
Учебники / Otolaryngology - Basic Science and Clinical Review
.pdf
THE ACOUSTICS AND MECHANICS OF DISEASED MIDDLE EARS 269
A
Figure 21-11 Comparisons of audiometric measurements of hearing function after ossicular disruptions and estimates of hearing function based on measurements of acoustic coupling. (After Peake et al, 1992.) (A) Mean of eight audiograms from patients with surgically confirmed incudostapedial disarticulation, and measurements
coupling suggests that stimuli reaching the inner ear through bone conduction mechanisms in this particular condition are small enough to be ignored. This conclusion is supported by other measurements of hearing function in cases where the ossicular route is greatly reduced.
LOSS OF THE TYMPANIC MEMBRANE,
MALLEUS, AND INCUS
Loss of the TM, malleus, and incus abolishes ossicular coupling and leads to an enhancement of acoustic coupling of 10–20 dB as compared with the normal ear (Peake et al, 1992). This enhancement results from the loss of the shielding effect of the TM, which in the normal ear attenuates the middle ear sound pressure by 10 to 20 dB relative to the ear canal sound pressure. Therefore, for the missing TM, malleus, and incus condition, the predicted air–bone gap is 40 to 50 dB. The predicted gap is similar to that measured in patients. Fig. 21-11B shows the mean air–bone gap from five cases with total loss of the TM, malleus, and incus). The increase in acoustic coupling due to loss of TM shielding also explains why the hearing of a patient with an interrupted ossicular chain and an intact TM is improved by 10 to 20 dB with the creation of a perforation in the TM.
B
of ossicular coupling of Békésy (1960). (B) Mean of five audiograms from ears with no tympanic membrane, malleus, or incus (Békésy, 1960) and the acoustic coupling estimates for ears with no tympanic membrane (Peake et al, 1992). IS, incudostapedial; TM, tympanic membrane.
OSSICULAR FIXATION
Fixation of the stapes footplate due to otosclerosis results in a conductive hearing loss that can range from 5 to 50 dB. Otosclerotic changes in the annular ligament and fixation of the stapes reduce ossicular coupling by hindering stapes motion, resulting in a conductive hearing loss. The amount of loss depends on the degree of decreased stapes motion. For low frequencies, where the stiffness of the annular ligament is a major constraint on the ossicular route in the normal ear, even a small increase in ligament stiffness will produce a measurable conductive loss that is consistent with the initial appearance of a low-frequency hearing loss in otosclerosis.
In contrast, the conductive hearing loss associated with so-called malleus fixation is only 15 to 25 dB. Malleus fixation is generally the result of a bony spur that extends from the epitympanic wall to the malleus head. Because the point of fixation lies near the axis of rotation of the malleus, and because this spur attaches to the malleus head only over a relatively small surface area, it is likely that true “fixation” of the malleus does not occur and some sound is still transmitted across the incudomalleal joint. Hence, so-called malleus fixation leads to a reduction in ossicular coupling, which is consistent with the 15 to 25 dB conductive losses that are observed clinically.

270 CHAPTER 21 ACOUSTICS AND MIDDLE EAR MECHANICS FOR OTOLARYNGOLOGY
TYMPANIC MEMBRANE PERFORATION
Perforations of the TM cause a conductive hearing loss that can range from negligible to 50 dB. The primary mechanism of the air–bone gap due to a perforation is a reduction in ossicular coupling that is caused by a loss in pressure difference across the TM, and the magnitude of the gap is proportional to the degree of reduction in ossicular coupling (Voss, 1998).The perforation-induced loss in ossicular coupling is generally greater at lower frequencies and greater with larger perforations. The perforation also leads to an increase in acoustic coupling by 10 20 dB, because of loss of the shielding effect of the intact TM. The increase in acoustic coupling allows one to predict that the maximum conductive loss from a perforation will be no more than 40 to 50 dB, which is consistent with clinical observations.
MIDDLE EAR EFFUSION
Fluid in the middle ear, a primary feature of otitis media with effusion (OME), is associated with a conductive hearing loss of up to 30 to 35 dB, though the degree and frequency dependence of individual losses can vary. The conductive loss occurs because of reduction in ossicular coupling due to several mechanisms. At high frequencies 1 kHz, hearing loss is caused primarily by mass loading of the TM by fluid, with decreases in
A
Figure 21-12 (A) A schematic of a type IV tympanoplasty. PEC, POW , and PRW denote the sound pressures in the ear canal, outside the oval window and outside the round window. US is the volume velocity of the stapes. (B) A comparison of the mean of the five best hearing
sound transmission of up to 20 to 30 dB. The effect increases as more of the TM is covered with fluid. At low frequencies 1 kHz, hearing loss is due to an increase in impedance of the middle ear air space (resulting from reduced middle ear air volume) and negative middle ear static pressure (which is often associated with OME). It appears that viscosity of the fluid does not significantly influence middle ear sound transmission in OME.
THE ACOUSTICS AND MECHANICS OF RECONSTRUCTED MIDDLE EARS
TYMPANOPLASTY TECHNIQUES WITHOUT
OSSICULAR LINKAGE: TYPES IV AND V
When the TM and ossicles are missing and there is a canal wall-down mastoid cavity, a type IV tympanoplasty is a surgical option. Incoming sound from the ear canal is allowed to impinge directly onto the stapes footplate, while the round window is shielded by a tissue graft such as temporalis fascia (Fig. 21-12A). If the stapes footplate is ankylosed, it is removed and replaced by a fat graft, and this arrangement constitutes a type V tympanoplasty. In both type IV and type V procedures, there is no ossicular coupling, and residual hearing depends solely on acoustic coupling (Peake et al, 1992.The introduction of a tissue graft to acoustically
B
results of Wullstein (1960) after type IV tympanoplasty and predictions based on the loss of ossicular coupling and the enhancement in acoustic coupling produced by the graft shield. (After Merchant et al, 1998.)

THE ACOUSTICS AND MECHANICS OF RECONSTRUCTED MIDDLE EARS 271
shield the round window enhances acoustic coupling. Under optimal conditions, one can achieve “maximum” acoustic coupling, and one would predict an air–bone gap of only 20 dB.This prediction is consistent with the best type IV hearing results observed clinically (Fig. 21-12B). The optimal conditions required to maximize acoustic coupling include normal footplate mobility, a sufficiently stiff acoustic shield, and aeration of the round window niche (Merchant et al, 1995; Peake et al, 1992). In clinical practice, the surgeon should
(1) preserve normal stapes mobility by preferably covering the footplate with a very thin split thickness skin graft, not a fascia graft; (2) reinforce a fascia shield with cartilage or Silastic, 1 mm thick; (3) create conditions that promote aeration of the round window niche; and
(4) preserve mobility of the round window membrane. The interposition of a graft to acoustically shield the round window in a type IV or typeV tympanoplasty primarily reduces the magnitude of the sound pressure at the round window. Under these circumstances, acoustic coupling (i.e., the difference in sound pressures at the oval and round window) is relatively insensitive to the phase difference between the two pressures (Merchant et al, 1998). In other words, the difference in magnitude between the oval and round window pressures is more important than the difference in phase in determining
the effective cochlear input.
TYMPANOPLASTY TECHNIQUES WITH
PRESERVATION OF OSSICULAR LINKAGE:
TYPES I, II, AND III
Types I, II, and III tympanoplasty involve reconstruction of the TM and/or the ossicular chain. The final hearing results depend on three factors: the efficacy of the reconstructed TM, the efficacy of the reconstructed ossicular chain, and the adequacy of middle ear aeration and its static pressure.At the present time, our knowledge of the mechanics of these three factors is incomplete, and much work remains to be done.
Tympanic Membrane Reconstruction
The TM is the major transducer of the middle ear. Motion of the normal TM is complex (Khanna and Tonndorf, 1972).At frequencies below 1000 Hz, the entire TM moves in-phase, but the magnitude of motion varies with location. At higher frequencies, different parts of the TM move with varying magnitudes and phases. Clinical observations suggest that those surgical techniques that tend to restore or preserve the normal anatomy of the drum can lead to good hearing results. However, the acoustical and mechanical properties of
reconstructed TMs are not well understood at the present time, and more research is needed. For example, (1) little is known of the mechanical significance of the arrangements of structural fibers in the TM; (2) although it has been argued that the conical shape of the normal tympanic membrane plays a role in middle ear function, the possible effects of changes in TM shape on middle ear function are not understood; and (3) although many existing models of TM function have been shown to fit some of the available data (e.g., Funnell and Decraemer, 1996), there are wide differences in the structure of these models, and little effort has been made to compare their significant similarities and differences.
Ossicular Reconstruction
Ossiculoplasty is required in 40 to 90% of all tympanoplasties. A wide variety of ossicular grafts and prostheses are in use. Currently, there are few scientific data on the precise structure–function relationship concerning their acoustical properties. Factors that can influence the acoustic performance of an ossicular prosthesis include its stiffness, mass, position, tension, and coupling (Merchant et al, 1998). In general, the stiffness of a prosthesis will not be a significant factor as long as the stiffness is much greater than that of the stapescochlear impedance. For clinical purposes, prostheses made of ossicles, cortical bone, and most synthetic materials generally meet this requirement.
Analysis of a middle ear model suggests that an increase in ossicular mass should not cause significant detriment in sound transmission. Increases in the mass of a prosthesis up to 16 times that of the stapes mass (which is 3 mg) were predicted to produce 10 dB air–bone gaps and only at frequencies above 1 kHz. Using a temporal bone preparation, it has been reported that a mass of 5 mg added to the stapes head led to a 13 to 15 dB loss at high frequencies (Goode and Nishihara, 1994). Thus the acoustic effects of mass of an ossicular strut need to be clarified. Measurements in a human temporal bone preparation have suggested that the angle between the stapes and a prosthesis should be 45 degrees for optimal sound transmission. Although it is ideal to attach a prosthesis to the manubrium, temporal bone data (Goode and Nishihara, 1994) have shown that acceptable results can occur with a prosthesis placed against the posterosuperior quadrant of the TM as long as 3 to 4 mm of the diameter of the prosthesis contacts the TM.
Tension and length are critical in determining the hearing result.The mechanical impedance of biological

272 CHAPTER 21 ACOUSTICS AND MIDDLE EAR MECHANICS FOR OTOLARYNGOLOGY
structures is inherently nonlinear, and measurements (e.g., tympanometry) have shown that the TM and the annular ligament act as linear elements only over the range of small motions ( 10 m) associated with physiological sound levels. The larger displacements produced by a prosthesis that is too long will produce a stiffening of the annular ligament and TM, resulting in excessive tension, and hence, a poor hearing result.
Coupling refers to how well a prosthesis “adheres” to the footplate or TM, and the degree of coupling will determine whether or not there is slippage in sound transmission at the end of a prosthesis. Thus a prosthesis will transmit sound effectively only if there is “good” coupling at both ends. Clinical observations indicate that it is rare to obtain a firm union between a total ossicular replacement prosthesis (TORP) and the stapes footplate, and hence, inadequate coupling at the TORP–footplate joint may be an important cause of a persistent postoperative air–bone gap. The physical factors that control coupling have not been determined in a quantitative manner, and further study of this parameter is warranted.
Middle Ear Aeration and Static Pressure
An important parameter for the success of tympanoplasty is the presence of an aerated middle ear. Aeration allows the TM graft, the ossicles, and the round window to move. Nonaerated ears have large 45 to 60 dB air–bone gaps, whereas in an adequately aerated ear, the size of the air–bone gap is directly proportional to the efficiency of the TM and ossicles. How much air is necessary behind the TM (i.e., within the middle ear and mastoid)? Model analyses of the effects of varying the volume of the middle ear and mastoid predict an increasing low-frequency hearing loss as volume is reduced.The normal, average volume of the middle ear and mastoid is 6 cc; a combined middle ear and mastoid volume of 0.5 cc was predicted to result in a 10 dB conductive loss.Volumes smaller than 0.5 cc were predicted to lead to progressively larger gaps, whereas volumes greater than 1.0 cc were predicted to provide little additional acoustic benefit. Experimental studies in our laboratory using a human temporal bone preparation where the middle ear and mastoid volume was reduced progressively have shown results consistent with the model prediction. Another parameter that can influence middle ear sound transmission is the static air pressure in the middle ear space. Experiments in a human temporal bone preparation have demonstrated that middle ear static pressure can have different effects on sound transmission at different frequencies (Murakami et al, 1997).The mechanisms and
structural alterations by which pressure changes reduce middle ear sound transmission are not well defined, and possible sites of pressure sensitivity include the TM, the annular ligament, the incudomalleal joint, and the suspensory ligaments of the ossicles. Some of these physical structures are drastically altered as a result of tympanoplasty, and the acoustic effects of negative and positive middle ear static pressure in such ears need to be characterized.
CANAL WALL-UP VERSUS CANAL
WALL-DOWN MASTOIDECTOMY
A canal wall-down mastoidectomy poses several considerations from an acoustical and mechanical perspective (when compared with a canal wall-up procedure): First, the canal wall-down procedure results in a significant reduction in the size of the residual middle ear air space. However, as long as this air space is greater than 0.4 cc, the acoustical effect of loss of sound transmission should be less than 10 dB. Second, a canal wall-down procedure results in the creation of a large air space lateral to the TM (i.e., the air space within the mastoid bowl including the external auditory canal). This mastoid bowl and ear canal air space generates resonances that can influence middle ear sound transmission favorably or unfavorably. For example, Goode et al (1977) described a patient with a 4.1 cc radical mastoid cavity that had a 25 to 30 dB resonance for frequencies between 2500 and 4000 Hz, in whom these resonances were felt to contribute to the patient’s good hearing at these higher frequencies. However, the structure–function relationships between the size and shape of the normal and modified mastoid cavity and cavity resonances have not been well defined. An improved understanding of this issue should help to develop guidelines for an otologic surgeon to configure mastoid cavities in ways that could be acoustically beneficial. Third, after a canal wall-down procedure, the TM graft comes to lie in a more medial position compared with normal, and the TM graft is made to couple to the stapes head or to a prosthesis such as aTORP.The mechanics of such aTM graft and its coupling to the stapes/TORP are likely to be different from normal and need to be characterized. For example, when placed against the stapes head, such a graft is often in contact with the promontory and tympanic segment of the facial canal; such contact may limit the functional surface area of the graft. When a TORP is considered, if the top of the TORP rises much above the level of the oval window niche, the TORP tends to extrude; if the TORP is kept low, the prosthesis often settles against the margins of the niche.

SUMMARY 273
STAPEDOTOMY
The output of the middle ear can be quantified by the volume velocity of the stapes, where this volume velocity is equal to the stapes linear velocity multiplied by the area of the stapes footplate. After a stapedotomy, the effective area of the footplate is reduced to the area of the prosthesis, thereby reducing the volume velocity produced by a given stapes (linear) velocity. The reduction in effective footplate area also reduces the area of the cochlear fluid over which the force generated by the stapes is applied. Whereas the reduced footplate area leads to a local increase in pressure over the surface of the prosthesis area, the average pressure at the cochlear entrance is reduced. The reduction in stapes volume velocity and cochlear sound pressure leads to a decrease in ossicular coupling and the development of an air–bone gap.The smaller the area of the stapes prosthesis, the greater the air–bone gap. Model predictions of the relationship between piston diameter and residual air–bone gap after a stapedotomy suggest that a 0.8 mm piston causes a 5 dB gap at frequencies of 1000 Hz and below, a 0.6 mm piston is predicted to cause a 10 dB gap, and 0.4 mm piston is predicted to cause a 15 dB gap. These predictions assume that the effective vibrating “footplate” surface area after a stapedotomy is no more than the area of the lower end of the prosthesis. In cases of partial stapedectomy with placement of a vein graft and a stapes prosthesis, the effective vibrating surface may be greater than the area of the prosthesis alone, and our predictions may overestimate the air–bone gap.
SUMMARY
This chapter has summarized some simple acoustic ideas, such as how sound propagates, what sound pressure is, and how the propagation of sound around objects depends on the relationship between the dimensions of the object and the wavelength of the sound.The influence of sound propagation velocity and wavelength on how we localize sounds is described. Also discussed is how the mechanics and acoustics of the middle ear shape the sounds that reach the inner ear and how pathological alterations in middle ear structure can affect hearing. Finally, the acoustics and mechanics after middle ear reconstructive surgery are discussed.
SUGGESTED READINGS
American National Standards Institute. Audiometer Standard 1969;3:6
Dallos P.The Auditory Periphery. NewYork:Academic Press; 1973 Funnell WRJ, Decraemer WM. On the incorporation of moiré shape measurements in finite-element models of the cat
eardrum. J Acoust Soc Am 1996;100:925–932
Goode RL, Friedrichs R, Falk S. Effect on hearing thresholds of surgical modification of the external ear. Ann Otol Rhinol Laryngol 1977;86:441–451
Goode RL, Nishihara S. Experimental models of ossiculoplasty. Otolaryngol Clin North Am 1994;27:663–675
Khanna SM, Tonndorf J. Tympanic membrane vibrations in cats studied by time-average holography. J Acoust Soc Am 1972; 51:1904–1920
Kurokawa H, Goode RL. Sound pressure gain produced by the human middle ear. Am J Otol 1995;113:349–355
Merchant SN, Ravicz ME, Voss SE, Peake WT, Rosowski JJ. Toynbee Memorial Lecture 1997: middle ear mechanics in normal, diseased and reconstructed ears. J Laryngol Otol 1998;112:715–731
Merchant SN, Rosowski JJ, Ravicz ME. Middle-ear mechanics of type IV and type V tympanoplasty, II: Clinical analysis and surgical implications. Am J Otol 1995;16:565–575
Murakami S, Gyo K, Goode RL. Effect of middle ear pressure change on middle ear mechanics. Acta Otolaryngol (Stockh) 1997;117:390–395
Peake WT, Rosowski JJ, Lynch TJ III. Middle-ear transmission: acoustic vs. ossicular coupling in cat and human. Hear Res 1992;57:245–268
Puria S, Peake WT, Rosowski JJ. Sound-pressure measurements in the cochlear vestibule of human cadavers. J Acoust Soc Am 1997;101:2745–2770
Rosowski JJ. The effects of externaland middle-ear filtering on auditory threshold and noise-induced hearing loss. J Acoust Soc Am 1991;90:124–135
Rosowski JJ. Models of external and middle-ear function. In: Auditory Computation New York: Springer-Verlag; 1996:15–61. Hawkins H, McMullen T, Popper A, Fay R, eds. The Springer Handbook of Auditory Research; vol 6
Shaw EAG. The external ear. In: Auditory System (pp. 455–490). New York: Springer-Verlag; 1974:455–490. Keidel WD, Neff WD, eds. Handbook of Sensory Physiology; vol 5
Sivian LJ, White SD. On minimum sound audible fields. J Acoust Soc Am 1933;4:288–321
von Békésy G. Experiments in Hearing. New York: McGraw-Hill; 1960
Voss SE. Effects of Tympanic-Membrane Perforations on MiddleEar Sound Transmission: Measurements, Mechanisms and Models [PhD dissertation]. Cambridge: Massachusetts Institute of Technology; 1998
Voss SE, Rosowski JJ, PeakeWT. Is the pressure difference between the oval and round windows the effective acoustic stimulus for the cochlea? J Acoust Soc Am 1996;100(3):1602–1616
Wever EG, Lawrence M. Physiological Acoustics. Princeton, NJ: Princeton University Press; 1954
Wullstein H. Results of tympanoplasty. Arch Otolaryngol 1960; 71:478–485
YostWA. Fundamentals of Hearing. NewYork:Academic Press; 1994 Zwislocki J.The role of the external and middle ear in sound transmission. In: Human Communication and Its Disorders. New York: Raven Press; 1975:45–55.Tower DB, ed.The Nervous
System; vol 3

274 CHAPTER 21 ACOUSTICS AND MIDDLE EAR MECHANICS FOR OTOLARYNGOLOGY
SELF-TEST QUESTIONS
For each question select the correct answer from the lettered alternatives that follow.To check your answers, see Answers to Self-Tests on page 716.
1.Which of the following statements best describes the middle ear gain in humans?
A.30 dB and independent of frequency
B.20 dB and independent of frequency
C.20 dB with a best frequency near 4 to 8 kHz
D.20 dB with a best frequency near 1 to 2 kHz
2.The inner ear responds best to
A.Sound pressure applied to the oval window
B.Sound pressure applied to the round window
C.The sum of sound pressures at the two windows
D.The difference in sound pressure at the two windows
3.What is the primary mechanism of conductive hearing loss due to a tympanic membrane perforation?
A.A reduction in area of the tympanic membrane
B.A reduction in coupling of the tympanic membrane motion to the malleus
C.A reduction in sound pressure difference across the tympanic membrane
D.An increase in sound pressure at the round window compared with the oval window
4.Which of the following statements concerning hearing results after a stapedotomy are false?
A.The smaller the area of the stapes prosthesis, the smaller the air–bone gap.
B.The larger the area of the stapes prosthesis, the smaller the air–bone gap.
C.The area of the stapes prosthesis is not correlated to the size of the air–bone gap.
D.Model analyses predict a small residual air–bone gap after a stapedotomy.

Chapter 22
SURGICAL ANATOMY OF
THE TEMPORAL BONE
HINRICH STAECKER AND ADRIEN A. ESHRAGHI
EXTERIOR ANATOMY OF THE TEMPORAL BONE |
NERVES RUNNING THROUGH THE TEMPORAL BONE |
|
ANATOMY OF THE TYMPANIC MEMBRANE AND |
EPONYMS AND ANATOMICAL PEARLS |
|
MIDDLE EAR CAVITY |
SUGGESTED READINGS |
|
ANATOMY OF THE MASTOID AND PETROUS APEX |
||
SELF-TEST QUESTIONS |
||
ANATOMY OF THE COCHLEA AND VESTIBULAR SYSTEM |
||
|
||
VASCULAR SUPPLY |
|
The anatomy of the temporal bone represents the junction of the structures of the neck, nasopharynx, and the cranium. Multiple vital neural and vascular structures pass through this area. In addition the temporal bone contains the sensory receptor organs of hearing and balance. Inferiorly, the sternocleidomastoid muscle and the great vessels of the neck attach and enter the temporal bone.Anteriorly, the temporal bone articulates with the condyle of the mandible and attaches to the midface via the zygomatic arch. The eustachian tube connects the aerated spaces of the middle ear and mastoid cavity to the nasopharynx. Medially, the temporal bone contacts the posterior and middle fossae of the skull base. Being at such a nexus makes the temporal bone a target for a bewildering variety of diseases. Although the anatomy of the temporal bone will be described in this passage, a full understanding of the complex anatomy of the temporal bone can only be obtained through repeated anatomical dissection.
EXTERIOR ANATOMY OF
THE TEMPORAL BONE
The lateral view of the temporal bone (Fig. 22-1A) presents several key anatomical features. The temporal line represents the insertion point of the temporalis
muscle and roughly approximates the position of the floor of the middle cranial fossa. The mastoid tip is the inferior extent of the mastoid portion of the temporal bone. Its inferior extent varies with age, with infants having only a minimal projection of the mastoid. This, along with the delayed ossification of the tympanic ring, makes it necessary to modify incisions for mastoid surgery in infants to avoid damaging the facial nerve. The spine of Henle approximates the position of the antrum. Visible in the external auditory canal are the tympanosquamous and tympanomastoid fissures that mark the fusion planes between the squamous, tympanic, and mastoid bones.The petrous bone makes up the fourth component of the temporal bone and lies deep to the lateral portion of the temporal bone. From the inferior aspect (Fig. 22-1B) one can observe the relationship between the stylomastoid foramen and the digastric muscle that inserts in a groove on the mastoid tip. Internally, this represents the digastric ridge. The carotid canal, mandibular fossa, and styloid process are also present. The superior projection encompasses the middle cranial fossa. This area is rather poor in landmarks. The arcuate eminence approximates the position of the superior semicircular canal. On the posterior projection of the temporal bone (Fig. 22-1C)

276 CHAPTER 22 SURGICAL ANATOMY OF THE TEMPORAL BONE
A 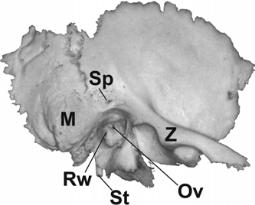 B
B
|
Figure 22-1 External bony structures of the temporal bone: (A) lateral |
|
view, (B) inferior view, and (C) posteromedial view.AE, arcuate eminence; CC, |
|
carotid canal; DR, digestive ridge; IAC, internal auditory canal; M, mastoid; |
|
MF, mandibular fossa; Ov, oval window; P, petrosquamous suture; PF, petrotym- |
|
panic fissure; Rw, round window niche; SMF, stylomastoid foramen; Sp, spine of |
C |
Henle; St, styloid process; Z, zygoma. |
one can see the internal auditory canal (IAC).The cochlear nerve occupies the anteroinferior portion of the IAC, and the facial nerve occupies the anterosuperior quadrant of the IAC and is separated from the cochlear nerve via the transverse crest (see Fig. 22-2). The superior and inferior vestibular nerves occupy the posterior half of the IAC. Of note is that the IAC is in line with the external auditory canal (EAC), providing a useful radiological and surgical landmark. The operculum is the opening to the bony portion of the endolymphatic sac. The transverse and sigmoid sinuses can be seen coursing along the edge of the temporal bone.
ANATOMY OF THE TYMPANIC MEMBRANE AND MIDDLE EAR CAVITY
The tympanic membrane is an irregularly round membrane that measures 8 9 mm and is 0.1 mm thick. It is divided into a pars tensa and a pars flaccida that are separated by the attachment of the anterior and
posterior tympanic striae. The pars tensa is firmly attached to the annulus and in its center is attached to the long process of the malleus.The pars flaccida forms the lateral border of Prussak’s space.The pars flaccida at this point attaches to the tympanic incisura or notch of Rivinus, thereby making up the superior recess of the tympanic membrane. Prussak’s space is defined superiorly by the lateral malleal ligament, medially by the head of the malleus, and inferiorly by the anterior and posterior malleal folds.The pars tensa consists of three layers: a squamous epithelial external layer, a fibrous middle layer (arranged in both radial and circular patterns), and a mucosal internal layer.The pars flaccida is composed of two layers, and the fibrous middle layer is not present.
The middle ear cavity (MEC) itself can be divided into five parts: the hypotympanum, compromising the floor of the middle ear; the epitympanum, making up the roof; the protympanum and posterior tympanum, composing the anterior and posterior borders, respectively; and the mesotympanum, making up the central

ANATOMY OF THE TYMPANIC MEMBRANE AND MIDDLE EAR CAVITY 277
Figure 22-2 The organization of the cranial nerves within the internal auditory canal (IAC) (medial to lateral view).The seventh nerve is located in the anterosuperior segment of the IAC and is separated from the superior division of the vestibular nerve (VIIIs ) in the distal portion of the IAC by Bill’s bar.The transverse crest separates the distal IAC into an upper and lower portion,providing another important surgical landmark.The cochlear nerve occupies the anteroinferior portion of the canal, whereas the inferior division of the vestibular nerve (supplying the macula of the saccule and the posterior canal crista) occupies the inferior portion of the IAC.
section (see Fig. 22-3, canal wall-up mastoidectomy view of the MEC). Sound conduction occurs through the action of three ossicles, the malleus, incus, and stapes (see Fig. 22-4, the isolated ossicles that form the ossicular chain).
Figure 22-3 Temporal bone dissection showing a canal wall-up mastoidectomy.E,endolymphatic sac;EAC,external auditory canal;LS, lateral semicircular canal;PS,posterior semicircular canal;S,sigmoid sinus;Tg, tegmen;VII, facial nerve.
Figure 22-4 The ossicles of the middle ear cavity: (A) malleus,
(B) incus, and (C) stapes.
The malleus is divided into the head, neck, lateral process, anterior process, and manubrium (Fig. 22-4A). The anterior process runs toward the glasserian fissure (pertotympanic fissure), the exit point of the chorda tympani nerve from the middle ear. The malleus is attached to the tympanic membrane via a cartilaginous cap at the lateral process and is completely enveloped in the lamina propria layer at the level of the umbo. Removal of the tympanic membrane at this point is impossible without causing a perforation. Just inferior to the lateral process, the malleus is loosely attached to the tympanic membrane via the plica mallearis. This layer may be elevated to allow for the attachment of an ossicular prosthesis to the malleus.
The incus is composed of the body, which articulates with the head of the malleus, the short process, and the long process, which articulates with the head (caput) of the stapes (Fig. 22-4B).
The stapes is the final bone in the ossicular chain that links the tympanic membrane to the oval window and that on average measures 3.2 mm in height (Fig. 22-4C). The footplate generally measures an average size of 1.4 2.9 mm and is articulated into the oval window via the annular ligament.
The ossicles are suspended by a complex series of membranes and ligaments that are thought to be formed by the migration and interaction of the mesenchymal tissues of the four embryonic pouches. These ligaments and folds of the mesotympanum and epitympanum

278 CHAPTER 22 SURGICAL ANATOMY OF THE TEMPORAL BONE
constitute barriers that tend to channel disease growth (e.g., cholesteatoma) along characteristic anatomical pathways. Besides the anterior and posterior malleal folds, the malleus is suspended by the anterior, lateral, and superior suspensory ligaments. The tensor tympani tendon attaches the neck of the malleus medial to the cochleariform process and to the tensor tympani muscle. The incus is held in place by the posterior incudal ligament that attaches to the short process of the incus and by the medial and lateral incudal ligaments that secure the body of the incus to the head of the malleus. The long process of the incus articulates with the head of the stapes and is the most common site for bony erosion in chronic otitis media.The tendon of the stapedius attaches to either the neck or the posterior crus of the stapes.The stapedius muscle is the smallest muscle of the body and is innervated by a branch of the facial nerve. The body of the stapedius muscle is encased within the pyramidal eminence of the middle ear. Lateral to the pyramidal eminence, the chorda tympani nerve enters into the MEC. The MEC is connected to the pneumatized portion of the mastoid bone via the posterior epitympanum that leads into the aditus ad antrum and from there into the mastoid antrum. The carotid artery and the opening to the eustachian tube make up the anterior wall of the middle ear, whereas the roof of the MEC (tegmen tympani) separates the middle ear from the middle fossa and temporal lobe dura. As discussed previously, the lateral boundaries of the MEC are the tympanic ring and membrane, and the scutum (consisting of bone at the junction of the squamous and tympanic bones). Erosion of the scutum is a common radiological sign of cholesteatoma.
The medial wall of the MEC borders the sensory organs of the inner ear. The oval and round windows are separated by the sinus tympani, a niche where cholesteatoma can be overlooked. The subiculum is a ridge of bone that separates the round window niche from the sinus tympani. The ponticulus separates the oval window from the sinus tympani. The facial canal is located superior to the oval window niche and is a common location for dehiscence of the facial nerve.The facial nerve turns medially to form the geniculate ganglion just posteromedially from the cochleariform process. This in turn represents the second genu.The area anterior to the head of the malleus is the epitymanic recess. This may be partially separated by a septum of bone.
One of the most important structures for maintaining adequate function of the middle ear is the eustachian tube.The eustachian tube is composed of a bony portion (one third total length, proximal to the middle ear) and a cartilaginous portion (two thirds total length, distal to the middle ear) 3 cm long in its total length and
2 mm wide at its narrowest point. It crosses the carotid artery and opens into the nasopharynx.The cartilaginous portion of the tube is shaped like an upside down U and opens into the fossa of Rosenmüller. Tumors in this region (nasopharynx) may present as a unilateral serous otitis media. The eustachian tube is lined by ciliated pseudostratified respiratory type epithelium. Opening of the tube is an active event controlled by three muscles: the tensor vela palatini, the levator vela palatine, and the salpingopharyngeal. Closure of the tube is a passive event. The dominant muscle is the tensor vela palatine, innervated by cranial nerve (CN) V, that acts to pull the lateral portion of the cartilage inferiorly.The levator veli palatine, innervated by CN X, opens the lumen of the eustachian tube.
ANATOMY OF THE MASTOID AND PETROUS APEX
The mastoid cavity is variable in size, depending on both the age of the patient and any history of prior otologic disease. During infancy the mastoid consists of a small cavity (the antrum). With increasing age, pneumatization of the mastoid air cells develops, yielding a variablesized cavity. Long-standing eustachian tube dysfunction can prevent pneumatization and results in a sclerotic cavity, which is seen in up to 20% of the population. Several pneumatization tracts connect the mastoid air cells to the hypotympanum (retrofacial cells) and to the petrous apex (posteromedial, posterosuperior, and subarcuate cell tracts). The petrous apex air cells are in turn connected to the middle ear and/or the bony portion of the eustachian tube.The mastoid cavity itself is divided into a lateral and a medial half by the petrosquamous (Körner’s) septum. There are also several accessory air cell tracts, including the retrosigmoid cells, the tip cells, the tegmental cells, and the sinodural cells.Awareness of these air cells is important in removing residual chronic otitis media.
ANATOMY OF THE COCHLEA AND VESTIBULAR SYSTEM
The membranous sensory structures of the inner ear are surrounded by a dense bony capsule that is derived from periotic cephalic mesenchyme (Fig. 22-3; see Chapter 20). The color and hardness of the bony otic capsule make it easily recognizable during temporal bone surgery.The inner ear may be divided into the cochlea, the vestibule, the three semicircular canals with their associated ducts, and the endolymphatic duct and sac.The oval window opens into the vestibule that contains two bony
