
Учебники / Pediatric Sinusitis and Sinus Surgery Younis 2006
.pdfPathophysiology and Etiology of Pediatric Rhinosinusitis |
25 |
antibiotic use in children aged 1 to 12 years (48). Complete or near-complete resolution of symptoms was reported in 58% of the children, some improvement in 21%, and minimal or no improvement in 21%. Other studies support the role of adenoidectomy as beneficial in the treatment of rhinosinusitis in the pediatric population (49–52).
Environmental Factors
Environmental factors, including pollutants, irritants, toxicants, and passive cigarette smoke, may cause local irritation or inflammation. Resultant cellular damage may initiate an inflammatory cascade including the release of mediators, attraction of inflammatory cells to the area, and local edema. This could lead to mucosal swelling, decreased airflow, and possible OMC obstruction with subsequent development of rhinosinusitis. Preexisting conditions such as allergic or vasomotor rhinitis may exacerbate the effects of environmental factors.
Environmental factors may also lead to ciliary dysfunction. Aguis et al. found that after in vitro exposure of nasal ciliated cells from nonsmokers to cotinine, a major metabolite of nicotine, there was a significant drop in ciliary beat frequency compared with non-exposed ciliated cells (53). They concluded that cotinine has a marked effect on ciliary function in vitro. Secondhand smoke exposure may thus lead to diminished mucociliary clearance in children and subsequently to rhinosinusitis.
Dubin et al. examined the effect of passive tobacco smoke exposure on eustachian tube function in rats (54). There was a significant alteration in ciliary function and mucociliary clearance time within the eustachian tube. Bascom et al. reported similar results (55). In summary, environmental factors have been shown to affect ciliary function and mucociliary clearance and are likely to be etiologically important in pediatric rhinosinusitis.
CONCLUSION
The management of pediatric rhinosinusitis relies on a clear understanding of the pathophysiology and etiology of the underlying disease process. Any condition that affects the patency of the ostia, the mucociliary clearance mechanism, or the consistency and makeup of the secretions predisposes to rhinosinusitis. Our understanding of the role of comorbidities such as allergic disease, immune deficiencies, and GERD in contributing to pediatric rhinosinusitis continues to increase. Finally, the role of environmental pollutants and particularly of secondhand smoke exposure is increasingly recognized as a cause of rhinosinusitis in children.
26 |
Hertler et al. |
REFERENCES
1.Lusk RP, Stankiewicz JA. Pediatric rhinosinusitis. Otolaryngol Head Neck Surg 1997; 3(2):S53–S57.
2.Hopp R, Cooperstock M. Medical management of sinusitis in pediatric patients. Curr Probl Pediatr 1997; 25(7):178–186.
3.Wald ER. Sinusitis in infants and children. Ann Otol Rhinol Laryngol 1992; 101(1):37–42.
4.Kaliner MA, Osguthorpe JD, Fireman P, Anon J, Georgitis J, Davis ML, Naclerio R, Kennedy D. Sinusitis: bench to bedside: current findings, future directions. Otolaryngol Head Neck Surg 1997; 116(6):S1–S20.
5.Gungor A, Corey JP. Pediatric sinusitis: a literature review with emphasis on the role of allergy. Otolaryngol Head Neck Surg 1997; 116(1):4–15.
6.Ott NL, O’Connell EJ, Hoffmans AD, Beatty CW, Sachs MI. Childhood sinusitis. Mayo Clinic Proc 1991; 66:1239–1247.
7.Braverman I, Wright ED, Wang CG, Eidelman D, Frenkiel S. Human ciliary beat-frequency in normal and chronic sinusitis subjects. J Otolaryngol 1998; 27(3):145–152.
8.Subauste MC, Jacoby DB, Richards SM, Proud D. Infection of a human respiratory epithelial cell line with rhinovirus: induction of cytokine release and modulation of susceptibility to infection by cytokine exposure. J Clin Invest 1995; 96:549–557.
9.Noah TL, Becker S. Respiratory syncytial virus-induced cytokine production by a human bronchial epithelial cell line. Am J Physiol 1993; 265(5 Pt 1):L472–L478.
10.Elias JA, Zheng T, Einarsson O, Landry M, Trow T, Rebert N, Panuska J. Epithelial interleukin-11: regulation by cytokines, respiratory syncytial virus, and retinoic acid. J Biol Chem 1994; 269:22261–22268.
11.Lundberg JO, Farkas-Szallasi T, Weitzberg E, Rinder J, Lidholm J, Anggaard A, Hokfelt T, Lundberg JM, Alving K. High nitric oxide in human paranasal sinuses. Nat Med 1995; 1:370–373.
12.Jain B, Rubenstein I, Robbins RA, Leishe KL, Sisson JH. Modulation of airway epithelial cell ciliary beat frequency by nitric oxide. Biochem Biophys Res Commun 1993; 191:83–88.
13.Shapiro GG, Rachelevsky GS. Introduction and definition of sinusitis. J All Clin Immunol 1992; 90:417–418.
14.Pelikan Z, Pelikan-Filipek M. Role of nasal allergy in chronic sinusitis maxillaries-diagnostic value of nasal challenge with allergen (NPT). J All Clin Immunol 1990; 86:484–491.
15.Shapiro GG, Virant FS, Furukawa CT, Pierson WE, Bierman CW. Immunologic defects in patient with refractory sinusitis. Pediatrics 1991; 87:311–316.
16.Lazar RL, Younis RT, Gross CW. Pediatric functional endonasal sinus surgery: review of 210 cases. Head Neck 1992; 14(2):92–98.
17.Hisamatsu K, Ganbo T, Nakazawa T, Murakami Y, Gleich GJ, Makiyama K, Koyama H. Cytotoxicity of human eosinophil granule major basic protein to human nasal sinus mucosa in vitro. J All Clin Immunol 1990; 86:52–63.
18.Nguyen KL, Corbett ML, Garcia DP, Eberly SM, Massey EN, Le HT, Shearer LT, Karibo JM, Pence HL. Chronic sinusitis among pediatric patients with chronic respiratory complaints. J All Clin Immunol 1993; 92(6):824–830.
Pathophysiology and Etiology of Pediatric Rhinosinusitis |
27 |
19.Manning SC, Wasserman RL, Silver R, Phillips DL. Results of endoscopic sinus surgery in pediatric patients with chronic sinusitis and asthma. Arch Otolaryngol Head Neck Surg 1994; 120(10):1142–1145.
20.Palmer JN, Conley DB, Dong RG, Ditto AM, Yarnold PR, Kern RC. Efficacy of endoscopic sinus surgery in the management of patients with asthma and chronic sinusitis. Am J Rhinol 2001; 15(1):49–53.
21.Rosenstein BJ, Cuting GR. The diagnosis of cystic fibrosis. J Pediatr 1998; 132:689–695.
22.Nishioka GJ, Cook PJ. Paranasal sinus disease in patients with cystic fibrosis. Otolaryngol Clin North Am 1996; 29(1):193–205.
23.Cuyler JP, Monaghan AJ. Cystic fibrosis and sinusitis. J Otolaryngol 1989; 18(4):173–175.
24.Gentile VG, Isaacson G. Patterns of sinusitis in cystic fibrosis. Larygnoscope 1996; 106:1005–1009.
25.Jones JW, Parsons DS, Cuyler JP. The results of functional endoscopic sinus surgery on the symptoms of patients with cystic fibrosis. Int J Pediatr Otorhinolaryngol 1993; 28:25–32.
26.Triglia J-M, Nicollas R. Nasal and sinus polyposis in children. Laryngoscope 1997; 107(7):963–966.
27.Jaffe BF, Strome M, Khaw KT, Shwachman H. Nasal polypectomy and sinus surgery for cystic fibrosis—a 10 years review. Oto Clin North Am 1977; 10: 81–90.
28.Crockett DM, McGill TJ, Healy GB, Friedman EM, Salkeld LJ. Nasal and paranasal sinus surgery in children with cystic fibrosis. Ann Otol Rhinol Laryngol 1987; 96(4):367–372.
29.Cepero R, Smith RJ, Catlin FI, Bressler KL, Furuta GT, Shandera KC. Cystic fibrosis: an otolaryngologic perspective. Otolaryngol Head Neck Surg 1987; 97(4):356–360.
30.Polmar SH. The role of the immunologist in sinus disease. J All Clin Immunol 1992; 90(3 Pt 2):511–515.
31.Shapiro GG, Virant FS, Furukawa CT, Pierson WE, Bierman CW. Immunologic defects in patients with refractory sinusitis. Pediatrics 1991; 87(3): 311–316.
32.Umetsu DT, Ambrosino DM, Quinti I, Siber GR, Geha RS. Recurrent sinopulmonary intection and impaired antibody response to bacterial capsular polysaccharide antigen in children with selective IgG-subclass deficiency. N Eng J Med 1985; 313(20):1247–1251.
33.Ambrosino DM, Umetsu DT, Siber GR, Howie G, Goularte TA, Michaels R, Martin P, Schur PH, Noyes J, Schiffman G. Selective defect in the antibody response to H. influenzae type b in children with recurrent infections and normal serum IgG subclass levels. J All Clin Immunol 1988; 81(6):1175–1179.
34.Teknos TN, Metson R, Chasse T, Balercia G, Dickersin GR. New developments in the diagnosis of Kartagener’s syndrome. Otolaryngol Head Neck Surg 1997; 116(1):68–74.
35.Chapelin C, Coste A, Reinert P, Boucherat M, Millepied MC, Poron F, Escudier E. Incidence of primary ciliary dyskinesia in children with recurrent respiratory diseases. Ann Otol Rhinol Laryngol 1997; 106(10 Pt 1):854–858.
28 |
Hertler et al. |
36.Phipps CD, Wood E, Gibson WS, Cochran WJ. Gastroesophageal reflux contributing to chronic sinus disease in children. Arch Otolaryngol Head Neck Surg 2000; 126(7):831–836.
37.Contencin P, Narcy P. Nasopharyngeal monitoring in infants and children with chronic rhinopharyngitis. Int J Pediatr Otorhinolaryngol 1991; 22:249–256.
38.Burton DM, Pransky SM, Katz RM, Kearns DB, Seid AB. Pediatric airway manifestations of gastroesophageal reflux. Ann Otol Rhinol Laryngol 1992; 101:742–749.
39.Contencin P, Maurage C, Ployet MJ, Seid AB, Sinaasappel M. Gastroesophageal reflux and ENT disorders in childhood. Int J Pediatr Otorhinolaryngol 1995; 32(Suppl):S135–S144.
40.Beste DJ, Conley SF, Brown CW. Gastroesophageal relux complicating choanal atresia repair. Int J Pediatr Otorhinolaryngol 1994; 29:51–58.
41.Bothwell MR, Parsons DS, Talbot A, Barbero G, Wilder B. Outcome of reflux therapy on pediatric chronic sinusitis. Otolaryngol Head Neck Surg 1999; 121:255–262.
42.Wald ER, Dashefsky B, Byers C, Guerra N, Taylor F. Frequency and severity of infections in day care. J Pediatrics 1988; 112(4):540–546.
43.Wald ER, Guerra N, Byers C. Frequency and severity of infections in day care: three-year follow-up. J Pediatr 1991; 118(4):509–514.
44.Goldsmith AJ, Rosenfeld RM. Treatment of pediatric sinusitis. Pediatr Clin North Am 2003; 50(2):413–426.
45.Jones NS, Strobl A, Holland I. CT findings in 100 patients with rhinosinusitis and 100 controls. Clin Otolaryngol 1997; 22:47–51.
46.Wilner A, Choi SS, Vezina LG, Lazar RH. Intranasal anatomic variations in pediatric sinusitis. Am J Rhinol 1997; 11(5):355–360.
47.Takahashi H, Honjo I, Fujita A, Kurata K. Effects of adenoidectomy on sinusitis. Acta Oto-Rhino-Laryngol Belgica 1997; 51(2):85–87.
48.Vandenberg SJ, Heatley DG. Efficacy of adenoidectomy in relieving symptoms of chronic sinusitis in children. Arch Otolaryngol Head Neck Surg 1997; 123: 675–678.
49.Lusk RP. Surgical modalities other than ethmoidectomy. J All Clin Immunol 1992; 90:538–542.
50.Fujita A, Takahashi H, Honjo I. Etiological role of adenoids upon otitis media with effusion. Acta Otolaryngol Suppl 1988; 454:210–213.
51.Paul D. Sinus infection and adenotonsillitis in pediatric patients. Laryngoscope 1981; 91(6):997–1000.
52.Merck W. Relationship between adenoidal enlargement and maxillary sinusitis. HNO 1974; 6:198–199.
53.Aguis AM, Wake M, Pahor AL, Smallman A. The effects of in vitro cotitine on nasal ciliary beat frequency. Clin Otolaryngol All Sci 1995; 20(5):465–469.
54.Dubin MG, Pollock HW, Ebert CS, Berg E, Buenting JE, Prazma JP. Eustachian tube dysfunction after tobacco smoke exposure. Otolaryngol Head Neck Surg 2002; 126(1):14–19.
55.Bascom R, Kesavanathan J, Fitzgerald TK, Cheng KH, Swift DL. Sidestream tobacco smoke exposure acutely alters human nasal mucociliary clearance. Environ Health Perspectives 1995; 103(11):1026–1030.

3
Diagnostic Workup for
Pediatric Rhinosinusitis
Edward Hepworth
Division of Otolaryngology–Head and Neck Surgery, University of New Mexico,
Albuquerque, New Mexico, U.S.A.
Ron B. Mitchell
Department of Otolaryngology, Virginia Commonwealth University,
Richmond, Virginia, U.S.A.
INTRODUCTION
The workup and treatment of rhinosinusitis in children is usually multidisciplinary. Recent advances in endoscopy and imaging techniques and in pharmacotherapy continue to improve the overall well-being of children with sinus disease. Research to date has focused mostly on antimicrobial therapy, criteria for disease classification, and improved techniques in operative management in adults. Sinus disease in children differs significantly from that seen in adults. Children with sinus disease have multiple factors that influence the presentation and the progression of the disease and these factors may be congenital, immunologic, or environmental. In addition, the initial symptoms, clinical findings, and radiological manifestations are quite different in children than in adults.
Epidemiology as it Relates to Disease Workup
The true prevalence of rhinosinusitis in children is unknown, but it has been estimated to be approximately 7% (1). Rhinosinusitis is the fifth most
29

30 |
Hepworth and Mitchell |
common diagnosis resulting in an antibiotic prescription. The direct medical cost to treat rhinosinusitis in children exceeds $2.4 billion annually in the United States (2).
Definitions
Acute bacterial rhinosinusitis has been defined as an infection of the sinuses lasting not more than 30 days and concluding in complete resolution (3). Subacute disease persists for 30 to 90 days with complete resolution. Recurrent acute disease consists of multiple acute episodes separated by symptomfree intervals of at least 10 days, or alternatively three acute episodes in six months or four acute episodes in one year. Chronic bacterial rhinosinusitis persists for more than 90 days. Acute rhinosinusitis superimposed on chronic disease occurs when patients with chronic rhinosinusitis acquire new symptoms that resolve within 30 days of treatment. The underlying residual symptoms attributed to chronic rhinosinusitis persist in these patients.
DEVELOPMENTAL ANATOMY AS RELEVANT TO
DISEASE WORKUP
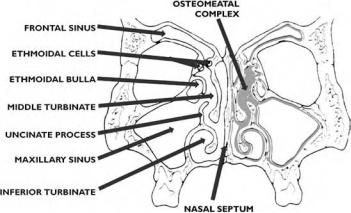
The embryologic development of the sinuses is summarized in Table 1. Certain key points regarding sinus cavity growth are germane to clinical, radiologic, and laboratory workup. The clinician must identify the child’s status along the continuum of sinus development in order to adequately assess and treat the disease. The ostiomeatal complex (OMC) is present in nearly full
Table 1 Paranasal Sinus Development
Age |
Development milestone |
|
|
|
|
Birth |
Maxillary sinus cavity present and partially aerated |
|
|
|
Ethmoidal cells present |
|
|
Sphenoidal and frontal sinus cavities absent |
4 months |
Frontal evaginations from anterior ethmoid cells |
|
|
|
visible microscopically |
5 |
months |
Maxillary sinus cavity visible radiographically |
6 months |
Ethmoidal cell septae visible radiographically |
|
1 |
year |
Frontal evagination evident in cadaveric dissection |
3 |
years |
Appreciable aeration of the frontal sinus in cadaveric |
|
|
specimens |
6 |
years |
Frontal aeration evident radiographically |
7 years |
Pneumatization of the sphenoid as far posteriorly |
|
|
|
as the sella turcica |
10 years |
Frontal disease becomes clinically significant |
|
20 years |
Complete pansinus aeration |
|
|
|
|
Diagnostic Workup for Pediatric Rhinosinusitis |
31 |
Figure 1 OMC in an infant.
complexity in the infant, although it continues to grow in size and change its orientation and topography throughout adolescence (Fig. 1). An image of the OMC in a one-year-old child is shown in Figure 2.
The assumption that immature or pathologically undersized sinus cavities are impervious to disease is, however, questionable. Suzuki et al. (4) demonstrated that patients with cleft lip and palate have significantly smaller sinus cavities than normal and are more prone to chronic sinus disease. Several authors have also described frontal mucocele development following pediatric trauma at a young age where frontal sinus development had been minimal (5,6).
Figure 2 An image of OMC in a one-year-old child.
32 |
Hepworth and Mitchell |
Several other factors related to the development of the sinuses are relevant to disease workup. These include the status of the foramen cecum; the status of the palate, lip, and alveolus; and the completion of closure of the nasal roof. Defects in any of these areas may result in conditions masquerading as, or contributing to, sinus disease. The presence of any of these defects should initiate a multidisciplinary workup rather than symptomatic management of sinonasal complaints. Evaluation of the intactness of the anterior skull base is best performed with computed tomography (CT) scan. Many of the midline nasal masses contribute to obstruction, inflammation, and chronic sinonasal complaints. These are often best evaluated by magnetic resonance imaging (MRI).
DISEASE HISTORY
A comprehensive medical history is essential for the diagnosis of sinus disease in children. This medical history serves a number of purposes. First, a diagnosis is obtained. Second, a reference point for monitoring treatment progress is established. Finally, a document is created that summarizes all relevant data for fellow healthcare providers in a standardized format. Children are often unable to articulate the symptoms of rhinosinusitis. Caregivers must provide information about congenital, genetic, and environmental factors that may influence treatment and outcome.
In fact, family circumstances may assume more importance than many aspects of disease pathology. For instance, time off from work, eligibility for day care while ill, and frequency of physician visits may prompt treatment decisions more than a change in symptoms. Ideally, treatment should address quality of life for all family members. Many providers rely on standardized questionnaires to avoid overlooking important details in this regard (7).
Chief Complaint
The chief presenting complaint of a child or caregiver may include:
frequent anterior or posterior nasal drainage
daytime cough
nasal congestion
low-grade fever
ear pain or fullness
irritability
headache
halitosis
behavior problems
learning problems
poor growth or failure to thrive
snoring
Diagnostic Workup for Pediatric Rhinosinusitis |
33 |
frequent snorting
cyclic vomiting (8)
anorexia nervosa (9)
chronic fatigue (10)
More severe cases of sinus disease may present as purulent rhinorrhea, a high fever, or periorbital edema. Nighttime cough is more prevalent in chronic than acute rhinosinusitis. A systematic approach to the documentation of presenting complaints will help to guide treatment, but more importantly, to provide a means for monitoring treatment and maintaining patient/caregiver rapport. This should include the following:
1.age at onset
2.severity
3.associated symptoms
4.alleviating factors
5.aggravating factors
6.any variation in the degree of severity or pattern of the complaint
7.a description of the nature of the complaint, for instance, burning, sharp or dull pain
History of Illness, Past Medical History, and Risk
Factor Assessment
The past medical history should focus on those factors that are treatable or may require otolaryngologic intervention. Occult genetic disorders, correctable lifestyle factors, systemic disease, and risk prevention are all requisite elements of the workup.
Important elements of the past medical history address patient quality of life. Quality of life factors such as time lost from school due to illness, sleep disturbance, interference with daily activity, lack of attention at school or home, and medication side effects are important elements to include in the evaluation of sinus disease. Equally important to document are the previous treatment regimens and response to treatment, including:
1.antihistamines, noting which were effective and any side effects
2.decongestants and route of delivery
3.other nasal sprays—saline, corticosteroids, or anticholinergics
4.asthma medications—oral or inhaled
5.antibiotics, type including length and number of courses
6.previous emergency room/hospital treatment
Inquiry into ear infections is important. About 50% of children with otitis media will ultimately be diagnosed with allergic or infectious sinonasal disease (11). Food sensitivities, drug hypersensitivity, insect sting allergy, eczema, asthma, urticaria or angioedema, and contact sensitivity or
34 |
Hepworth and Mitchell |
dermatitis are all conditions that indicate systemic atopy and tendency toward sinonasal disease (12). Sinonasal disease is often familial, manifesting in one or both parents, or a sibling. This is particularly true with chronic rhinosinusitis (13). More importantly, high-density occurrence of sinus disease in a family may be the initial indicator of a more serious inherited disorder, as discussed below.
Inhalant allergies are becoming better understood as a major contributor to pediatric rhinosinusitis (14). Atopic conditions are perhaps the most common cause of mucosal edema in the sinonasal spaces and are largely influenced by the child’s family and social environment. About 80% of children undergoing sinus surgery have a positive skin test response to inhalant allergens (12). Many children will not have classic allergy symptoms but may have enough disease manifestation to alter normal nasal function (15). Investigation into an allergic environment should include:
1.type of family dwelling: single or multiple, apartment or home
2.type of heating system: forced air, baseboard, or wood stove
3.type of cooling system: air conditioning, evaporative cooling
4.bedroom: frequency of cleaning, bedding changes, other issues related to hygiene, presence of stuffed animals or dolls (a child spends up to 12 hours daily there)
5.flooring: linoleum, carpeting, or hard wood
6.bedding: conventional mattress or waterbed, hollow-fiber-filled or feather pillow
7.pets: outdoor or indoor and access into bedroom areas
8.other: presence of molds or dampness; use of a humidifier, electrostatic or HEPA filters; and exposure to secondhand smoking
Related Disorder Assessment
Several disease conditions are relevant to both the history and the subsequent laboratory investigation of pediatric rhinosinusitis patients. These are discussed individually.
Cystic Fibrosis and Genetic Disorders
Cystic fibrosis is a disorder in which a transmembrane conductance regulator is defective. Related symptoms and disease states include congenital bilateral absence of the vas deferens, allergic bronchopulmonary aspergillosis, chronic pulmonary infection, and isolated chronic pancreatitis (16). Most patients with cystic fibrosis present to the otolaryngologist for focused workup and treatment often to include surgery for nasal polyposis. Chronic rhinosinusitis in the very young, especially when associated with multiple infections of the ear, nose, and throat, should prompt concern about undiagnosed cystic fibrosis (16).
