
ЛЕКЦІЇ мод 3; 4; 5 укр рус англ / ЛЕКЦИИ 5 мод / АНГЛ / лекц 6 англ. 5к / лекц 6
.docxThe Ministry of health of Ukraine Higher state educational institution of Ukraine «Ukrainian medical stomatological Academy» Approved at the meeting of the Department surgical stomatology and maxillofacial surgery with plastic and reconstructive surgery of the head and neck Head of the Department,
doctor of med.s., Professor Avetikov D.S. METHODICAL DEVELOPMENT OF LECTURES
|
Academic discipline |
Surgical stomatology |
|
Module № 5 |
5 |
|
Module № 5 substantial |
5 |
|
The topic of the lecture |
Periodontal surgery.Muko-gingival plastic surgery. Surgical stages of dental implantation. Corrective operations. |
|
course |
V |
|
Faculty |
stomatological |
Number of training hours 2. Poltava - 2013 Scientific and methodological substantiation of topics. Among the directions of modern medicine dental (dental) implantology, rose in the middle of the XX century as a multidisciplinary specialty, thanks to its research intensity and интегративному potential is experiencing rapid development. Dental implant is great interest among specialists and attracts an increasing number of patients. In recent decades, this type of treatment is successfully applied, in particular, in Germany, where more than 1000 specialists dentists are trained and can make a prosthesis on implants at a high professional level. Research conducted with the purpose of improvement of this type of dental care, primarily related to the service life of the implant. Determined that an average of 92% of orthopedic constructions on dental implants are more than 10 years. Dental implantation is a relatively new branch of dentistry, which solves the problem of restoration of the anatomical form and function in different areas of the dental system through the introduction of tissue alloplastic materials. With the help of various implants can restore the continuity of the jaws, TMJ facial contours (maxillofacial implantology), or dental arch and individual teeth. 2. Educational entire lectures. - Provide a description of the basic stages of development of domestic and foreign dental implantology. - Classify the types of dental implants and methods of their introduction. - Justify the concept of "multidisciplinary approach" to the dental implant. - Classify different types of corrective surgery. To give a description of separate stages of surgical stage of dental implantation. - Demonstrate the basic kinds of surgical treatment of the atrophy of the jaws. Indicate the advantages and disadvantages of dental implantation. Purpose of the development of the personality of a future specialist, topical aspects. Introduction of a student in the clinic of maxillofacial and plastic surgery of the head and neck after a course of maxillofacial traumatology requires knowledge of ethical behavior and features of деонтологичного approach to patients with defects and deformations of the tissues of the head and neck, skills to use modern classifications, methods of examination and differential diagnostics to provide full, safe medical care.
4. Interdisciplinary integration.
|
The names of the previous disciplines |
skills |
|
1. ethics and deontology.
|
Install psychological contact with patients who have defects or tissue deformation of maxillofacial area. |
|
2. Health organization. |
Apply knowledge of the principles of the organization of surgical care in the Department of maxillofacial surgery and clinical examination. Issue the necessary documentation. |
|
3. Pathomorphology. |
Describe the nature of the pathological changes of anatomical structures in the presence of defects and distortion of fabrics Chairman and neck. |
|
4. Pathological physiology. |
To determine the etiology and pathogenesis of the wound process. |
|
5. Propedeutics of internal diseases. |
Write a general scheme of examination of the patient. To conduct supervision of the patient.
|
5. Plan and organizational structure of the lecture.
|
№ |
Main stages of lectures and their content |
Type lectures. The activation of students. Materials of methodical maintenance |
Distribution time |
|
1. |
The preparatory phase. Determining the relevance of the topic, educational goals and motivation. |
Introduction, clinical lecture with elements of reality.
|
5% |
|
2. |
The main stage. Teaching lecture material in the plan. 1. Description of the main stages of development of Russian and foreign dental implantology. 2. Known methods of substitution of Edentia. 3. Justification of the concept of "muko-gingival" plastic surgery. 4. Classification of different types of corrective operations. 5. The characteristic of separate stages of the planning of surgical stage of dental implantation. |
Clinical lecture with the use of clarity: multimedia support decision of problem situations, situational tasks, thematic patients. |
85% |
|
3. |
In the final step. Summary of lectures, General conclusions. Answers to the questions. The task for self-study students.
|
Training literature. Methodological development Department. The task for self-study. |
10% |
6. The content of the lecture material. Attempts to replace lost teeth fracture nails implants can be traced to the ancient civilizations of Egypt and South America. Examples of these are described in the ancient manuscripts of the sources and found the skeletal remains discovered by the archaeologists. So, in my skull, relating to the time before the discovery of America by Columbus and is now in the Museum of Harvard University, discovered an artificial tooth, carved from dark stone and replacing the lower-left side cutter. Keepers of the Museum believe now that this implant was made after the death according to the custom of South American Indians of those times. In this regard, in the opinion of M. Block, numerous references to the skull in the literature on the implantation of the teeth need to be adjusted. In a Museum in Peru is stored skull Inka with 32 teeth - implants made of quartz and amethyst. This surgery was performed in 800 years BC. Today the main condition of implantation is the use of inert materials for the manufacture of dental implant, do not induce immunological reactions. In modern dentistry is used titanium, gold, Nickel-chromium-vanadium alloys. Also are used in modern dentistry implants with porous powder coating, which is a bioactive that is due to porosity germination of bone tissue inside the implant is faster, and the implantation becomes more reliable. Porous composition of titanium powder, and then bioactive кирамики applied for titanium billet by plasma spraying. These inorganic constituents of bone tissue tend over time to disperse, actively encouraging the bone formation. The survival rate of such implants are considerably higher and stabilization of more reliable than any other.
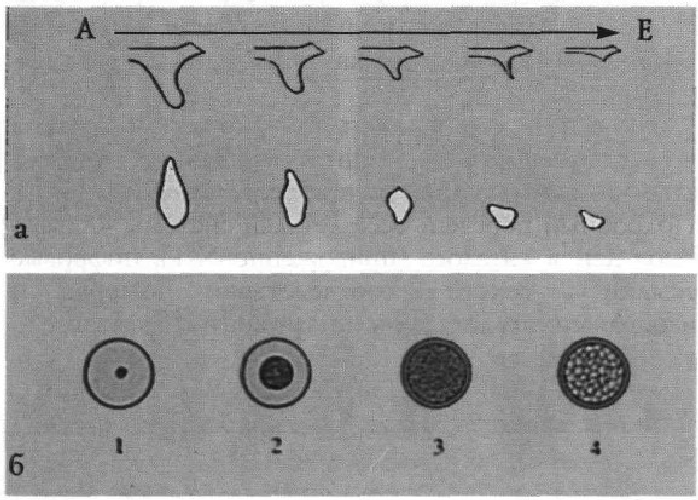
Types of dental(intraosseous) implants: On the surface of the intraosseous: smooth, structured photo, with bioactive coating. Material: metal, ceramic. In the method of application: one line-of-communication, two stages. The mechanism of osteogenesis implantation The concept of biocompatibility of a generalized and covers both influence the biological environment of the organism and direct reaction of the local tissues of the implant, and the effect of constant exposure to implant the surrounding tissues and the organism as a whole. There are three main variants of the organization of tissues on the surface of section implant+bone: 1. Direct contact with the bone implant surface of bone integration or osseointegration. 2. Indirect contact between the actual bone тканню and implant surface is formed a layer of connective tissue, consisting mainly of collagen fibers and fibered bone fibro-bone integration. 3. The formation of fibrous connective tissue on the surface of the implant (the connective-tissue integration) The first two options are functional response of bone tissue on the establishment and functioning of the implant. A third option is normal for compounds with a soft cloth, for example, mucous membranes, or stroma of bone marrow tissue spaces. The mechanism of achieving the bone integration is the contact osteogenesis, based on processes остеоиндукции and остеокондукции directly on the surface of the implant, and the ability of the bone to heal on the type of the primary tension. Fibro-bone integration is the result of distant osteogenesis based on the same processes. However остеоиндукция and остеокондукция is not on the implant surface and on the surface of the bone. In its biological essence distant osteogenesis is a bone healing by type of secondary tension. Contact and distant osteogenesis occurs in the following cases: 1. If the surface is made of biocompatible material implant no admixture of foreign material (no контоминации) and saved maintain the integrity of the oxide film or coating. 2. If the bone tissue of the receiving socket has not lost the ability to regenerate. Viability adjacent to the implant surface of the bone tissue is determined primarily by the absence of significant violations of the blood supply and severe damage to the structural units of the bone. After non traumatic preparation of the seedbed depth necrosis of bone tissue surrounding the implant is up to 500 microns. Moreover, the destruction of all osteocytes can occur only on the edge of the bed to a depth of 100 microns, while the border with necrosis zone throughout the remaining 400 microns part of osteocytes remains alive. 3. If there is close contact between the surface of the implant and bone tissue. Processes for contact and distant osteogenesis will occur when there is direct contact between the structural units of the bone and the implant surface adjoining trabekl or osteon is about 100 microns. Condition for остеокондукции is building strong attachment to the implant surface clot and bridging of fibrin fibers between the implant surface and a viable, preserving the osteoinductive properties of the bone tissue. Damage to bone capillaries, the preparation of the receiving bed causes bleeding. After implant in the bloody bone bed some blood gets into the surrounding tissue and on its surface, on which produces a protein film. In the formation of the film take part proteins and microelements blood plasma: fibrinogen, prothrombin, tromboplasty, glycoproteins, PDGF and IGF-protein, calcium ions, as well as cells, platelets, erythrocytes, leukocytes. Platelet aggregation causes the formation of a clot thrombosis and bleeding vessels. Part of the platelets stick to the collagen fibers of the bone tissue and the implant surface. Simultaneously with the aggregation of platelets through thromboplastin prothrombin turns into thrombin, which in turn provokes the polymerization fibrinoguena in fibrin fibers. The result is a vast network of thin fibrin fibers that are attached to the collagen fibers bones and capillary walls, and the other to the implant surface. Right after the establishment of the clot occurs his retraction. Contracting, clot reaches 10% of the initial volume. This is a critical moment for остеокондукции, because the stronger attachment of blood plasma proteins and fibrin fibers to the implant surface, the less number of the last leap from the surface of the implant and the greater the size of its surface will be covered matrix, which can occur proliferation and differentiation of osteogenic cells. The stage of contact osteogenesis: 1. Оsteoconduction. Proliferation of osteogenic cells during fibrin fibers and differentiation of these cells into osteoblasts. 2. Education bones de novo. Secretion of osteoblasts оsteopoetin, оsteonektin and collagen. 3. The formation of the line cement formation. The formation of crystals of calcium-phosphate compounds. Histological links between the surface of the implant and the mucosa, gums like зубодесневому connection, but differs organization of collagen fibers and blood vessels. Indications and contraindications for implantation established on the basis of General history taking and examination, evaluation and emotional condition and dental status of the patient. Indications for dental implantation are: 1. Single dentition defects, when implantation will avoid the preparation located near the defect of the tooth. 2. Involved defects of dentitions, when with the help of implantation can be avoided preparation limiting defect teeth and removable prosthetics. 3. End defects of dentitions in which implantation allows removable prosthetics. 4. Full edentulism, when with the help of implantation fixed prostheses can be made either to ensure a more reliable fixation of full dentures. There are a number of diseases which implantation, like any other elective surgery, is contraindicated. These include: 1. Chronic diseases in the stage of compensation. 2. Coagulation disorders and homeostasis. 3. HIV and any other serum positive infection. 4. Mental illness. There are also diseases, physiological and functional condition in which only at a certain period of time to perform any operation may cause harm to a patient, or in the period of state of the body would not achieve the positive results of the operational the intervention. These include: 1. Acute inflammatory diseases and acute viral infections. 2. Chronic infectious diseases (tuberculosis, actinomycosis and other). 3. Exacerbation of chronic diseases. 4. High risk of bacteriemic diseases (patients with prosthetic heart valves and had bacterial endocardit, rheumatism). 5. Recently transferred a heart attack or stroke. 6. Pregnancy or lactation. 7. Treatment with drugs that have an adverse effect tissue regeneration. 8. Endocrine pathology. As contraindications to the dental implantation should be considered osteopathy (primary and secondary osteoporosis, osteomalacia, and others). The proportions between compact and cancellous bone bone classified from 1 to 4; 1 means the situation when more compact bone, and 4 more spongy
(Fig. 1). Ideal for implantation of bone is a large bone, without the expressed resorption of bone in which there is a sufficient number of cortical bone, providing rapid healing and OS - teointegration. According to the study of biomechanics intraosseous implants, it is cortical bone of the jaw, contributes to the perception and distribution of loads. Therefore, the ideal bone is A2. After implantation should not be loading implants for 3 months at a jaw surgery and 6 months in the upper jaw to strengthen the implant into the bone. In this period, there is an interaction between osteoblasts and osteoclastami in the process of healing and bone integration. Premature disclosure of implant reduces the chances of success. Marked periods of 3-6 months is the minimum terms of «adjustment»with the «soft» bone it is necessary to extend the waiting period (osseointegration) up to the moment of the implant. The stage of contact osteogenesis: 1. Оsteokonduction. Proliferation of osteogenic cells during fibrin fibers and differentiation of these cells into osteoblasts. 2. Education bones de novo. 3. The formation of the line cement formation. The formation of crystals of calcium-phosphate compounds. Histological links between the surface of the implant and the mucosa, gums like gingival connection, but differs organization of collagen fibers and blood vessels. Indications and contraindications for implantation established on the basis of General history taking and examination, evaluation and emotional condition and dental status of the patient. Indications for dental implantation are: 1. Single dentition defects, when implantation will avoid the preparation located near the defect of the tooth. 2. Involved defects of dentitions, when with the help of implantation can be avoided preparation limiting defect teeth and removable prosthetics. 3. End defects of dentitions in which implantation allows removable prosthetics. 4. Full edentulism, when with the help of implantation fixed prostheses can be made either to ensure a more reliable fixation of full dentures. There are a number of diseases which implantation, like any other elective surgery, is contraindicated. These include: 1. Chronic diseases in the stage of compensation. 2. Coagulation disorders and homeostasis. 3. HIV and any other серопозитивная infection. 4. Mental illness. There are also diseases, physiological and functional condition in which only at a certain period of time to perform any operation may cause harm to a patient, or in the period of state of the body would not achieve the positive results of the operational the intervention. These include: 1. Acute inflammatory diseases and acute viral infections. 2. Chronic infectious diseases (tuberculosis, actinomycosis and other). 3. Exacerbation of chronic diseases. 4. High risk of bacteriemic diseases (patients with prosthetic heart valves and had bacterial endocardit, rheumatism). 5. Recently transferred a heart attack or stroke. 6. Pregnancy or lactation. 7. Treatment with drugs that have an adverse effect tissue regeneration. 8. Endocrine pathology. As contraindications to the dental implantation should be considered osteopathy (primary and secondary osteoporosis, osteomalacia, and others). The proportions between compact and cancellous bone bone classified from1to 4; 1 means the situation when more compact bone, and 4 more spongy (Fig. 1). Ideal for implantation of bone is a large bone, without the expressed resorption of bone in which there is a sufficient number of cortical bone, providing rapid healing and OS - теоинтеграцию. According to the study of biomechanics intraosseous implants, it is cortical bone of the jaw, contributes to the perception and distribution of loads. Therefore, the ideal bone is A2. After implantation should not be loading implants for 3 months at a jaw surgery and 6 months in the upper jaw to strengthen the implant into the bone. In this period, there is an interaction between osteoblasts and osteoclastami in the process of healing and bone integration. Premature disclosure of implant reduces the chances of success. Marked periods of 3-6 months is the minimum terms of «adjustment»with the «soft» bone it is necessary to extend the waiting period (osseointegration) up to the moment of the implant.
Features of carrying out of implantation in the upper jaw. - the lower wall of the sinus uneven, and there are concave and convex region. On a panoramic x-ray of sinus bottom wall looks completely smooth, but this is because a snapshot is a copy of the two-dimensional volumetric picture. So sometimes the x-ray picture, you can see that the implant is of sinus. Actually the bottom of the implant can be placed in the thickness of the wall of sinus. In some cases, the low location of the sine implantation is possible, because cortical plate of the bottom wall of the sinus is able to support the implant, distributing forces acting on it the entire length of the cortical bone; - in the base of the nose is thick bone, which can become a good support for the implant and distributes the forces on the implant, along cortical plate upper jaw; - region Fossa Canine has in most cases enough bone for implant (if you cannot enter enough implants for a fixed prosthesis, you can make the denture, which will rely on implants placed in this area); - in palatal site should beware hurt great Palatine artery (in the case of injury to squeeze artery and suturing it); - sometimes there are the need to make implantation in tuberal region and rely on Fossa Pterigoidea. Bone on this site, as a rule, soft Round 4, and we must be careful not to fall in Fossa Sphenopalatine, which is very rich in blood vessels and nerve endings. Features of the implantation on the lower jaw - mandibular the neurovascular bundle can be located and buccal and лингвально in the body of the mandible; - to determine the position of мандибулярного nerve, it is necessary to trace its path on the panoramic shot with the area of his entry in the lower jaw to the mental hole; - mandibular nerve exits the temporomandibular channel in the mental hole, which is usually located between premolar teeth of the lower jaw. Part mandibular nerve goes forth, for the mental hole inside the channel towards the front teeth and called (incisive nerve). Damage it usually does not entail problems, it rarely causes paresthesia, continued for several months; - trajectory mandibular nerve before he comes out of the mental openings, several times is bent in the form of loops in the direction of the front surface of the jaw. It is very important to see the loop and not to mix it with the channel incizive nerve. Damage to the hinges would entail the loss of sensitivity. - in retromolar plot of the x-ray picture shows two boundary vertices of the alveolar process: the buccal and lingual cortical plates. When determining the size of the implant need to focus on the bottom of them. Before implantation, must draw up its program, plan of examination and treatment, answering the following questions: Whether this clinical case suitable for implantation? Is there a need for additional special medical examination and an examination? What are the desired plans patient recovery dentition? Where exactly to put implants? What number of implants you need to install? What is the length of the implant in each case and the site of implantation? What is the diameter of the implant in each case? We need to get acquainted with the patient in terms of cognitive and psychological features, level of oral hygiene, the possibility of mutual understanding. Also need to consider the complaints of the patient, what they expect from treatment with aesthetic and functional points of view. During the examination of the oral cavity it is important to pay attention to: - the state of soft tissues: the height and the position of the fixed mucous (аttached gingiva), fabric color, thickness of gums, pathological areas and the status of salivation; - the condition of the teeth: dental caries, periodontal status, tooth mobility, density and inclination of teeth, hygiene of mouth cavity; - state of the alveolar process, not having teeth: height, width, shape, and also the presence of roots destroyed the teeth. You should carefully study the aesthetic and the functional state of the dentition status of the temporomandibular joints prior to treatment. It is necessary to collect detailed medical history of the General health of the patient, if necessary, to get clarification of a family doctor.
The operation of implantation can be divided into several stages: - preparing the patient for implantation, - verify the health of the necessary instruments and equipment; - conduction anesthesia; - raising the flap and exposure of the important anatomical areas, such, such as the mental eye; - designation of bones with the help of direct or round surgical boron desired place implantation; - initial preparation of bone at a depth of less than planned; - introduction of the meter length and monitoring parallelism productions implant; - continuation of the preparation of the first drill to the length required after the checkpoint x-ray; - continuation of the development of the implant bed the following drills in accordance with the selected type of implant; - installation of the meter length and carrying out control dental x-ray; - installation of the implant; - closing of the implant cover screw in the technique of Two Phases or closing abutments when One technique Phases; - closure of mucous membrane; - if necessary snapshot after implantation (or panoramic dental x); - monitoring after implantation; -disclosure of the implant when the two-step method of implantation. At breaking away слизистонадкостничного flap incision should be made in the Attached Gingiva, i.e. fixed and not in the mobile mucosa of the alveolar ridge. You can make the cut Middle - Crest on top of the alveolar process or slightly вестибулярно or лингвально (Fig. 4). Recommended incision little лингвально; thus at laying seams implant will be fully covered by mucous membrane, and the seam will not be placed above it. Thus, reduce the risk of uncovering the implant and infections. It is recommended to raise the wider area of the mucous membrane and trace the direction of a bone, its size, defects. It is necessary to ensure a good blood supply to отслоенного area of mucous membrane.
Manipulation on the mucous membranes and bone tissues of the oral cavity. At present, developed surgical techniques, which allowed to considerably expand the indications to intraosseous implantation or improve its results. They are produced in the process of preparation for implantation, during the operation of implantation or after it. These procedure is not recommended for a beginner in the field of implantology doctor, and some of them are recommended in the Department of maxillofacial surgery. In many cases, the form and state of the bone does not allow the installation of the long and wide implants in the optimum location at the optimal angle and get good aesthetic results. It is possible that the alveolar ridge low and narrow, the dice have any defects, or top of the alveolar ridge is located under the strong щечным angle. To solve these problems, we have developed a special methodology.
Aimed of a bone regeneration. As a rule, bone tissue defect on the border with the mucous membrane is filled with connective tissue or epithelium, not bone. This is because the connective tissue and epithelium regenerate several times faster than bone, and therefore they «win» in the competition for filling in the spaces. It is established that barrier (partition) before connective tissue and epithelium creates an opportunity for bone regeneration of the defect. Partition (membrane) is a thin strip of material, placed under the gums to the bone. Using different types of membranes. The most common: - membrane Gore Those is a membrane made of резорбируемого polymer that is absorbed. It is of oval form three different sizes. When denudation membrane easily destroyed; - membrane Kolagen consists of a synthetic collagen, which is part of the bones and connective tissues. Membrane made in the shape of a square and it goes with a sheet to cut membranes required form; - membrane Laminal Bone (LAMB) is a membrane from dried frozen bones. Membrane made of human bones, which took place sterilization and special handling and contains substances that stimulate growth of bone. It is immersed in water and put on the desired area; - polymer membrane Vicril - rezorbl membrane consisting of polymer, similar in composition to the collagen; - titanium diaphragm (№ 305) - non resolve membrane made of pure titanium. It has a number of advantages: fast is not polluted; its price is 15% of the price of collagen membrane; you can give the necessary rounded shape by means of surgical instruments. Installation of membranes during surgery can be done in several ways: - the membrane is bonded to the periost (membranes are made of titanium is not suitable); - membrane strengthened small titanium screws. For this there are two kinds of screws: a) fixing screw diaphragm - screw is screwed through the membrane into the wall of the bone defect. Before screw in the screw is not - large hole drill the screw, and establish the membrane with the help of key 1,25. If we compare the membrane with a tent, the screw will perform the role of the wedge (peg) for tents; b) support screw screw is screwed into the depth of the bone defect. Before screw in the screw, made a small hole drill the screw. After setting of the reference screws fasten the membrane, placing it upon the reference screw and screwing it on edges of additional fastening screws. If we compare the membrane with a tent, support screw will perform the role of a pole for a tents; - membrane is fixed with the help of the closing screws (cap) for the implant if implantation was performed simultaneously with the installation of the membrane. You should make a hole in the membrane over the implant and screw in the screw through the membrane into the implant. Then it is necessary to strengthen the membrane additional screws. The membrane should not touch the adjacent teeth, so as not to disrupt ermetic fit to the teeth gums. The success of the process of building (thickening) bone is provided by filling of space or cavity under the membrane material to stimulate bone growth. It also prevents breaking through membranes inside the cavity. Developed several opportunities to fill the cavity: 1. Autograft bone is taken from the patient. The results of application of such bones are very good. When you need a small amount of bone, you can use the jaw bone. The most common place to take the tissue of the jaw: - bone below the lower front teeth. With vestibular the surface should be to retreat at least 5 mm below from апексов roots lower teeth; - bone of retro mandibular plot; - interdental bone partitions; - pieces of bone, protruding in the places of the missing tooth or between the teeth. - fragments of bones collected in the process of preparation of the bone. For this you need to set in saliva ejector special filter that collects the fragments of bone. Perhaps the use of bone from other parts of the human body. The most common sites are the iliac crest bone and ribs. The bone can be taken in the form of blocks and in the same form to enter in a defect - this form of transplantation is called inlay (tab) bones. 2. Allograft (Homograft) - bone of human origin. Bones are sterilized, ground and subjected to special treatment. This material is called Demineralized Freeze Dried Bone (D. F. D. Century) - dried frozen bone, passing the process of demineralization. The necessary amount is 0,25 cm3, for small defects, to fill holes remote teeth required and 1.0 0.5 cm3 cm3 for the larger sites or multiple sites. The material is produced as powder. Particles of a powder come in two sizes: 250 to 500 microns (№ 308) and 500 to 1,000 microns. DFDB supplied in a sterile package 1.0 and 0.5 cm3. Selected natural protein that stimulates the growth of bone - Bone Morphologic Protein (B.M.P.). To get micrograms of this product requires many pounds of bone, and therefore the material is very expensive. Being developed to create this material with the help of genetic engineering. 3. Xenograft - bone of an animal origin. For example, Bovines Bone - bone cattle, grind into a powder; - bone pigs, held deproteinization bearing mineral structure. 4. Alloplast - bone of synthetic origin. Its purpose is to influence a osteoclasts, so that they utilized the artificial bone and contributed to the growth of normal bone instead of the artificial. To the materials of synthetic origin refers hydroxyapatite. Granules of hydroxyapatite Hydroxyapatit (H.A) produced by 0,5; 0,75; 3,0 cm3. Rezorbl form of synthetic materials preferable not resorbable. 5. A blood clot in the blood are prognator, cells for building bone, and the presence of a blood clot in the regeneration section is mandatory. Each company claims that its material gives the best results. However, it is doubtful that any material gives good results without the presence of a blood clot. It is believed that the bone of the patient and B. M. R. yield the best results. Many doctors use a mix of several materials such as autogenic bone + D. F. D. Century + N. A. + blood. Usually оsteoplastic material placed under the membrane, but if you have a small defect, the membrane is not used, but care should be taken to place of operation was hermetically closed. Before placing the material make a hole (perforation) in the bone on this site, that speeds up the interaction of the material, bone marrow and blood. Stitches over membranes has its own peculiarities. When the sutures over the membrane should be full hermetic sealing of the membrane to prevent contamination. It is very important to the operation place, we have not created voltage for better healing and create aesthetically pleasing good appearance. In many cases, not enough soft cloth to sew it without tension, therefore, must make cross laxative sections with the internal surface of the mucoperiosteal flap. Incisions allow the tissue to stretch. Featured seams are horizontal and vertical mattress suture. Unfortunately, from 25% to 60% of newly formed bone undergoes a process of reverse resorption. When there is a narrow alveolar ridge (3 mm), you can apply the technique of splitting the alveolar ridge. With the help of various bits split (split) vestibular and oral cortical plate on top of the ridge on the depth of 4-8 mm Vestibular plate deflected to the side and match the dimensions of the drill for implants, create a bed for implants (with the broad basis of the alveolar ridge is possible to use a drill for implants instead остеотомов). Then, as a rule, use membrane technology.
The raising of the maxillary sinus (Sinus Lifting) The main limitation in carrying out of implantation in the upper jaw is low wall of sinus. Very often the height of the bone under the lower wall of the sinus is small and does not establish long implants. This situation arises from the resorption of the alveolar bone and function of a sinus (sinus down); both of these processes occur after tooth removal. Bone located under the wall of the sinus divided by height on 3 groups: - more than 10 mm - produce implantation in a usual way; - between 8-10 mm - establish gently implants height 10 mm, immersing them on 1-2 mm in sinus under a mucous membrane. Bone wall of the sinus slightly перфорируется and installed implants method intercortical fixation; - less than 8 mm - is a surgical procedure which allows the increase of the thickness of the wall of the sinus space sinus. Sequence for surgery Sinus lifting: - exfoliate wide vestibular plot mukosubperiostel flap, vertical cuts are made in the mucous layer 4 and 7 of the teeth in the upper jaw. The incision for exfoliation of the flap should be done along the alveolar ridge with a shift in the Palatine area to get by hermetic closure after the end of the operation; cautiously, using hog stands out in the vestibular wall of the sinus bone region 1 cm width and height of 0.7 see The integrity of the слизис - the shell sine is not disturbed and the bone fragment is not separated from the sinus mucosa. It is necessary to ensure that the outline of the cortical bone was moving; - then you must push the lower part of the bone fragment upwards and inwards so that its upper part serves as the axis. Indentation is made carefully and in his bare exfoliate sinus mucosa. Raising the mucosa is done by special instruments in the form of quret spoons, bent at different angles. At the end of the indentation of a bone fragment turns into the lower wall of the sinus and creates a space between it and the old wall of the sinus. Sinus thus decreases; - the space formed through the window in the vestibular wall of the sinus is filled osteotrohic materials; implants are installed simultaneously, provided that there is enough natural jaw bone under the sinus to create the initial fixation of the implant (at least 5-6 mm bones); - close the vestibular window using any of the membrane, as described above; - produce tight stitches on a mucous membrane; - make a break 9 months at least before implantation (or disclosure implants, if the implantation is made together with the raise of the sinus). After implantation in перестроившуюся bone also follows a period of 9 months before the disclosure of the implant. Developed methodology micro Sinus Lifting, and new variants of the standard operations sinus lift
Change of location neurovascular. One of the main limitations of implantation in the lower jaw is a small bone height above the mandibular characters nerve. In this situation, you can consider moving the neurovascular and installation of implants using the whole height of the jaw. Clean the bone tissue in the form of 2-3 Windows (or the entire length along the projection of neurovascular, ranging from mental openings. Gently tighten the neurovascular bundle through the window created and thus giving the space for installation of the implant. After consistently installed implants, lay rezorbl membrane between implants and surrounding areas neurovascular bundle. Then impose membranes on the outer surface of the neurovascular bundle and suture. This procedure is complex and requires good skills of the doctor, because there are often paresthesia, and anesthesia after surgery. Change of location of neurovascular.One of the main limitations of implantation in the lower jaw is a small bone height above the mandibular characters nerve. In this situation, you can consider moving the neurovascular and installation of implants using the whole height of the jaw. Clean the bone tissue in the form of 2-3 Windows (or the entire length along the projection of neurovascular, ranging from mental openings. Gently tighten the neurovascular bundle through the window created and thus giving the space for installation of the implant. After consistently installed implants, lay резорбируемые membrane between implants and surrounding areas neurovascular bundle. Then impose membranes on the outer surface of the neurovascular bundle and suture. This procedure is complex and requires good skills of the doctor, because there are often paresthesia, and anesthesia after surgery.
7. Materials activization of students during the teaching lectures. Tasks for self-control: 1. Patient 23 years, went to see the surgeon-dentist with complaints about the lack of contact between the front group of teeth. Objectively: the contact is saved on the first premolar. Specify specialists to optimize treatment planning? (Answer: to optimize patient with such disorders requires a multidisciplinary approach.) 2. With the doctor, dentist, the patient is 21 years. Anterior genal tubercle first molar teeth of the upper jaw is located in fissure on the side (buccal) surface of the first molar teeth of the lower jaw. Specify the class bite according to the classification by Engl. (Answer: first class) 3. Increasing the angle ANB more 4 OC corresponds to what class of malocclusion according to the classification by Engl? Answer: (skeletal anomaly bite of the II class) 4. What angles are relatively easy to identify and are the main source of information for the analysis of the relationship of the upper and lower jaws? (Answer: the corners of the SNA, the SNB, ANB) 5. The doctor dentist asked the patient 19 years. Objectively: expressed protrusion of the lower jaw forward, the upper jaw in the position retruzn.
Anterior genal tubercle first molar teeth of the upper jaw is distal than normal. What is the most likely diagnosis. (Answer: Anterior bite III class, skeleton) Educational objectives the 3rd level (nonstandard tasks) : 1. Patient went to see the surgeon dentist with complaints aesthetic defect, snoring, which appeared more than 10 years ago. An objective study found a reduction of the lower jaw, front segment of the upper jaw in the position of protrusion. When conducting цефалометрического analysis was calculated angle ANB which was 5 degrees. Specify a preliminary diagnosis. What should be the doctor's tactics? What additional methods of examination should I apply? (Answer: skeletal anomaly bite II class, multidisciplinary approach to the processes of diagnosis and treatment planning. 2. To oral surgeons sent a patient with a preliminary diagnosis: outdoor class III malocclusion (III class) skeletal form. The decision of combined treatment. What projections should be made for the full фотодокументального analysis? (Answer: you should make not less than five photos: front, right, left and two in oblique projections. In addition, you should make a snapshot in subcheen projection and a photo bite closeup side and front. 3. Patient turned to the dental surgeon in connection with the fact that he had after the orthognathic surgery arose night snoring (sleep apnea). From an anamnesis: an operation was carried out on the lower jaw method Obwegeser. Diagnosis before the operation class III malocclusion (III class) skeletal form. Specify the possible error in the surgical treatment. (Answer: to avoid the above-mentioned complaints should be bimaxillary operation). 8. Materials for students ' preparation for lectures. The theme of which is set out in the lecture. 1. Sukachev V. A. Atlas of reconstructive operations on the jaws. /VA Sukachev// M, Medicine, 1984, 120 p. 2. Surgical dentistry and maxillofacial surgery: підручник; in 2 so - So-1 /V.O. Маланчук, O. S. Воловар, І.Ю.Гарляускайте and others - K.: LOGO, 2011. - 672с. + 16 ст.кольор.вкл. 3. Plastic and reconstructive surgery of the face / Ed. by A.D. Пейпла// M.: BINOM. 2007. - 951с. Question and assignment: 1. Historical aspects of formation of plastic, reconstructive surgery, as a science. 2. Goals and tasks at the modern stage. 3. The basic principles that guide the conduct of orthognathic operations. 4. Classification of defects and deformations of jaws. 5. Group jaw deformities. 6. Indications and contraindications to ortognatic operations. 7. The main bone guiding line when conducting cefalometric analysis. 8. Positive and negative sides of orthognathic operations. 9. Concepts of multudicipline approach in orthodontic surgery. 10. Conditions for successful execution of the operation. 11. Prevention of early complications. 12. Prevention of late complications. Materials for test control: 1. Among intraosseous dental implants are: A. Endodonto-endoossal and endoossal. B. Endoossal and over bone. C. Mono implants and combined. D. Submucosal and subperiosteal. E. All listed. 2. That refers to an absolute contraindications for dental implantation? A. Endocrine diseases. B. Neurological and endocrine diseases. C. Autoimmune and allergic diseases. D. All of the answers correct. E. Correct answer is no. 3. The advantages of flat (laminar) implants does not apply: A. Small depth of immersion of the implant into the bone. B. Possibility with great accuracy instrumental create bone bed. C. Possibility to install along with the natural teeth and include them as supports for orthopedic constructions. D. All of the answers correct. E. Correct answer is no. 4. Rasmus implant is: A. Implant, which is fixed underperiosteum. B.Inmucous implant. C. Bioactive implant. D. Design with cushion system. E. Flat design that is recorded in three places lower jaw. 5. What are dental implants are used most frequently? A. In osseus implants. B. Subperiosteal implants. C. Combined implants. D. Over osseous implants. E. All the answers to be correct. 6. That is not related to anatomical risk in implantology? A. The risk to injure the anatomic structure during the operation. B. The risk of lack of osseointegration. C. Risk creating a situation of temporary or constant discomfort. D. The risk of bleeding during surgery. E. The risk of injury is not adequate with the volume of intervention when installing the implant. 7. That is the advantage of the use of titanium alloys in dental implantation? A. High corrosion resistance and biological activity. B. High corrosion resistance and bio- tolerance. C. The chance to design any shape. D. The material in patients with blood diseases. E. All the answers to be correct. 8. Metal, which is used for intraosseous implantation and is practically the full analogue of titanium? A. Molybdenum. B. Nov. C. Zinc. D. Zirconium. E. Gidrargirum. 9. What factors do not affect the osseointegration of the implant? A. Material and shape of the implant. B. The degree of preparation of the bone bed. C. Compliance with the rules of aseptics. D. Time. E. Type of anesthesia. 10. That is an indication for dental implantation? A. Unit defects of the dentition. B. Involved defects of dentitions. C. End defects of dentitions. D. Full edentulism. E. All the answers to be correct. (Correct answers: 1 - A, 2 - C, 3 - B, 4 - E, 5 - A, 6 - D, 7 - B, 8 - D, 9 - E, 10 - E.) The topic of the next lecture. Standards answers: 1, 2. - D, 3 -, 4 -, 5 -, 6 - Year, 7 - B, 7 - D, 8 - B, 9 -, 10 -. 9. The used literature:
-
Barnes I E, Surgical Endodontics corrected reprint (MTP Press: Lancaster 1991).
-
Howe G L, Minor Oral Surgery, 3rd edn (Wright: Bristol 1985).
-
MacGregor A J, The Impacted Lower Wisdom Tooth (Oxford University Press: Oxford 1985).
-
McGowan D A, Baxter P W and James J, The Maxillary Sinus(Wright: Oxford 1993).
-
Seward GR, Harris M, McGowan D A, Killey H C and Kay L W, An Outline of Oral Surgery (Wright: Oxford 1998).
