
Practical Plastic Surgery
.pdf
622 |
Practical Plastic Surgery |
Part B: Radial Forearm Free Flap
AI
Peter Kim and John Y.S. Kim
Indications
The radial forearm free fasciocutaneous flap has become one of the mainstays of head and neck reconstruction. The radial forearm flap provides thin, pliable tissue from a reliable donor site based on a long vascular pedicle. It is described for coverage of soft tissue defects in the head and neck, the posterior trunk, and upper and lower extremities. Additionally, the radial forearm free flap has been used for reconstruction of defects of the esophagus and penis.
Numerous modifications have broadened the application of this flap. A portion of the radial cortex (no greater than one-third the circumference of the radius) can be harvested along with the skin paddle in reconstructing composite defects such as those seen in marginal mandibulectomies and palatal resections. The tendon of the palmaris longus can be included in the flap to be used as a sling in lip reconstruction. The lateral and/or medial antebrachial sensory nerve can be included to create a neurosensory flap, as is used in neophallus reconstruction.
Preoperative Considerations
Allen Test
This is the first screening test that should be performed on all potential patients. The surgeon uses his thumb and fingers to compress the radial and ulnar arteries at the wrist. The patient exsanguinates the hand by making a fist several times, and then opens the hand so that the fingers are in a relaxed and gently extended position. The examiner then releases pressure from over the ulnar artery. Capillary refill time in the hand is noted. A normal Allen test is refill in less than 5 seconds, and greater than 5 seconds indicates an abnormal Allen test. About 85-90% of patients will have a normal Allen test. If the test is normal, surgery can proceed without further testing.
If the Allen test is abnormal, bilateral duplex ultrasonography or pulse volume recordings should be performed of hands and fingers, with and without radial artery compression. Over 90% of these patients will have a normal noninvasive exam and can proceed to radial forearm flap harvest safely. In most cases, one of the two hands will demonstrate preserved flow pattern with radial artery compression, and consequently, safe harvesting of the flap. In the rare case that both hands demonstrate abnormal arterial flow to the hands, use of this flap is contraindicated.
The donor site scar must be addressed during preoperative counseling. The scar can be particularly unsightly in obese patients due to the high “step-off ” between the muscle bed and the surrounding skin. Other flaps may need to be considered if the patient is particularly concerned about the appearance of the donor site scar. Another relative contraindication is the use an osseocutaneous flap in postmenopausal women. Osteoporosis places these patients at increased risk of developing a postoperative fracture.
Appendix I |
623 |
AI
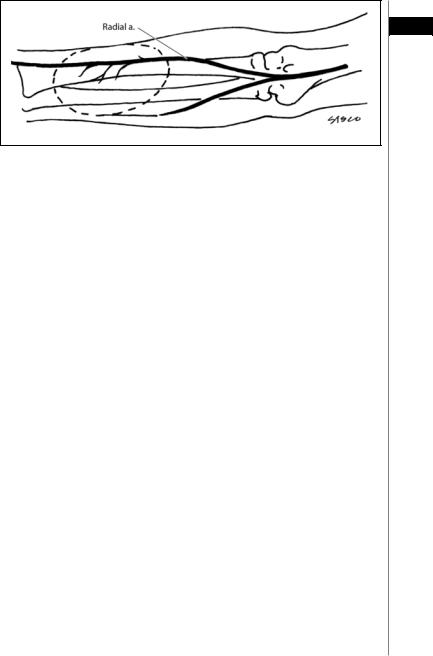
Figure AI.10. The course of the radial artery. The skin island can be designed anywhere along its axis (dashed area).
Flap Elevation
Harvest of the flap can usually be performed rapidly in a bloodless field using a tourniquet. The radial forearm flap is a Type II fasciocutaneous flap. Its dominant pedicle is the radial artery. Deep venous drainage is via the venae comitantes. Superficial venous drainage is through the cephalic vein which is routinely included with the flap. One large (up to 10 x 40 cm) or multiple smaller skin islands can be harvested anywhere in the volar forearm from the antecubital fossa to the wrist along the axis of the radial artery (Fig. AI.10).
As it bifurcates off the brachial artery, the radial artery courses between the brachioradialis and the pronator teres muscle bellies. As it progresses distally, it travels between the tendons of the brachioradialis and the flexor carpi radialis. Accordingly, the distal incision is made first, identifying the flexor carpi radialis and brachioradialis tendons, as well as the underlying artery. The cephalic vein lies radial to the brachioradialis tendon. It can be ligated and divided at this stage.
The proximal incision is made, and the brachioradialis and the flexor carpi radialis are identified. The radial artery can be found deep to the brachioradialis muscle and superficial to the pronator teres. An incision is carried out along the ulnar border of the skin island. The flap is then elevated from this ulnar border, working toward its arterial axis. The flap is elevated off the flexor digitorum superficialis, palmaris longus and the flexor carpi radialis. Particular care is taken to preserve the peritenon of the tendons. Just radial to the flexor carpi radialis lays the intermuscular septum carrying the fasciocutaneous perforators.
Lastly, the radial skin incision is made, and the deep fascia is dissected off the brachioradialis muscle ulnarward. The perforators are identified at the ulnar border of the brachioradialis along the intermuscular septum. The brachioradialis is retracted radially to reveal the radial artery. The radial artery is cross-clamped distally and, if adequate arterial filling of the hand is demonstrated, the radial artery is ligated and transected. The flap is elevated with dissection of the radial artery and its venae comitantes. The cephalic vein can be dissected further proximally to provide an additional long venous pedicle. The radial forearm flap is then ready for transfer to the intended defect.

624 |
Practical Plastic Surgery |
Postoperative Considerations
AI Donor Site Closure
Part of the donor site can be closed in a primary fashion. The remainder of the defect is covered with a split-thickness skin graft. The donor site is dressed according to preference and the hand is splinted for 5-7 days to ensure graft take.
Complications
Complications are not very frequent at the donor site, and harvest of this flap is generally well-tolerated. The following complications can occur:
•Infection
•Partial or complete skin graft loss
•Cold intolerance
•Hand claudication and other neurosensory changes
•Poor cosmetic appearance of the arm
•Radius fractures (osteocutaneous flap)
Pearls and Pitfalls
•Peritenon covering the flexor carpi radialis, brachioradialis, FDP and FDS tendons should be preserved to minimize skin graft loss and tendon desiccation.
•If the hand is found to be ischemic during cross-clamping of the radial artery, a venous interposition graft may rarely be needed to maintain adequate perfusion.
•Care should be taken to preserve the sensory branch of the radial nerve during dissection of the radial artery.
•It is important to include the intermuscular septum to preserve the septocutaneous perforators. The more distal the skin island, the longer the vascular pedicle.
Suggested Reading
1.Abu-Omar Y, Mussa S, Anastasiadis K et al. Duplex ultrasonography predicts safety of radial artery harvest in the presence of an abnormal Allen test. Ann Thorac Surg 2004; 77:116.
2.Bardsley AF, Soutar DS, Elliot D et al. Reducing morbidity in the radial forearm flap donor site. Plast Reconstr Surg 1990; 86(2):287.
3.Evans HB. The radial forearm flap. In: Buncke HJ, ed. Microsurgery: Tranplantation, Replantation: An Atlas Text. 4th ed. Philadelphia: Lea and Febiger, 1991: Chapter 14.
4.Evans GRD et al. The radial forearm free flap for head and neck reconstruction: A review. Am J Surg 1994; 168:446.
5.Villaret DB, Futran NA. The indications and outcomes in the use of osteocutaneous radial forearm free flap. Head Neck 2003; 25(6):475.
6.Yang G, Chen B, Gad Y. Forearm free skin flap transplantation. Nat Med J China 1981; 61:139.
626 |
|
|
Practical Plastic Surgery |
|
|
|
|
|
|
|
A |
B |
C |
|
AII
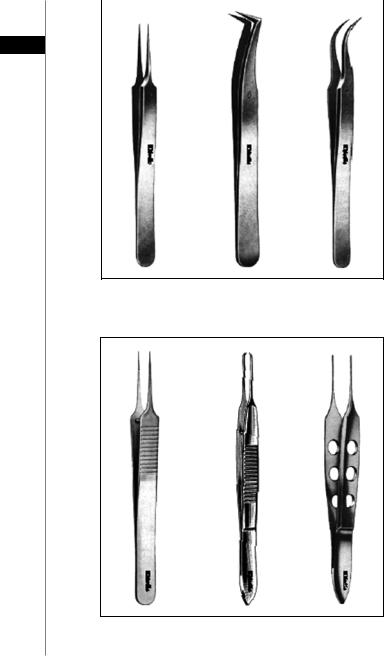
Figure AII.2. Jeweler forceps (straight, angled, curved).
A B C
Figure AII.3. Micro tying forceps (A), Castroviejo micro forceps (B), Bishop Harmon forceps (C).
Appendix II |
|
627 |
||
|
|
|
|
|
|
A |
B |
C |
|
AII
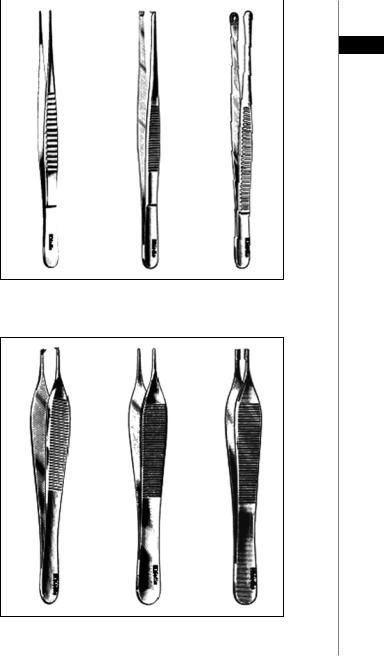
Figure AII.4. Debakey atraumatic forceps (A), Tissue forceps (B), Russian forceps (C).
A B C
Figure AII.5. Adson tissue forceps or “Adson with teeth” (A), Adson dressing forceps or “smooth Adson forceps” (B), Adson Brown forceps (C).
628 Practical Plastic Surgery
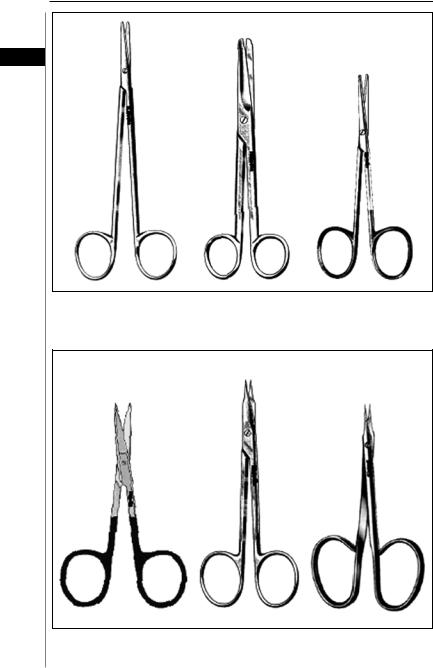
A B C
AII
Figure AII.6. Metzenbaum scissors (A), Mayo scissors (B), Strabismus scissors (C).
A B C
Figure AII.7. Iris scissors (A), Stevens tenotomy scissors (B), Gradle scissors (C).
Appendix II |
629 |
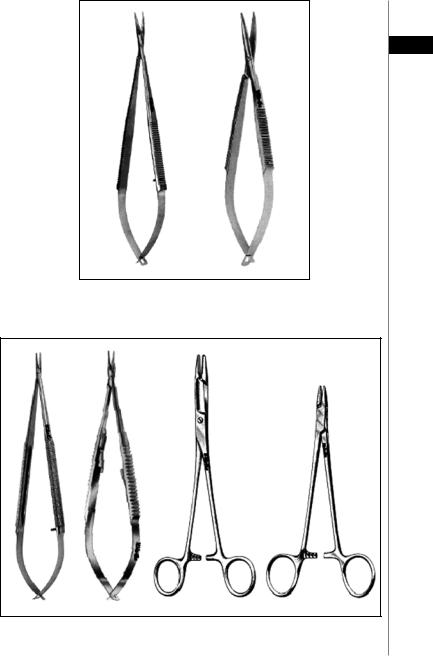
A B
AII
Figure AII.8. Micro scissors (A), tenotomy scissors (B).
A B C D
Figure AII.9. Barraquer needle holders (A), Castroviejo micro needle holder (B), Olsen-Hager needle holders (C), Webster/Brown needle holders (D).
630 |
|
|
|
Practical Plastic Surgery |
|
|
|
|
|
|
|
|
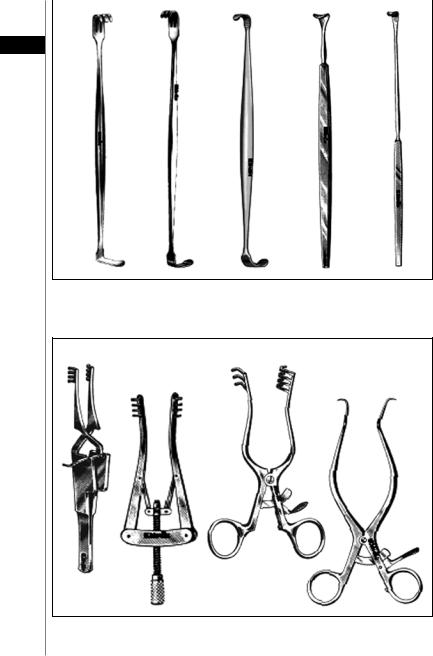
A |
B |
C |
D |
E |
AII
Figure AII.10. Mathieu retractor (A), Senn retractor (B), Ragnell-Linde retractor (C), Cushing vein retractor (D), Love nerve retractor (E).
A C
B D
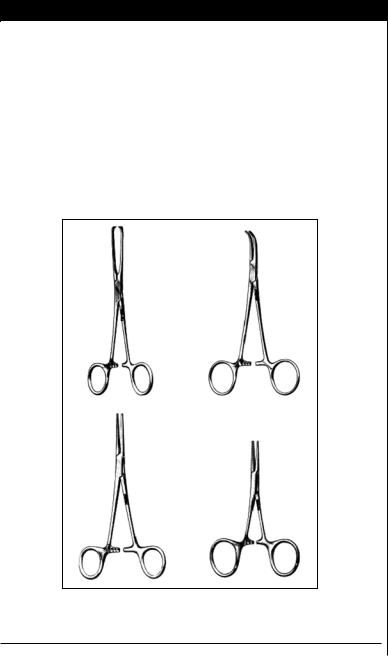
Figure AII.11. Self-retaining retractor (A), Alm retractor (B), Weitlaner retractor (C), Gelpi retractor (D).
Appendix II |
|
631 |
|
|
|
|
|
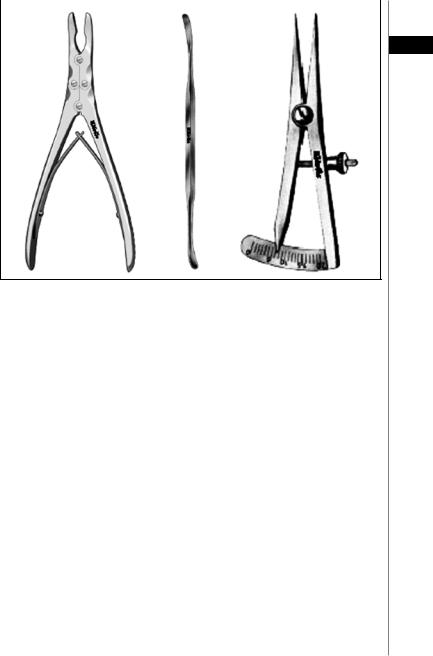
A |
B |
C |
|
AII
Figure AII.12. Ruskin/Beyer rongeur (A), Periosteal elevator (B), Castroviejo calipers (C).
