
Учебники / Otolaryngology - Basic Science and Clinical Review
.pdf
ANTIBIOTICS 109
flumazenil must be readily available. Minimal effective concentrations of the local anesthetics should be used to decrease the total amount of anesthetic. For example, 1% lidocaine may be used for skin infiltration; 0.5% lidocaine is effective in subcutaneous areas.
Recognition of Toxicity
Local anesthetic toxicity is biphasic, beginning with alterations in the CNS and progressing to cardiac arrhythmias and cardiac arrest. Signs and symptoms of CNS toxicity include drowsiness (especially with lidocaine), personality changes, headache, tinnitus, tingling in lips or tongue, muscle tremors, and convulsions. Drowsiness is so common when lidocaine is used that it may be overlooked as a harbinger of worse things to come. The earliest indication of incipient toxicity is a change in personality. It is imperative that the anesthesiologist (or surgeon if no anesthesiologist is in attendance) maintain voice contact with the patient. Even if the patient has been premedicated with a benzodiazepine, a baseline can be established and variance noted. Deep sedation (as with, e.g., propofol) makes effective contact impossible. Tingling in lips or tongue is probably not a true sign of toxicity, but only a reflection of high concentrations of local anesthetics in richly perfused areas. These signs do indicate high blood levels of local anesthetic and serve to warn the clinician of troubles to come.Tremors begin in the small muscles of the hand or face, progressing to large muscle groups and frank convulsions. Recognition of the early signs of toxicity should prevent this occurrence.
Among the most commonly used local anesthetics bupivacaine causes the greatest depression of cardiac excitability and conduction, lidocaine the least and ropivacaine intermediate. Lidocaine overdose causes a marked reduction in myocardial contractility, bradycardia, hypotension, and respiratory depression. The electrocardiogram may demonstrate first-degree atrioventricular block and intraventricular conduction block. Bupivacaine overdose will cause ventricular tachycardia and fibrillation.The premonitory CNS signs may be lacking, and the first evidence of toxicity may be cardiac arrest.The toxicity of ropivacaine resembles that of lidocaine, but with periods of ventricular arrhythmia. Bupivacaine is approximately four times more potent than lidocaine as local anesthetic but is approximately nine times more toxic.
An interesting concept suggests that the lethality of bupivacaine is not caused by any direct toxic effect on the heart, but is actually a CNS toxicity caused by an imbalance between sympathetic and parasympathetic activity, causing hypertension and cardiac dysrhythmias.
This suggests that appropriate therapy of bupivacaine toxicity might best be directed primarily at the brain, not the heart, and may explain the efficacy of benzodiazepines in treating bupivacaine overdose.
Management of Toxicity
Toxicity is best managed by avoidance, the use of suitable benzodiazepine premedication, administration of minimal effective concentrations of the drugs to avoid overdose, and the incorporation of epinephrine 1:200,000 when feasible into the anesthetic mixture. When large doses of local anesthetics are used, it is advisable to monitor the patient with electrocardiography to detect cardiac arrhythmias.A pulse oximeter is useful to detect hypoxia, and a capnograph may serve to detect hypoventilation, hypercarbia, and respiratory acidosis. Severe hypoxia increases the cardiotoxicity of bupivacaine.
Treatment of Toxicity
CNS hyperactivity may be treated with the intravenous administration of a benzodiazepine such as diazepam 0.1 mg/kg or preferably midazolam in 0.5 mg increments to a maximum of 5 mg. The anesthesiologist is more likely to use thiopental, a thiobarbiturate, in a dose of 1 to 2 mg/kg up to 4 to 5 mg/kg if necessary. These doses may be repeated if necessary if blood pressure is maintained and ventilation supported. Hypoxia and acidosis must be corrected.
If convulsions occur and persist despite appropriate therapy, muscle relaxants must be used to induce paralysis, and the patient then intubated and mechanical ventilation instituted. Hyperventilation will reduce PaCO2 (partial pressure exerted by carbon dioxide dissolved in arterial plasma and red blood cell water) and increase the local anesthetic toxic threshold.
Hypotension is treated with intravenous fluids and positive inotropes (e.g., epinephrine, dopamine, or dobutamine). Bretylium (5 mg/kg) may be useful in refractory cardiac arrhythmias.
SUMMARY OF LOCAL ANESTHETICS
Local anesthetics are useful, safe drugs, applicable to a wide variety of surgical procedures. Adverse effects are rare and may be treated effectively if recognized early.
ANTIBIOTICS
As pharmaceutical companies keep pace with the development of bacteria resistant to antibiotics, the number of antibacterial agents continues to increase. Entirely new

110 CHAPTER 8 PRINCIPLES OF PHARMACOLOGY
classes of antibiotics are also under development and may make their way onto the marketplace in the next few years. Bacteria develop resistance to antibiotics because of one simple reason: the use of antibiotics. Bacterial resistance is merely a survival technique and the result of evolutionary pressure on bacteria.Although much antibiotic use is justifiable and necessary to treat infections, excessive and unnecessary prescribing of antibiotics by physicians in many subspecialties, both for inpatients and outpatients, as well as the use of antibiotics in animal feed, contributes to needless bacterial resistance to antibiotics and the consequent occasional inability of physicians to treat bacterial infections successfully. The need for new antibiotics will continue for the foreseeable future.
All physicians should realize that it is impossible to eliminate bacteria from the world (and not even desirable to do so), and that use of antibiotics eventually always leads to bacterial resistance. A small fraction of the bacteria living in the body of a patient will become resistant to whatever antibiotic is given to that patient. If the number of bacteria in an infected site is relatively small, the infection will be cured. However, if the bacterial load is large, a superinfection by resistant bacteria may result. In either case, or if there is no bacterial infection at all, bacteria in the gastrointestinal tract or on the skin may acquire resistance. This is true even if the rate of acquiring resistance to a particular antibiotic is only one in a trillion (10 12), because there are an estimated 1014 bacteria in the human body. If resistant bacteria multiply and cause infection, they may be difficult or even impossible to treat, and even if they do not cause infection, they may be spread to others. Therefore, physicians must use good medical judgment in deciding whether or not to treat a patient with antibiotics.
It is also important to note that cultures should be taken in the correct manner. Unless a particular species of bacteria is being sought, such as Streptococcus pyogenes from a throat culture, swab cultures should never be done. Even in an obviously infected area, swab cultures cannot distinguish the bacteria that are causing the infection from those that are simply on the surface. Instead, the infected area should be debrided or the infected body cavity should be entered in a sterile manner for cultures to be properly done.
In the subspecialty of otorhinolaryngology, these principles are most easily demonstrated with sinusitis and otitis, many cases of which are viral in origin. Indiscriminate use of antibiotics for these conditions, both in adults and children, undoubtedly contributes to resistance by many common bacteria. However, viral and bacterial forms of these diseases are impossible to
distinguish on clinical grounds, and swab cultures of ears and sinuses are useless. Moreover, invasive techniques such as tympanocentesis and sinus puncture to make etiologic diagnoses are not justified on a routine basis. Therefore, clinicians are often forced to treat these conditions with antibacterials without proof of a bacterial cause.
Finally, it is important to note that even if a package insert states that a particular antibiotic is indicated for a specific condition, the phrase “due to susceptible bacteria” is always implied if not explicitly stated. Because of increased bacterial resistance, some antibiotics are no longer as useful for certain types of infections as they were when they were first marketed, and they should no longer be used empirically to treat these conditions. Conversely, just because an antibiotic does not have a particular indication does not mean that it will not work, and there are situations in which it is reasonable to use an antibiotic in an “off-label” manner, especially when multiresistant nosocomial bacteria are suspected or proven. Physicians should know the susceptibility patterns of common bacteria in their own local hospitals so that they can make a reasonable choice of empirical antibiotics for their hospitalized patients.The microbiology laboratories of most hospitals are glad to supply this information to their physicians.
Groups of antibiotics and individual agents are reviewed on the following pages, with some focus on their use for infections of the ears, nose, and throat, as well other uses that otorhinolaryngologists are likely to encounter. When brand names are commonly used for a specific antibiotic, they are supplied in parentheses after the generic names. For more detailed reviews of antibiotics, and for thorough discussions of their uses for other types of infections, a variety of texts may be consulted (see Suggested Readings). A multitude of pocket-sized handbooks (e.g., The Medical Letter Handbook of Antimicrobial Therapy, The Sanford Guide to Antimicrobial Therapy) have also been published that summarize antibiotic dosing, empirical selection by site of infection, dosages in patients with renal failure and in pediatric patients, achievable serum concentrations, side effects, and so on. Even clinicians who are familiar with antibiotics will find one or more of these handbooks useful for prescribing antibiotics in certain situations.
SULFONAMIDES AND TRIMETHOPRIM
Sulfonamides were the first type of modern antibiotic used. The first scientific report of antibacterial activity described the use of sulfachrysoidine in the treatment of streptococcal infections in mice. Sulfanilamide (Prontosil)

ANTIBIOTICS 111
became the first antibiotic to be widely used in humans after scientists discovered that it was the active metabolite of sulfachrysoidine.After scientists realized that chemical modifications of the sulfanilamide molecule greatly expanded its antibacterial activity and reduced its side effects, thousands of sulfonamides were studied, and dozens were used to treat patients. Only a small fraction of these are used nowadays, but they are still valuable antibiotics.
Currently, the sulfonamide most frequently used for systemic administration is sulfamethoxazole, which is almost always used in a fixed combination with trimethoprim.This preparation is marketed under several brand names, such as Bactrim, Cotrim, and Septra, and is also available generically.The different brands are equivalent. Single-strength (SS) pills consist of 80 mg of trimethoprim and 400 mg of sulfamethoxazole, and double-strength (DS) pills contain 160 and 800 mg, respectively. It is useful for the treatment of acute otitis media and sinusitis, as well as for urinary tract infections, exacerbations of chronic bronchitis, and other conditions.
Another sulfonamide that is still used by pediatricians in some areas is a suspension of sulfisoxazole in a fixed combination with erythromycin, known as Pediazole. Each teaspoon (5 mL) contains 600 mg of sulfisoxazole and 200 mg of erythromycin. It is indicated only for otitis media due to susceptible strains of Haemophilus influenzae, which is too narrow an indication for routine empirical use because other species of bacteria that cause otitis media, especially Streptococcus pneumoniae, are frequently resistant.
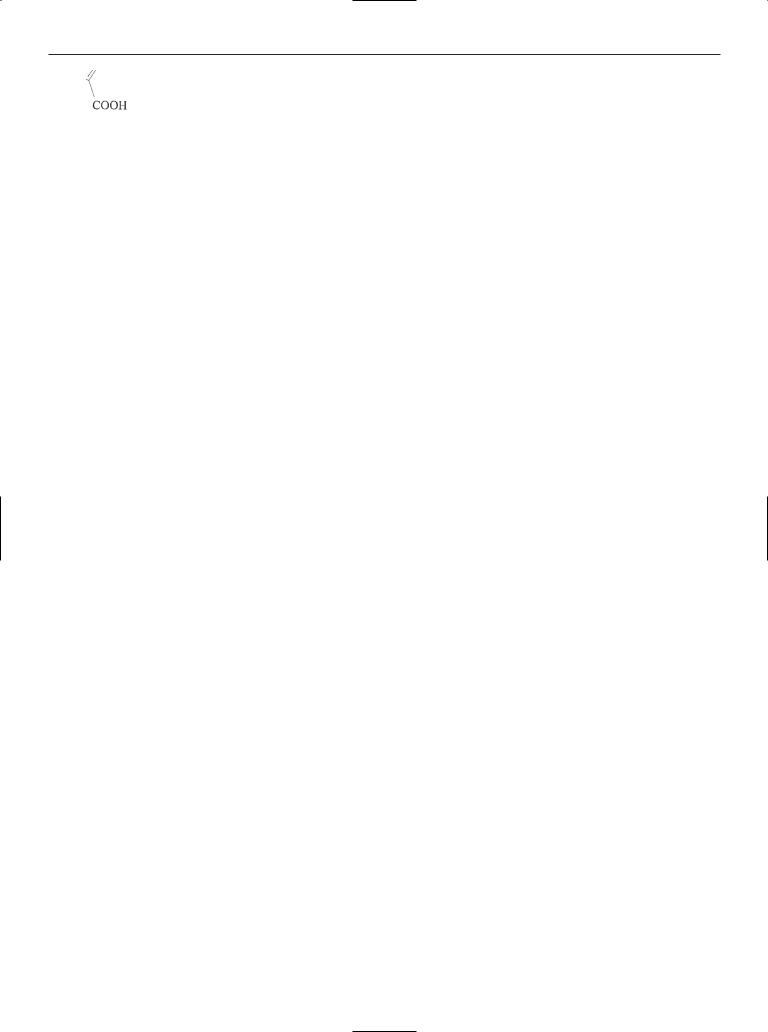
All currently used sulfonamides consist of a benzene ring with an aminosulfonyl group on C1 and an amino group on C4.Addition of a heterocyclic aromatic ring on N1 of the aminosulfonyl group, as in sulfamethoxazole, greatly increases antibacterial activity compared with the original sulfanilamide (Fig. 8-3).
Chemically, sulfonamides resemble para-aminoben- zoic acid (PABA), and their mechanism of action is to inhibit the enzyme dihydropteroic acid synthetase, which catalyzes the incorporation of PABA into dihydropteroic acid to form dihydrofolic acid. The latter compound is
Figure 8–3 Molecular structure of sulfamethoxazole.
important in the transfer of single carbon fragments in numerous biochemical pathways. Humans cannot synthesize dihydrofolic acid and must ingest folic acid in their diet or in vitamin supplements.Therefore, sulfonamides do not adversely affect humans in the same way that they harm bacteria.
Bacteria become resistant to sulfonamides via overproduction of PABA to counteract the competitive inhibition by sulfonamides. This is accomplished by production of a mutant dihydropteroic acid synthetase that does not bind well to sulfonamides (alteration of the target site), or by decreased uptake of sulfonamides.
The spectrum of activity of sulfonamides includes streptococci (including some strains of S. pneumoniae),
H. influenzae, and Moraxella catarrhalis. Strains of
S. pneumoniae that are resistant to penicillin are also frequently resistant to other classes of antibiotics as well, including sulfonamides, and these strains account for 40% of isolates in some areas of the United States. Outpatient-type enteric Gram-negative bacilli, including Escherichia coli, Klebsiella spp., Enterobacter spp., Morganella morganii, and Proteus spp., are also usually susceptible to sulfonamides. Sulfonamides should not be given for the treatment of sore throats because they do not eradicate group A streptococci (S. pyogenes) from the tonsils as well as penicillin does.
Sulfonamides are fairly well absorbed when taken by mouth, and the trimethoprim-sulfamethoxazole combination needs to be dosed only twice a day for the treatment of most types of infections. Once absorbed into the bloodstream, they distribute fairly well to most body tissues, including the CNS. Metabolism is by acetylation and glucuronidation, which occur in hepatocytes. Glucuronidation increases solubility in water so that excretion, which is via glomerular filtration, can occur.
The most common side effects are rashes due to allergic hypersensitivity; most often, this is an erythematous rash that disappears after the sulfonamide is stopped. Occasionally, Stevens-Johnson syndrome (erythema multiforme major), a severe, blistering, and desquamating mucosal rash, may occur.This is sometimes preceded by other types of rashes, but not always. Sulfonamides should not be given late in pregnancy or to newborns because they compete with bilirubin for the negligible amounts of glucuronyl transferase in the bloodstream of newborns. If the bilirubin cannot be conjugated, kernicterus may result. Other rare but serious side effects include fulminant hepatic necrosis and agranulocytosis.
Trimethoprim was developed for use with sulfamethoxazole because it has a similar mechanism of action, spectrum of activity, and pharmacokinetics. It is

112 CHAPTER 8 PRINCIPLES OF PHARMACOLOGY
a 2,4-diaminopyrimidine and is not chemically related to the sulfonamide group. The only other chemically related antibiotic is pyrimethamine, which is an antiparasitic agent. (Trimethoprim binds very well to bacterial dihydrofolate reductase, and pyrimethamine binds very well to parasitic dihydrofolate reductase; neither one binds very well to the human enzyme.) Dihydrofolate reductase reduces dihydrofolic acid to tetrahydrofolic acid. Because this biochemical reaction directly follows the one that is inhibited by sulfonamides, it was reasoned that combining trimethoprim with sulfamethoxazole would have a synergistic action, and this has been borne out by in vitro testing. (In microbiology, synergy means that bacterial killing actually obtained as a result of combining two antibiotics is more than the killing expected by simply adding their individual effects.)
A 1:5 fixed ratio of trimethoprim to sulfamethoxazole was selected because this combination yields a concentration of 1 to 20 in serum. (Sulfamethoxazole is absorbed 4 times as well as trimethoprim.) Because trimethoprim is 20 times as active as sulfamethoxazole on a milligram per milligram basis, this yields equal activities of both.
Distribution of trimethoprim into various body tissues and fluids is also very good, with therapeutic levels found in many areas. About 60% of a dose is excreted unchanged by renal tubular secretion in urine within 24 hours, with the remainder excreted in bile or undergoing oxidation or hydroxylation in hepatocytes to inactive metabolites. Side effects are also similar in quality to those due to sulfonamides, although rashes occur much less frequently.
PENICILLINS
Although Alexander Fleming noted in 1928 that Staphylococcus aureus was unable to grow near colonies of Penicillium notatum, the full importance of this finding was not understood, until systematic studies of penicillins were undertaken several years later. It was not until 1941 that penicillin G was first used in humans, and its development would have been further delayed if it had not been needed to fight battlefield infections during World War II. The penicillins, cephalosporins, and carbapenems are the three classes of -lactam antibiotics.
The earliest forms of penicillin were a mixture of different natural penicillins that were designated by letters. The most active of these compounds was penicillin G (benzylpenicillin), which is still used for parenteral administration. Penicillin G is available in two crystalline
Figure 8–4 Penicillin nucleus.
forms (as sodium and potassium salts), as a less soluble procaine salt, and as an even less soluble benzathine (dibenzyl ethylene diamine) salt. Penicillin V (phenoxymethylpenicillin) is used for oral administration because it is more resistant to hydrolysis mediated by stomach acid.
Even though the initial antibacterial property of penicillin was observed on S. aureus, nearly all strains of these bacteria are now resistant to penicillin G and penicillin V due to the production of a penicillinase that hydrolyzes the penicillin molecule (Fig. 8-4). Resistance to penicillin G and penicillin V by S. aureus was first noted in the 1950s. Both these forms of penicillin have remained active against most streptococci, especially anaerobic streptococci found in the mouth and-hemolytic streptococci. However, in the past 10 years, many strains of S. pneumoniae have become intermediately or highly resistant to penicillin, with rates of resistance approaching 40% in some areas of the United States and even higher rates elsewhere.
Because the individual penicillins in the initial natural mixtures differed only in their side chain, or “R group,” scientists reasoned that by either modifying the side chain or putting a synthetic side chain onto the penicillin nucleus, they might be able to increase the antibacterial activity of the natural penicillins. There are several groups of these semisynthetic penicillins that have activity against staphylococci, enteric Gram-negative bacilli, and other bacteria.These are outlined as follows.
Penicillinase-resistant (antistaphylococcal) penicillins: methicillin,oxacillin,nafcillin,cloxacillin,and dicloxacillin. These all have very large R groups that stereochemically prevent penicillinases produced by staphylococci from getting close to the -lactam ring and hydrolyzing it. Although methicillin is no longer used clinically, it is still employed by microbiology laboratories for susceptibility testing of staphylococci to all penicillins, cephalosporins, and carbapenems. Oxacillin and nafcillin are for intravenous administration; cloxacillin and dicloxacillin are for oral administration. Penicillins in this group are also active against streptococci, but to preserve

ANTIBIOTICS 113
their effectiveness, they should be used only for the treatment of infections due to staphylococci that are susceptible to methicillin. They are inactive against enterococci and Gram-negative bacilli.
Aminopenicillins: ampicillin and amoxicillin.The amino group on the carbon next to the benzyl side chain allows better entry than that of penicillin G and penicillin V into Gram-negative bacteria. These were originally called “broad-spectrum” penicillins because they had activity against enteric Gram-negative bacilli (especially
E. coli and Proteus mirabilis) and H. influenzae, as well as streptococci and enterococci. Many strains of Gramnegative bacilli are now resistant to ampicillin and amoxicillin, making their empiric use unwarranted for serious infections. However, if culture results show susceptibility, these can still be used. Amoxicillin is used extremely often by pediatricians for the treatment of otitis media because the oral liquid formulation tastes good, making its administration easy in children. The good clinical results suggest that many cases of otitis media do not need treatment with antibiotics because a large proportion are caused either by bacteria that are amoxicillin resistant or by viruses. It is available only in oral formulations (pills and liquid).Ampicillin is available in both oral and intravenous formulations.
Carboxypenicillins: carbenicillin (Geocillin) and ticarcillin (Ticar). The carboxyl group on the carbon next to the benzyl side chain facilitates entry into Pseudomonas aeruginosa, making these antibiotics the first that were active against this species.They also have good activity against other Gram-negative bacilli, in addition to activity against streptococci that are susceptible to penicillin and staphylococci that are susceptible to methicillin. However, neither of these is used frequently nowadays. The absorption of oral carbenicillin is very limited, so it is useful only for the treatment of urinary tract infections, and its intravenous formulation is not as active as penicillins in the ureido group.Ticarcillin, which is available only intravenously, is now almost always used in the ticarcillin-clavulanic acid form (see below).
Ureidopenicillins: mezlocillin (Mezlin) and piperacillin (Pipracil). These have a ureido group, which facilitates their entry into P. aeruginosa. They also have good activity against penicillin-susceptible streptococci and enterococci, methicillin-susceptible staphylococci, and enteric Gram-negative bacilli.They are available only in intravenous formulations.
-lactam– -lactamase inhibitor combinations: ticarcillinclavulanic acid (Timentin; intravenous), amoxicillinclavulanic acid (Augmentin; oral), ampicillin-sulbactam (Unasyn; intravenous), and piperacillin-tazobactam (Zosyn; intravenous). The -lactamase inhibitor component of
these preparations chemically resembles the -lactam ring of penicillin and binds to -lactamases that are produced by bacteria. Because the -lactamase inhibitors have very little antibiotic activity themselves, their function is to prevent the hydrolysis of the penicillin component via their binding to -lactamases. Addition of the -lactamase inhibitor component significantly enhances the antibiotic spectrum of the penicillin component against bacteria that are resistant to penicillins via production of -lactamases. Generally, only-lactamases that are encoded by plasmids bind to-lactamase inhibitors. Therefore, some bacteria, most notably P. aeruginosa, which produce chromosomally encoded -lactamases, are no more susceptible to piperacillin than piperacillin-tazobactam. Staphylococci, enteric Gram-negative bacilli such as E. coli, Klebsiella pneumoniae, and Proteus spp., and Gram-negative anaerobes such as Bacteroides fragilis, all of which produce-lactams that are encoded by plasmids, are more likely to be susceptible to the combinations than to the corresponding penicillin without the -lactamase inhibitor. However, strains of penicillin-resistant S. pneumoniae are no more likely to be susceptible to -lactam– -lactamase inhibitor combinations than they are to the corresponding-lactam alone because their resistance to -lactams is mediated by altered penicillin-binding proteins.
All penicillins have the same mechanism of action. Their chemical structure is similar to that of D-alanyl-D- alanine in the polypeptide portion of peptidoglycan in the bacterial cell wall, which is hydrolyzed by transpeptidases that act as penicillin-binding proteins.All bacteria have several different types of penicillin-binding proteins. After penicillins penetrate the bacterial envelope, they attach to penicillin-binding proteins, which starts a series of events involving accumulation of bacterial cell wall precursors that cannot be incorporated into the growing cell wall, activation of murein hydrolases that are normally involved in the regulation of growing cell walls, and finally bacterial death.
Resistance to penicillins by staphylococci, enteric Gram-negative bacilli, anaerobic Gram-negative bacilli, and some other bacteria (e.g., Neisseria gonorrhoeae) is generally due to production of -lactamases.This is the most clinically important type of bacterial resistance because it is the most common type; in the case of-lactamases encoded on plasmids, it can be passed from bacterium to bacterium (sometimes even across species), and no amount of penicillin can overcome this type of bacterial resistance. Hundreds of different types of -lactamases have been discovered and characterized, but the individual types generally are not important to clinicians. A -lactamase that is active only against

114 CHAPTER 8 PRINCIPLES OF PHARMACOLOGY
penicillins is sometimes termed a penicillinase, and one that is active only against cephalosporins is sometimes called a cephalosporinase.
A second mechanism of resistance, which occurs only in Gram-negative bacilli, is a permeability barrier of the outer membrane. This is accomplished by the production of mutant porins, which are the channels in the outer membrane through which penicillins gain access to the cell membrane.
In the past decade, a third mechanism of resistance has become clinically important, that of the production of altered penicillin-binding proteins, which bind penicillin poorly. S.pneumoniae, which in the United States had been universally susceptible to penicillins prior to the 1980s, is now resistant at rates that make the empirical use of penicillins no longer justifiable when serious pneumococcal infections are suspected. The addition of a -lactamase inhibitor does nothing to overcome this resistance. Third-generation cephalosporins are still useful when this type of resistance is present at an intermediate level because they still bind well enough to the penicillin-binding proteins to have antibacterial activity. However, when high-level penicillin resistance is present, even cephalosporins do not bind to the penicillin-binding proteins, and a macrolide, a quinolone with good streptococcal activity, or vancomycin should be used.
The availability of oral and intravenous formulations of penicillins has been described with each individual type of penicillin. Absorption of oral formulations depends on the particular penicillin; for example, only 60% of an oral dose of penicillin V, 40% of a dose of ampicillin, 75% of a dose of amoxicillin, and 50% of a dose of dicloxacillin are absorbed from the stomach.
In patients with normal renal function, the half-life of most penicillins is relatively short, ranging from as little as 30 minutes for penicillin G and the penicillinase-resistant penicillins to as long as 1.3 hours for piperacillin.
After absorption or intravenous administration, penicillins generally achieve reasonably high tissue and fluid concentrations, with the notable exceptions of the prostate, joint cavities, and cerebrospinal fluid (CSF). However, in the presence of meningeal inflammation, CSF concentrations reach 15% of simultaneous serum concentrations and are adequate to treat meningitis due to Neisseria meningitides and susceptible strains of S. pneumoniae.
Most penicillins are not metabolized to a significant degree. In the case of penicillin G, 20% of a dose is metabolized by hepatic enzymes. Excretion of penicillins is nearly all renal, and active renal tubular secretion by
an organic acid transport system accounts for their relatively short serum half-lives. Probenecid, which competes for penicillins in this transport system, can be given concurrently to prolong the half-life and raise serum levels.
The most important side effects of penicillins are hypersensitivity reactions. Immediate reactions occur within minutes of a dose and in their most severe form consist of hives, urticaria, flushing, wheezing, laryngeal edema, and shock. This is an immunoglobulin E (IgE)– mediated allergic reaction, similar to other forms of anaphylaxis, and occurs with a frequency of 0.004 to 0.4% of courses of treatment. Anaphylaxis to penicillin is more common in patients with a history of atopy, asthma, and other allergies.
Delayed or late allergic reactions, which are mediated by IgM or IgG antibodies, are more common hypersensitivity reactions, occurring in the range of 4 to 8%, and usually are manifested as morbilliform or macular rashes, interstitial nephritis, hemolytic anemia, or serum sickness. There is no way to predict whether a patient who is allergic to one penicillin will be allergic to another. Similarly, the chance that a person with a penicillin allergy is also allergic to cephalosporins or carbapenems is in the range of 1 to 5%, but there is no way to predict a cross-reaction in a particular patient. Because of this, and because other classes of antibiotics are available to treat infections, it is prudent to use a different type of antibiotic if a patient has an immediate hypersensitivity reaction. However, if the type of allergy is delayed hypersensitivity and a penicillin, cephalosporin, or carbapenem is needed, they may be used.
A less common but important side effect of penicillins is seizures if they are given at high doses, especially to patients with mass lesions in the brain, renal insufficiency, or hyponatremia.
CEPHALOSPORINS
After the penicillins, cephalosporins were the second class of -lactam antibiotics developed.The first cephalosporin was isolated by Giuseppe Brotzu from a sewage outlet on the island of Sardinia after he noted that the seawater in the vicinity of the outlet was intermittently free of bacteria. The source of the cephalosporin was a fungus named Cephalosporium acremonium, which was in the water.
Because of their relatively broad antibacterial activity and lack of toxicity, more than 30 different cephalosporins have been marketed in the United States over the last 4 decades. However, many are very similar and therefore can be grouped together. As with other

|
|
|
ANTIBIOTICS 115 |
TABLE 8-5 COMMONLY USED CEPHALOSPORINS |
|
|
|
First Generationa |
Second Generation |
Third Generation |
Fourth Generation |
Oral |
No activity versus |
Intravenous, no Pseudomonas coverage |
Good activity against both |
cefadroxil (Duricef), |
Bacteroides spp. |
but good activity versus Gram- |
Pseudomonas spp. and |
cephalexin (Keflex), |
cefuroximeb (Zinacef, |
positive cocci |
Gram-positive cocci |
cephradine (Anspor, |
Kefurox, Ceftin) |
cefotaxime (Claforan), |
cefepime (Maxipime) |
Velosef) |
cefaclor (Ceclor) |
ceftriaxone (Rocephin), |
|
|
|
ceftizoxime (Cefizox) |
|
Intravenous |
With activity versus |
Intravenous, good Pseudomonas coverage |
|
cefazolin (Kefzol, |
Bacteroides spp. |
but poor activity versus Gram-positive |
|
Ancef) |
cefotetan (Cefotan), |
cocci |
|
|
cefoxitin (Mefoxin) |
ceftazidime (Fortaz,Tazicef, |
|
|
|
Tazidime), |
|
|
|
cefoperazone (Cefobid) |
|
Oral
cefixime (Suprax), cefprozil (Cefzil), cefpodoxime (Vantin)
a Cephalothin, although no longer available in the United States for use in patients, is the representative first-generation cephalosporin used for in vitro susceptibility testing by many microbiology laboratories (the same situation as for methicillin).
bCefuroxime is available both intravenously and orally; the other second-generation cephalosporins are available for intravenous administration only.
antibiotics, large marketing efforts by pharmaceutical companies frequently make distinctions without differences in their efforts to promote one cephalosporin over another. Distinguishing genuine variations between cephalosporins is even more difficult for physicians who are not experts in antibiotics, microbiology, or infectious diseases.
The most widely used classification system for cephalosporins categorizes them as first, second, third, and fourth generation. Table 8-5 is meant to be used as a guide and does not list all available cephalosporins.
Clinicians should be aware that for nearly all purposes, cephalosporins that are grouped together in Table 8-5 are the same.The price that a patient pays to a retail pharmacy, or the cost to the hospital pharmacy from the wholesaler, or formulary availability (either a hospital or insurance formulary) should determine the selection of a cephalosporin within each grouping in
Table 8-5.
The antibacterial activity of cephalosporins requires the 7-aminocephalosporanic acid nucleus.The spectra of activity of individual cephalosporins are determined by the structures of their side chains. The chemical structure of the cephalosporin nucleus is shown in Fig. 8-5.
Cephalosporins have the same mechanism of action as penicillins. By binding to penicillin-binding proteins, which regulate bacterial cell wall synthesis, they induce
several changes in bacterial metabolism, including the production of autolysins, ultimately resulting in cellular lysis. They bind to different penicillin-binding proteins in different proportions than do the penicillins.
The most common mechanism of bacterial resistance to cephalosporins is production of -lactamases, which result in the hydrolysis of the -lactam ring. Many different types of -lactamases have been identified. Some are more active than others; some are constitutively produced, whereas others are inducible; and some are encoded by chromosomal genes, whereas others are produced by genes that are located on plasmids. Additionally, certain cephalosporins are more resistant to-lactamases than others, whereas some are better inducers of -lactamases than others. Therefore, one cephalosporin may be inactive against a certain strain
Figure 8–5 Cephalosporin nucleus.

116 CHAPTER 8 PRINCIPLES OF PHARMACOLOGY
of bacteria that produces a certain -lactamase, whereas another may be active.Although closely related cephalosporins tend to have similar antibacterial activity, there are important differences that require testing of the in vitro activity of several cephalosporins (usually one for each generation) against bacteria from clinical samples by a microbiology laboratory.
Additional mechanisms of resistance include decreased bacterial permeability to cephalosporin molecules (by aerobic Gram-negative bacilli) and bacterial production of altered penicillin-binding proteins that bind poorly to cephalosporins (usually by Gram-positive cocci).
The side chains of individual cephalosporins determine the amount of their uptake into bacterial cells as well as their binding affinities to the various penicillin-binding proteins, resulting in different spectra of activity.
First-generation cephalosporins are active against all streptococci and methicillin-susceptible staphylococci, and against most community-acquired strains of E. coli,
Klebsiella spp., and Proteus spp.
Second-generation cephalosporins have slightly less activity against streptococci and methicillin-susceptible staphylococci than first-generation cephalosporins (but still enough to be useful), but more activity against enteric Gram-negative bacilli. Cefuroxime (Zinacef, Kefurox, Ceftin) has excellent additional activity against H. influenzae (making it useful for the treatment of acute sinus, ear, and respiratory pathogens), and cefotetan (Cefotan) and cefoxitin (Mefoxin) have excellent additional activity against B. fragilis and other anaerobic bacteria.
The intravenous third-generation cephalosporins cefotaxime (Claforan), ceftriaxone (Rocephin), and ceftizoxime (Cefizox) have additional activity against many nosocomial Gram-negative bacilli, including Enterobacter spp., Citrobacter spp., and Serratia marcescens. Ceftazidime (Fortaz, Tazicef, Tazidime) also has activity versus Pseudomonas spp., but is significantly less active against Gram-positive cocci than most other cephalosporins.The oral third-generation cephalosporins have activity against penicillin-susceptible S.pneumoniae, H.influenzae, and M. catarrhalis, making them attractive to use for the treatment of acute respiratory, ear, and sinus infections in children.
Cefepime (Maxipeme), the first fourth-generation (or extended spectrum) cephalosporin, has Gramnegative activity similar to that of ceftazidime (i.e., enteric Gram-negative bacilli including nosocomial strains, and Pseudomonas spp.), and also has good activity against Gram-positive cocci.
All cephalosporins are inactive against enterococci, methicillin-resistant staphylococci, and Listeria monocyto-
genes because the penicillin-binding proteins produced by these bacteria do not bind cephalosporins.
Most cephalosporins can be administered either orally or intravenously, but not both.The only exception to this generalization is cefuroxime. The methods of administration of the individual cephalosporins are outlined in the classification system in Table 8-5.
Although most cephalosporins achieve concentrations in many body tissues and fluids that are adequate to treat infections at these sites, only ceftriaxone, cefotaxime, ceftizoxime, and ceftazidime achieve adequate concentrations in CSF and are considered reasonable treatment for bacterial meningitis. (These are all third-generation cephalosporins. Cefepime also enters the subarachnoid space, but there are not enough clinical data to warrant its use in treating meningitis.) Ceftriaxone also achieves relatively high biliary concentrations.
The cephalosporins are excreted unmetabolized, except for cefotaxime, which is deacetylated, and this metabolite also has antibacterial activity.
The usual mechanism of excretion is via glomerular filtration and tubular secretion, just as for penicillins. Because elimination is exclusively via the kidneys, dosages of cephalosporins must be reduced when they are given to patients with renal failure, or else serum concentrations become excessively high and may lead to seizures. Renal tubular reabsorption can be blocked with probenecid to prolong the serum half-life, as with the penicillins. The only important exception to exclusively renal elimination is ceftriaxone, which is eliminated via bile into feces as well.
As a group, the cephalosporins are relatively safe antibiotics. Side effects are very similar to those caused by the penicillins, in both type and frequency.The most common are allergic hypersensitivity reactions, which range from maculopapular rashes (mild and relatively common) to anaphylaxis (severe but relatively rare). About 1 to 5% of patients who are allergic to penicillin are also allergic to cephalosporins.
Cephalosporins that have a methylthiotetrazolium side chain have been associated with significant gastrointestinal bleeding due to the inhibition of post-translational carboxylation of glutamic acid residues in vitamin K–dependent clotting factors. These cephalosporins are cefamandole (Mandol), cefmetazole (Zefazone), cefotetan (Cefotan), cefoperazone (Cefobid), and moxolactam (Moxam). However, except for cefotetan, nowadays these are rarely used, no longer marketed, or no longer even made.
Other occasional side effects are thrombocytopenia, interstitial nephritis, fever, serum sickness, and Clostridium difficile colitis.
ANTIBIOTICS 117
Figure 8–6 Structure of imipenem.
CARBAPENEMS
These are also -lactam antibiotics, but their side chains are in a trans configuration in relation to the -lactam ring, which makes them much more resistant to hydrolysis by -lactamases and therefore much more active against a wide variety of bacteria. Compared with the structure of penicillins and cephalosporins, there are additional differences to the -thiazolidine ring and the side chain (Fig. 8-6). The three carbapenems currently available are imipenem (Primaxin), meropenem (Merrem), and ertapenem (Invanz).
The mechanisms of action of carbapenems are the same as that of penicillins and cephalosporins. The mechanisms of bacterial resistance are also the same, except that the trans ring configuration makes them poor substrates for nearly all -lactamases, so both inherent and acquired resistance is much less common. When resistance occurs, it is often due to decreased permeability of the bacterial cell, altered penicillin-binding proteins, or production of a particular -lactamase that has the ability to hydrolyze carbapenems.
The spectrum of activity of carbapenems includes streptococci, methicillin-susceptible staphylococci, ampicillin-susceptible enterococci, nearly all Gramnegative bacilli, and anaerobes. Notable exceptions are
Stenotrophomonas maltophilia, Burkholderia cepacia,ampicillinresistant enterococci, and methicillin-resistant staphylococci. Ertapenem is inactive against all Enterococcus spp. and Pseudomonas spp. Carbapenems should be used only for hospital-acquired, severe, or mixed infections, and not for routine empirical treatment of a patient requiring hospitalization of a mild or moderate infection.They cannot be given orally because they are hydrolyzed by stomach acid.
After administration, they enter all body tissues and fluids, except urine for imipenem. Upon reaching the kidneys, imipenem is hydrolyzed by a dehydropeptidase in the brush border of the proximal renal tubule cells. Its metabolites are also somewhat nephrotoxic. Therefore, commercially available imipenem is combined with a compound called cilastatin, which is a competitive
inhibitor of the dehydropeptidase. This prevents the hydrolysis of imipenem, allowing it to reach therapeutic concentrations in urine, and also eliminates its nephrotoxicity. Meropenem and ertapenem are not metabolized and do not need to be given with cilastatin. Excretion is similar to that of most penicillins and cephalosporins and is via the kidneys.
Side effects are also similar to those of penicillins and cephalosporins (including 1–5% hypersensitivity in patients who are allergic to penicillins and cephalosporins). Carbapenems can cause seizures when given at high doses, especially to patients with renal insufficiency or underlying abnormalities of the CNS. Unless there are no alternatives, one carbapenem should not be substituted for another if this happens.
MONOBACTAMS
Aztreonam (Azactam) is the only member of this class of antibiotics that is currently available. It is a monocyclic lactam ring to which a side chain identical to that of ceftazidime is attached (Fig. 8-7). Because it has only one ring, it is not a -lactam antibiotic.
Its mechanism of action is similar to that of penicillins, cephalosporins, and carbapenems. However, it primarily binds to penicillin-binding 3 of Gram-negative bacilli and does not bind to penicillin-binding proteins that are present in Gram-positive bacteria. Therefore, the spectrum of activity of aztreonam is limited to aerobic Gramnegative bacilli. Although this is very similar to the spectrum of aminoglycosides, these two classes of antibiotics are not interchangeable. Gram-negative bacteria can acquire resistance via the production of certain -lactamases that hydrolyze aztreonam.
Aztreonam is not absorbed from the gastrointestinal tract. From a pharmacokinetic perspective, it can be given intramuscularly, but its frequency of administration (every 6–8 hours) makes this too painful to be practical, so only intravenous administration is useful.Therapeutic levels are achieved in nearly all body tissues and fluids,
Figure 8–7 Structure of aztreonam.

118 CHAPTER 8 PRINCIPLES OF PHARMACOLOGY
including lungs and sputum,kidneys and urine,gallbladder, liver, bone, and prostate. Approximately 10% of aztreonam is hydrolyzed, presumably by hepatic enzymes, to yield metabolites that have the ring structure opened. Excretion is exclusively by renal mechanisms, via both glomerular filtration and tubular secretion.
The most common side effects are rashes. However, these are not due to immediate-type hypersensitivity. There is no cross-allergenicity between aztreonam and-lactams and no risk of anaphylaxis to aztreonam in patients who have a history of anaphylaxis to those agents.
GLYCOPEPTIDES
Despite being discovered 40 years ago, vancomycin has remained the only antibiotic in this class. It is a very large, complex glycopeptide structure with molecular weight of 1450 daltons (the unit of measure). It acts by inhibiting bacterial cell wall synthesis. It surrounds the C-terminal D-alanyl-D-alanine precursor of the polypeptide portion peptidoglycan, thereby preventing hydrolysis of the last D-alanine of the polypeptide and the simultaneous transfer of the precursor to the growing cell wall by alanine transferase.
Until several years ago, acquired bacterial resistance to vancomycin did not occur. However, some strains of enterococci now produce an enzyme encoded by a gene called van A, which synthesizes a C-terminal D-alanyl-D- lactate precursor, to which vancomycin is unable to bind. When the terminal D-lactate is hydrolyzed, the resulting peptidoglycan is indistinguishable from that of vancomycin-susceptible strains.
Several cases of infections due to strains of S. aureus that are only intermediately susceptible to vancomycin have been reported.This may be only the beginning of a potentially huge clinical problem. The mechanism of decreased susceptibility by S. aureus has not yet been elucidated. More recently, several infections caused by S. aureus that are resistant to vancomycin have occurred. The mechanism of resistance is via the same van A gene as in enterococci. Prolonged previous treatment with vancomycin has occurred in all patients who have developed infections due to vancomycin-intermediate and vancomycin-resistant staphylococci.
Vancomycin is active against nearly all Gram-positive bacteria, including Streptococcus spp., Enterococcus spp.,
Staphylococcus spp., Corynebacterium spp., Clostridium spp., Bacillus spp., Lactobacillus spp., and Listeria monocytogenes. Gram-positive exceptions include Leukonostoc spp., some strains of enterococci, and rare strains of S. aureus (as previously noted) and Staphylococcus haemolyticus. It is inactive against Gram-negative bacteria. Therefore, it
should be used when an infection due to methicillinresistant S. aureus is suspected or proven, or when an immediate-type allergy to -lactam antibiotics prevents the use of an antistaphylococcal penicillin.
Because it is a very large molecule, vancomycin is poorly absorbed. Intramuscular injections are too painful to be used for even a single dose.Therefore, except for the treatment of C. difficile colitis, it must be given intravenously.The usual dose of 1000 mg yields a peak serum concentration of 20 to 50 g/mL and a trough of 5 to 12 g/mL. Because of the relatively low toxic to therapeutic ratio, monitoring of trough levels should be performed to avoid side effects that are related to serum concentrations.
Adequate levels are achieved in skin, pleura, synovia, and other tissues that are susceptible to infection by Gram-positive bacteria. An exception to this general rule is the colonic lumen, which makes oral treatment necessary for C. difficile colitis.When being used to treat meningitis (e.g., due to methicillin-resistant S. aureus), additional intrathecal injections are sometimes necessary.
Vancomycin is excreted unchanged in urine via glomerular filtration, and therefore urinary levels are very high, but because it is not active against Gram-negative bacteria, they are usually irrelevant. The creatinine clearance of all patients who are to be given vancomycin should be calculated, because the dosage must be adjusted in patients with even mild renal insufficiency. In patients with renal failure who are on dialysis, it needs to be given only once every 2 to 7 days, depending on whether or not it is removed by the dialysis equipment being used (newer high-flux dialysis equipment removes large molecules, older machines do not).
If a dose is given too rapidly, flushing of the face and neck, sometimes accompanied by the “red man” or “red neck” syndrome, may occur. This is due to histamine release caused by local hyperosmolarity when a dose is given too rapidly, and is not an allergic reaction that precludes additional doses. Deafness may occur if serum levels are permitted to remain too high for a prolonged period. Older preparations of vancomycin were relatively impure and caused renal insufficiency. Many physicians mistakenly believe that vancomycin still can cause acute renal failure, but this is not a problem with the currently available preparations.
AMINOGLYCOSIDES
Because of resistance by Gram-negative bacilli to many sulfonamides and early penicillins, which were the first two classes of antibiotics to be discovered, microbiologists began to screen soil bacteria for the production of other
