
- •Preface
- •Contents
- •Procedures, Assays, and Normal Values
- •Normal Cells of the Blood and Hematopoietic Organs
- •The Individual Cells of Hematopoiesis
- •Bone Marrow: Cell Composition and Principles of Analysis
- •Abnormalities of the White Cell Series
- •Predominance of Mononuclear Round to Oval Cells
- •Prevalence of Polynuclear (Segmented) Cells
- •Erythrocyte and Thrombocyte Abnormalities
- •Hypochromic Anemias
- •Normochromic Anemias
- •Hyperchromic Anemias
- •Erythrocyte Inclusions
- •Thrombocyte Abnormalities
- •Cytology of Organ Biopsies and Exudates
- •Lymph Node Cytology
- •Branchial Cysts and Bronchoalveolar Lavage
- •Cytology of Pleural Effusions and Ascites
- •Cytology of Cerebrospinal Fluid
- •Introduction to the Physiology and Pathophysiology of the Hematopoietic System
- •Cell Systems
- •Principles of Regulation and Dysregulation in the Blood Cell Series and their Diagnostic Implications
- •Procedures, Assays, and Normal Values
- •Taking Blood Samples
- •Erythrocyte Count
- •Hemoglobin and Hematocrit Assay
- •Calculation of Erythrocyte Parameters
- •Red Cell Distribution Width (RDW)
- •Reticulocyte Count
- •Leukocyte Count
- •Thrombocyte Count
- •Significance of the Automated Blood Count
- •Bone Marrow Biopsy
- •Lymph Node Biopsy and Tumor Biopsy
- •Step-by-Step Diagnostic Sequence
- •The Individual Cells of Hematopoiesis
- •Eosinophilic Granulocytes (Eosinophils)
- •Basophilic Granulocytes (Basophils)
- •Monocytes
- •Lymphocytes (and Plasma Cells)
- •Megakaryocytes and Thrombocytes
- •Bone Marrow: Medullary Stroma Cells
- •Abnormalities of the White Cell Series
- •Predominance of Mononuclear Round to Oval Cells
- •Reactive Lymphocytosis
- •Relative Lymphocytosis Associated with Granulocytopenia (Neutropenia) and Agranulocytosis
- •Monocytosis
- •Acute Leukemias
- •Neutrophilia without Left Shift
- •Reactive Left Shift
- •Osteomyelosclerosis
- •Elevated Eosinophil and Basophil Counts
- •Clinically Relevant Classification Principle for Anemias: Mean Erythrocyte Hemoglobin Content (MCH)
- •Hypochromic Anemias
- •Iron Deficiency Anemia
- •Hypochromic Infectious or Toxic Anemia (Secondary Anemia)
- •Hypochromic Anemia with Hemolysis
- •Normochromic Anemias
- •Normochromic Hemolytic Anemias
- •Cytomorphological Anemias with Erythrocyte Anomalies
- •Bone Marrow Aplasia
- •Hyperchromic Anemias
- •Erythrocyte Inclusions
- •Hematological Diagnosis of Malaria
- •Thrombocyte Abnormalities
- •Thrombocytopenia
- •Lymph Node Cytology
- •Sarcoidosis and Tuberculosis
- •Non-Hodgkin Lymphoma
- •Metastases of Solid Tumors in Lymph Nodes or Subcutaneous Tissue
- •Branchial Cysts
- •Cytology of Pleural Effusions and Ascites
- •Cytology of Cerebrospinal Fluid
- •References
- •Index

86 Abnormalities of the White Cell Series
Relative Lymphocytosis Associated with Granulocytopenia (Neutropenia) and Agranulocytosis
Neutropenia is defined by a decrease in the number of neutrophilic granulocytes with segmented nuclei to less than 1500/µl (1.5 #109/l). A neutrophil count of less than 500/µl (0.5 #109/l) constitutes agranulocytosis. Absolute granulocytopenias with benign cause develop into relative lymphocytoses.
In the most common clinical picture, drug-induced acute agranulocytosis, the bone marrow is either poor in cells or lacks granulopoietic precursor cells (aplastic state), or shows a “maturation block” at the myelo- blast–promyelocyte stage. The differential diagnosis of pure agranulocytosis versus aplasias of several cell lines is outlined on page 146.
Classification of Neutropenias and Agranulocytoses
1.Drug-induced:
a)Dose-independent—acute agranulocytosis. Caused by hypersensitivity reactions: for example to pyrazolone, antirheumatic drugs (anti-inflammatory agents), antibiotics, or thyrostatic drugs.
b)Relatively dose-dependent—subacute agranulocytosis (observed for carbamazepine [Tegretol], e.g. antidepressants, and cytostatic drugs).
c)Dose-dependent—cytostatic drugs, immunosuppressants.
2.Infection-induced:
a)E.g., EBV, hepatitis, typhus, brucellosis.
3.Autoimmune neutropenia:
a)With antibody determination of T-cell or NK-cell autoimmune response
b)In cases of systemic lupus erythematosus (SLE), Pneumocystis carinii pneumonia (PCP), Felty syndrome
c)In cases of selective hypoplasia of the granulocytopoiesis (“pure white cell aplasia”)
4.Congenital and familial neutropenias:
Various pediatric forms; sometimes not expressed until adulthood, e.g. cyclical neutropenia
5. Secondary neutropenia in bone marrow disease:
Myelodysplastic syndromes (MDS), e.g., acute leukemia, plasmacytoma, pernicious anemia
Bone marrow diagnosis is indicated in cases of unexplained agranulocytosis
 a
a
 b
b
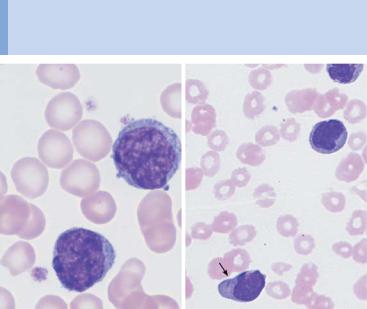
Fig. 29 The bone marrow in agranulocytosis. a In the early phase of agranulocytosis the bone marrow shows only red cell precursor cells (e.g., 1), plasma cells (2), and lymphocytes (3); in this sample a myeloblast—a sign of regeneration—is already present (4). b Bone marrow in agranulocytosis during the promyelocytic phase, showing almost exclusively promyelocytes (e.g., 1); increased eosinophilic granulocytes (2) are also present.
87
88 Abnormalities of the White Cell Series
Monocytosis
If mononuclear cells stand out in showing an unusually elaborate nuclear structure with ridges and lobes and a wider cytoplasmic layer with very delicate granules (for characteristics see p. 46, for cell function, see p. 6), and this is in the context of relative ("10%) or absolute monocytosis (cell count "900/µl), a series of possible triggers must be considered (Table 12). If the morphology does not clearly identify the cells as monocytes, then esterase assays should be done in a hematological laboratory using unstained smears.
Table 12 Possible causes of monocytosis
Infection
Nonspecific monocytosis occurs in many bacterial infections during recuperation from or in the chronic phase of:
–Mononucleosis (aside from stimulated lymphocytes there are also monocytes)
–Listeriosis
–Acute viral hepatitis
–Parotitis epidemica (mumps)
–Chickenpox
–Recurrent fever
–Syphilis
–Tuberculosis
–Endocarditis lenta
–Brucellosis (Bang disease)
–Variola vera (smallpox)
–Rocky mountain spotted fever
–Malaria
–Paratyphoid fever
–Kala-azar
–Thypus fever
–Trypanosomiasis (African sleeping sickness)
Chronic reactive condition of the immune system, e. g., in:
–Autoimmune diseases
–Chronic dermatoses
–Regional ileitis
–Sarcoidosis
Paraneoplasm
(as attempted immune defense),
e.g., in:
–Large solid tumors
–Lymphogranulomatosis
Neoplasm
–Chronic myelomonocytic leukemia (CMML, p. 107)
–Acute monocytic leukemia (p. 100)
–Acute myelomonocytic leukemia (p. 98)
Conspicuously large numbers of monocytes usually indicate a reactive disorder. Only a monotonous predominance of monocytes suggests leukemia
a |
b |
 c
c
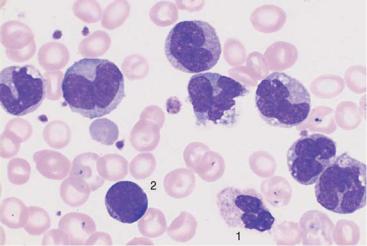
Fig. 30 Reactive monocytosis and monocytic leukemia. a Reactive and neoplastic monocytes are morphologically indistinguishable; here two relatively condensed monocytes in reactive monocytosis are shown. b Whenever monocytes are found exclusively, a malignant etiology is likely: in this case AML M5b according to the FAB classification (see p. 100). Auer bodies (arrow). c Monocytes of different degrees of maturity, segmented neutrophilic granulocytes (1), and a small myeloblast (2) in chronic myelomonocytic leukemia (CMML, see p. 107).
89
