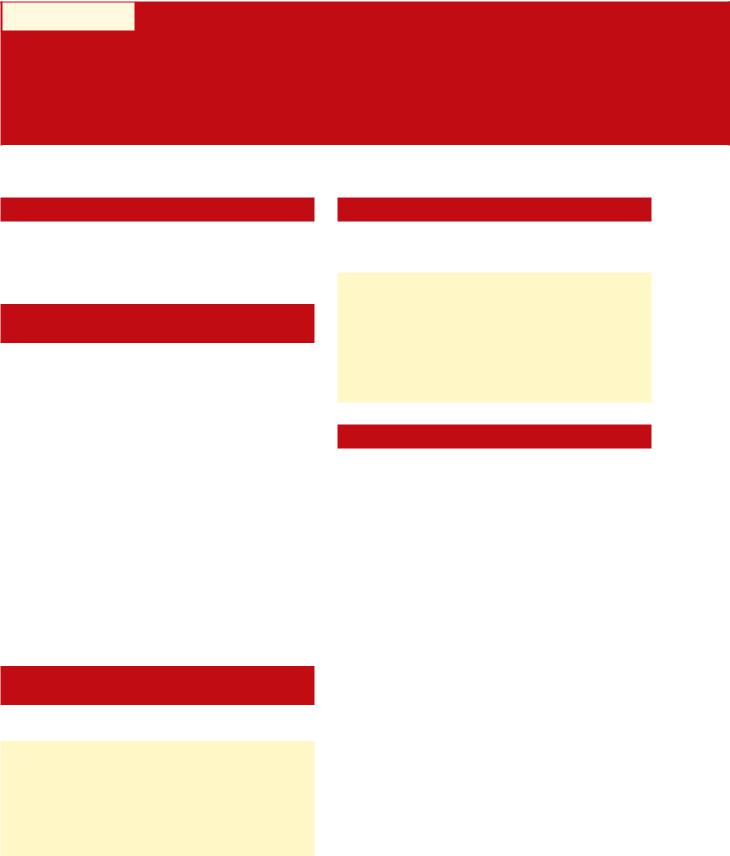
■Symptomatic Teflon granuloma in a patient with UVFP in which there is sparing of the free edge of the vocal fold (vocal ligament/mucosa appear uninvolved with granuloma) (Fig. 42.1)
■Desire for complete removal of granuloma
Relative contraindications although these are not absolute contraindications to this approach, include the following:
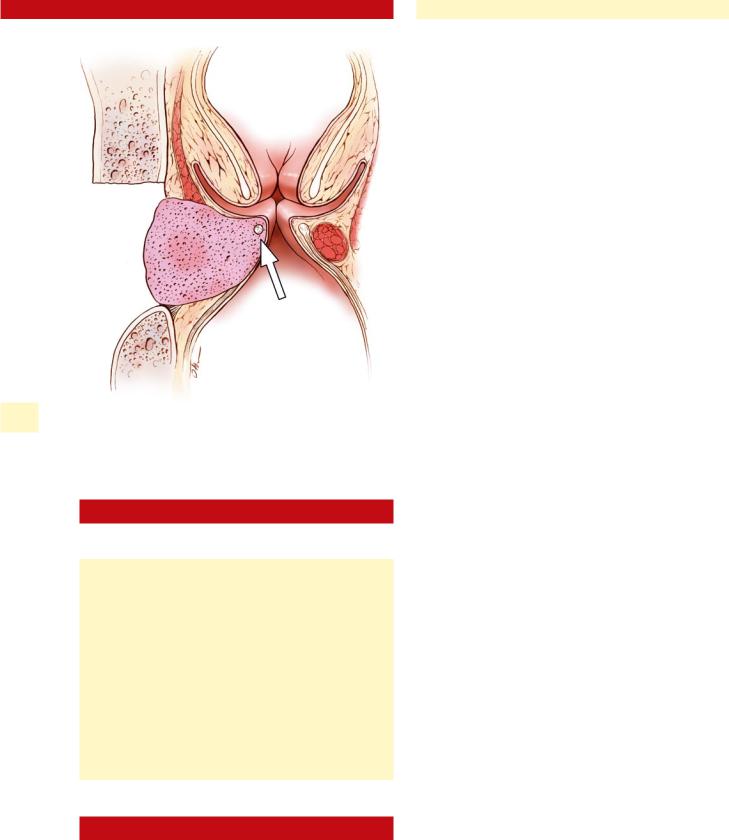
■Extensive granuloma infiltration along the medial edge of the vocal fold (vocal ligament involvement) (Fig. 42.2)
■Minimally symptomatic patient
■These clinical settings may be better suited for endoscopic treatment (see Chap. 24)
Fig. 42.1 Coronal section of larynx with Teflon granuloma sparing the vocal fold mucosa and vocal ligament (arrow)
268 |
Translaryngeal Removal of Teflon Granuloma |
42
Fig. 42.2 Coronal section of the larynx with Teflon granuloma involving the free edge of the vocal fold (arrow). This is a relative contraindication for translaryngeal removal
42.4Surgical Equipment
Equipment includes:
■Netterville medialization tray (Medtronic ENT, Jacksonville, Fla.)
■Drill with 2- or 3-mm cutting burr
■Kerrison rongeurs tray (1- to 3-mm-sized tips)
■Medium-grade Silastic block (Medtronic ENT)
■4-0 monofilament suture, double-armed needle
■Ruler (15-mm section of plastic ruler at tip of hemostat)
■Flexible laryngoscope
■C-mount camera with videocart/monitor
■Overdrape for laryngoscope (1010)
■Local anesthetic (nasal and subcutaneous)
■High-power surgical loops (optional)
■Middle ear instrument tray
(especially a no. 2 House knife; optional)
42.5Surgical Procedure
This advanced framework technique requires experience with the techniques of ML and AA. The surgeon should be well versed in the techniques of Chaps. 38, “Silastic Medialization Laryngoplasty for Unilateral Vocal Fold Paralysis” and 40, “Arytenoid Adduction” before attempting this technique.
1.The surgical region is liberally infiltrated with 1% lidocaine with1:100,000 epinephrine, from the hyoid down to the cricoid cartilage, on the side of the intended surgery. Typically, 20–25 ml is used.
2.Four percent lidocaine and oxymetazoline nasal spray is applied to the most patent nasal cavity. Placement of an indwelling flexible laryngoscope, allows videomonitoring of the larynx during the entire surgical case. The visual feedback of the larynx is invaluable when performing this surgery.
3.After sterile prep of the neck and flexible laryngoscope placement, a horizontal incision is placed in a skin crease at the level of the cricothyroid membrane extending past the midline, in a cervical skin crease, typically 7–8 cm in length.
4.Subplatysmal flaps are raised to the hyoid superiorly and the upper portion of the cricoid below; retention hooks are used to secure the flaps out of the way.
5.A randomly pedicled flap is raised that is composed of the superficial layer of the deep cervical fascia covering the strap muscles, with its overlying fat. This flap is posteriorly based and has a wide base lateral to the omohyoid muscle (Fig. 42.3). The flap should be raised with cold dissection and bipolar cautery to avoid thermal damage. Once reflected, the flap is covered with moist gauze.
6.The midline raphae is divided between the strap muscles with cautery, exposing the thyroid lamina on the involved side.
7.A single-prong hook is placed under the thyroid notch, and the larynx is retracted to the side opposite the paralysis, bringing the entire hemilaryngeal cartilage into view.
8.A vertical parasagittal laryngotomy is performed 5–7 mm posterior to the midline on the ipsilateral side, using a 15 blade or a powered sagittal saw (Fig. 42.4).
9.The thyroid lamina is retracted laterally with hooks allowing for wide exposure of the paraglottic space (Fig. 42.5). Dissection of the granuloma can now proceed (Fig. 42.6). Identification of the correct plane of dissection between the granuloma and normal paraglottic tissue is frequently difficult; surgical loops may be helpful during this portion of the case. A variety of dissection tools may be employed; Jamison scissors, Freer, and Woodson elevators are useful for the gross dissection, while middle ear instruments (no. 2 House knife) can be used for dissection with surgical loops. The mucosa of the ventricle should be avoid anteriorly where is may be adherent to the granuloma. Care is taken to preserve the vocal ligament/conus elasticus and lamina propria, as their integrity has proven an important prognostic indicator of postoperative voice quality. The granuloma often encases most of the paraglottic laryngeal musculature (thyroarytenoid/vocalis, lateral cricoarytenoid), such that complete removal may result in an “empty” paraglottic space. Not infrequently, defects in the ventricular or subglottic mucosa may be created during dissection. These mucosal defects should not compromise the end result. In contrast, removal of the vocal fold mucosa and/or vocal ligament should be avoided as this has a detrimental effect on the voice result.

|
Chapter 42 |
269 |
Fig. 42.3 Posteriorly based fat flap is raised
Fig. 42.6 Dissection of granuloma from the paraglottic space
Fig. 42.4 Vertical laryngotomy is performed 5–7 mm off the midline for exposure of the paraglottic space
|
Fig. 42.7 After removal of the granuloma, the laryngotomy is repaired |
Fig. 42.5 Axial view of parasagittal laryngofissure |
with 2-0 Prolene sutures, and windows are made for medialization |
laryngoplasty and arytenoid adduction |
