
- •Preface
- •Contents
- •Procedures, Assays, and Normal Values
- •Normal Cells of the Blood and Hematopoietic Organs
- •The Individual Cells of Hematopoiesis
- •Bone Marrow: Cell Composition and Principles of Analysis
- •Abnormalities of the White Cell Series
- •Predominance of Mononuclear Round to Oval Cells
- •Prevalence of Polynuclear (Segmented) Cells
- •Erythrocyte and Thrombocyte Abnormalities
- •Hypochromic Anemias
- •Normochromic Anemias
- •Hyperchromic Anemias
- •Erythrocyte Inclusions
- •Thrombocyte Abnormalities
- •Cytology of Organ Biopsies and Exudates
- •Lymph Node Cytology
- •Branchial Cysts and Bronchoalveolar Lavage
- •Cytology of Pleural Effusions and Ascites
- •Cytology of Cerebrospinal Fluid
- •Introduction to the Physiology and Pathophysiology of the Hematopoietic System
- •Cell Systems
- •Principles of Regulation and Dysregulation in the Blood Cell Series and their Diagnostic Implications
- •Procedures, Assays, and Normal Values
- •Taking Blood Samples
- •Erythrocyte Count
- •Hemoglobin and Hematocrit Assay
- •Calculation of Erythrocyte Parameters
- •Red Cell Distribution Width (RDW)
- •Reticulocyte Count
- •Leukocyte Count
- •Thrombocyte Count
- •Significance of the Automated Blood Count
- •Bone Marrow Biopsy
- •Lymph Node Biopsy and Tumor Biopsy
- •Step-by-Step Diagnostic Sequence
- •The Individual Cells of Hematopoiesis
- •Eosinophilic Granulocytes (Eosinophils)
- •Basophilic Granulocytes (Basophils)
- •Monocytes
- •Lymphocytes (and Plasma Cells)
- •Megakaryocytes and Thrombocytes
- •Bone Marrow: Medullary Stroma Cells
- •Abnormalities of the White Cell Series
- •Predominance of Mononuclear Round to Oval Cells
- •Reactive Lymphocytosis
- •Relative Lymphocytosis Associated with Granulocytopenia (Neutropenia) and Agranulocytosis
- •Monocytosis
- •Acute Leukemias
- •Neutrophilia without Left Shift
- •Reactive Left Shift
- •Osteomyelosclerosis
- •Elevated Eosinophil and Basophil Counts
- •Clinically Relevant Classification Principle for Anemias: Mean Erythrocyte Hemoglobin Content (MCH)
- •Hypochromic Anemias
- •Iron Deficiency Anemia
- •Hypochromic Infectious or Toxic Anemia (Secondary Anemia)
- •Hypochromic Anemia with Hemolysis
- •Normochromic Anemias
- •Normochromic Hemolytic Anemias
- •Cytomorphological Anemias with Erythrocyte Anomalies
- •Bone Marrow Aplasia
- •Hyperchromic Anemias
- •Erythrocyte Inclusions
- •Hematological Diagnosis of Malaria
- •Thrombocyte Abnormalities
- •Thrombocytopenia
- •Lymph Node Cytology
- •Sarcoidosis and Tuberculosis
- •Non-Hodgkin Lymphoma
- •Metastases of Solid Tumors in Lymph Nodes or Subcutaneous Tissue
- •Branchial Cysts
- •Cytology of Pleural Effusions and Ascites
- •Cytology of Cerebrospinal Fluid
- •References
- •Index

58 Normal Cells of the Blood and Hematopoietic Organs
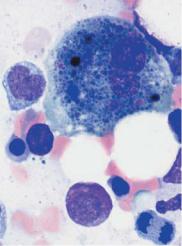
Bone Marrow: Medullary Stroma Cells
Fibroblastic reticular cells form a firm but elastic matrix in which the blood-forming cells reside, and are therefore rarely found in the bone marrow aspirate or cytological smear. When present, they are most likely to appear as dense cell groups with long fiber-forming cytoplasmic processes and small nuclei. Iron staining shows them up as a group of reticular cells which, like macrophages, have the potential to store iron. If they become the prominent cell population in the bone marrow, an aplastic or toxic medullary disorder must be considered.
Reticular histiocytes (not yet active in phagocytosis) are identical to phagocytic macrophages and are the main storage cells for tissuebound iron. Because of their small nuclei and easy-flowing cytoplasm, they are noticeable after panoptic staining only when they contain obvious entities such as lipids or pigments.
Osteoblasts are large cells with wide, eccentric nuclei. They differ from plasma cells in that the cytoplasm has no perinuclear lighter space (cell center) and stains a cloudy grayish-blue. As they are normally rare in bone marrow, increased presence of osteoblasts in the marrow may indicate metastasizing tumor cells (from another location).
Osteoclasts are multinucleated syncytia with wide layers of grayishblue stained cytoplasm, which often displays delicate azurophilic granulation. They are normally extremely rare in aspirates, and when they are found it is usually under the same conditions as osteoblasts. They are distinguished from megakaryocytes by their round and regular nuclei and by their lack of thrombocyte buds.
From the above, it will be seen that bone marrow findings can be assessed on the basis of a knowledge of the cells elements described above (p. 32ff.), taking account of the eight categories given on p. 52f. It also shows that a diagnosis from bone marrow aspirates can safely be made only in conjunction with clinical findings, blood chemistry, and the qualitative and quantitative blood values. For this reason, a table of diagnostic steps taking account of these categories is provided at the beginning of each of the following chapters.
Cells from the bone marrow stroma never occur in the blood stream
a 
 b
b
c 
 d
d
Fig. 20 Bone marrow stroma. a Spindle-shaped fibroblasts form the structural framework of the bone marrow (shown here: aplastic hematopoiesis after therapy for multiple myeloma). b A macrophage has phagocytosed residual nuclear material (here after chemotherapy for acute leukemia). c Bone marrow osteoblasts are rarely found in the cytological assessment. The features that distinguish osteoblasts from plasma cells are their more loosely structured nuclei and the cloudy, “busy” basophilic cytoplasm. d Osteoclasts are multinucleated giant cells with wide, spreading cytoplasm.
59

60
