
Practical Plastic Surgery
.pdf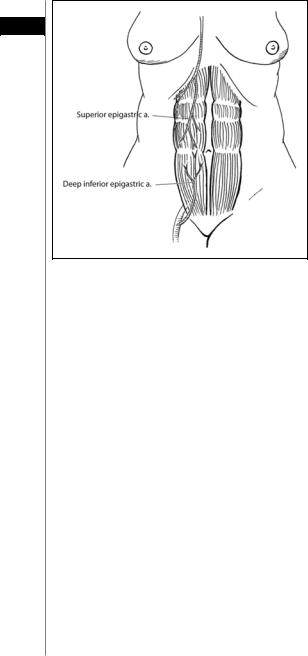
612 |
Practical Plastic Surgery |
Figure AI.2. The rectus abdominus musculocu- AI taneous flap and its dual
blood supply.
If only a muscle flap is required, the abdominal skin and subcutaneous fat are elevated off the anterior abdominal wall. The rectus sheath can then be opened as described above without concern for the musculocutaneous perforators.
Once the rectus muscle is harvested, the donor site is closed. The anterior rectus sheath can be closed primarily using a running or interrupted permanent suture. If the fascial edges are frayed or primary closure will create under undue tension, a synthetic mesh can be used to replace the missing segment. If necessary, small tears in the fascial edges during primary fascial closure can be reinforced with an overlying piece of mesh.
Fibula Composite Flap
The fibula free flap can be harvested as either an osseous or osseofasciocutaneous (composite), Type V flap. In addition, cuffs of muscle are usually incorporated in order to protect the blood supply. The dominant pedicle is the nutrient branch of the peroneal artery. The minor pedicles are the periosteal and muscular branches of the peroneal artery. The sensory nerve supply is from the superficial peroneal nerve. This flap is used primarily as a free flap for mandibular reconstruction or for reconstruction of the ipsilateral tibia and femur.
If an osseous flap is needed, a longitudinal incision is made along the posterior border of the fibula from the head of the fibula to the lateral malleolus. If an osseofasciocutaneous flap is used, the skin territory should be marked as a vertical ellipse over the middle third of the fibula. The skin island can span from 6 cm below the fibular head to 8 cm above the distal fibula, and it can measure up to 5 x 15 cm. The width of the skin island can be extended; however closure will require a skin graft.
For harvesting the osseous flap, the lateral compartment is opened, and the peroneus longus and brevis are detached from the fibula leaving a small cuff of muscle attached. The common and superficial peroneal nerves are identified and preserved.
Appendix I |
613 |
AI
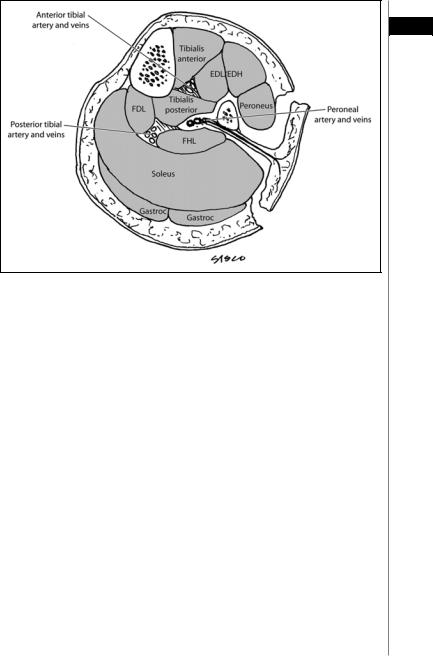
Figure AI.3. A cross section of the leg showing the compartments of the leg and the anterior and posterior approaches to the deep posterior compartment.
The proximal and distal osteotomies are performed (4 cm inferior to fibular head and 6 cm superior to lateral maleolus). As long as at least 6 cm of distal fibula is left intact, ankle stability will be preserved.
A cross section of the leg showing the compartments in relationship to the fibula are shown in Figure AI.3. In the anterior approach, the anterior compartment muscles are released followed by division of the interosseous membrane and entry into the superficial and deep posterior compartment musculature. The peroneal artery and vein are divided upon entry into the deep posterior compartment, followed by tibialis posterior and flexor hallucis longus. In the posterior approach, the posterior compartments are released first followed by entry into the anterior compartment and release of its musculature. Cuffs of muscle should be included with the flap.
The dominant pedicle usually enters the middle third of the fibula on the medial side via the nutrient foramen 14-19 cm (average of 17 cm) below the styloid process. The peroneal artery and vein can be dissected proximally as needed to achieve adequate length. Shortening of the bone should be done in the subperiosteal plane in order to avoid injuring the blood supply.
For harvesting the osseofasciocutaneous flap, the skin island is incised circumferentially down through the deep fascia. Anteriorly the skin island is elevated subfascially off the anterior and lateral compartment musculature. The posterior skin island is elevated subfascially off the lateral gastrocnemius and soleus muscles. The remainder of the dissection proceeds as described above. Special care is taken to preserve the septocutaneous and musculocutaneous perforators. A cuff of flexor hallucis longus and soleus should be preserved.
614 Practical Plastic Surgery
|
Pectoralis Major Flap |
|||
|
|
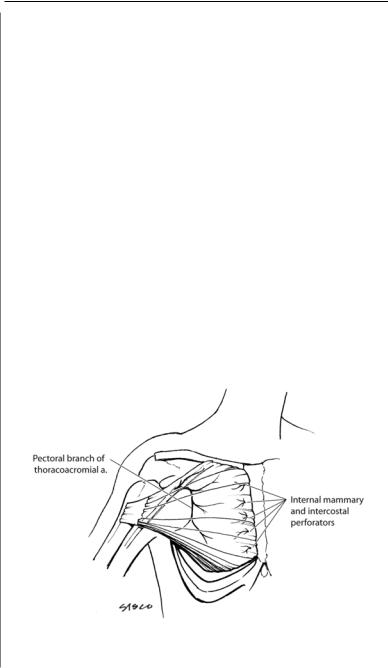
The pectoralis major flap (Fig. AI.4) can be harvested as either a muscle or |
||
AI |
||||
musculocutaneous, Type V flap. The dominant pedicle is the pectoral branch of |
||||
|
||||
|
the thoracoacromial artery. The minor pedicle is the pectoral branch of the lat- |
|||
|
eral thoracic artery. Minor segmental pedicles include the first through sixth inter- |
|||
|
nal mammary perforators, and the fifth through seventh intercostal perforators. |
|||
|
The muscle is innervated by the lateral (superior) and medial (inferior) pectoral |
|||
|
nerves. The sensory innervation is from the intercostal (2-7) nerves. It is a versatile |
|||
|
pedicle flap for coverage of defects of the face, chest, neck, shoulder, axilla, sternum |
|||
|
and upper extremity flap. It can also be used in the intrathoracic cavity. By dividing |
|||
|
either its origin or insertion, it can serve as a rotational flap or island pedicle flap |
|||
|
for many sites. The pectoralis major muscle flap can also serve as a functional flap |
|||
|
for the upper extremity (elbow flexion). Rarely, it is used as a free flap for coverage |
|||
|
in the head and neck or perineum. |
|||
|
|
The flap can be elevated with the entire skin paddle covering the muscle, or any |
||
|
part of it. The borders of the flap are the clavicle, the anterior axillary line, the sixth |
|||
|
intercostal space and the parasternal line. The skin territory can measure up to 20 x |
|||
|
28 cm. For head and neck reconstruction, a smaller skin paddle is used: an |
|||
|
inframammary skin island in women and a parasternal paddle in men. Most small |
|||
|
skin defects can be closed primarily. Larger skin paddles will leave a donor site re- |
|||
|
quiring skin grafting or secondary flap closure. |
|||
|
|
Harvesting the pectoralis major muscle is relatively simple. If only muscle is |
||
|
required, a horizontal incision is made below the clavicle, vertically along the axil- |
|||
|
lary line or midsternal. The skin and subcutaneous fat are dissected free of the muscle. |
|||
|
As an island flap based on the thoracoacromial pedicle, the muscle fibers are divided |
|||
|
from their origin and from the clavicle, and the muscle is dissected from medial to |
|||
|
|
|
|
|
|
|
|
|
|
Figure AI.4. The pectoralis major muscle flap and its blood supply.

Appendix I |
615 |
lateral. The muscle is divided just lateral to the pedicle, which enters the muscle from the deep side around the junction of the middle and lateral thirds of the clavicle.
As a turnover flap (reverse flap), the muscle is divided laterally at the level of the AI lateral border of pectoralis minor, preserving the lateral one-third of the muscle. The muscle is dissected from lateral to medial, preserving the vascular and nerve supply
to the remaining portion. The dissection continues to within 2-3 cm from the sternal border until the internal mammary perforators are visualized.
For head and neck reconstruction, the horizontal, infraclavicular skin incision is used. A skin paddle is often needed as described above. The skin island is incised and the muscle divided distally. Mobilization occurs in a superior direction towards the clavicle. If the entire muscle is not needed, a wide central strip of muscle is often sufficient to vascularize the skin pedicle. The musculocutaneous flap can be pulled through the clavicular incision.
If functional muscle transfer for the upper extremity is required, an anterior axillary line incision is used. The portion of muscle required is outlined. The muscle is dissected free from the subcutaneous tissue, and the origin at the ribs and sternum is divided. The muscle is mobilized from medial to lateral towards the humerus. Care is taken to preserve the blood supply and motor nerves. The muscle can be tunneled through the axilla onto the arm. Elbow flexion can be achieved by suturing the pectoralis to the biceps tendon.
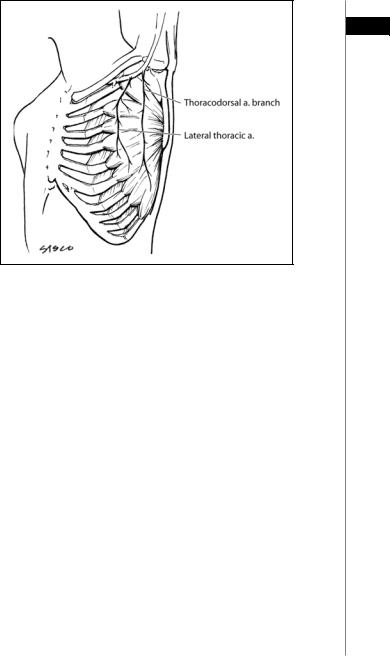
Latissimus Dorsi Flap
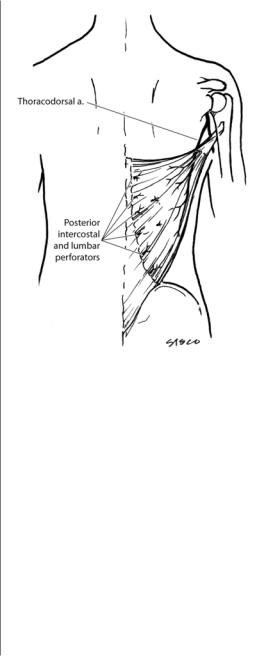
The latissimus dorsi flap (Fig. AI.5) can be harvested as either a muscle or musculocutaneous, Type V flap. The dominant pedicle is the thoracodorsal artery. Minor segmental pedicles include a medial and lateral row of posterior intercostals and lumbar perforators. The muscle is innervated by the thoracodorsal nerve which travels with the vascular pedicle. The sensory innervation is from the intercostal nerves. It is a versatile pedicle flap for coverage of defects of the neck, trunk, breast, abdomen and upper extremity. The latissimus muscle flap can also serve as a functional flap for the upper extremity (elbow extension or flexion). It is also used as a free flap for coverage in the scalp, lower and upper extremity-especially when a thin flap is required.
The skin island, when required, is marked. Options include oblique skin is- lands—with the superior end towards the midline or the axilla, superior posterior skin island, superior transverse, inferior transverse, lateral or vertical orientation. The dominant pedicle is marked in the posterior axilla entering the lateral deep surface of the muscle about 15 cm below the humeral insertion. The skin is incised around the island beveling away from the skin island. The muscle fibers of the latissimus are identified: superiorly, with the scapula and trapezius muscle. The fibers are divided, separating the muscle from the scapula. The attachments to the vertebral column are divided. The lumbrosacral fascia is divided to the level of the posterior axillary line. The minor pedicles are divided as they emerge from the posterior intercostals and lumbar vessels. The direction of dissection progresses towards the axilla where the pedicle is located. The dissection should allow sufficient flap mobility without compromising the pedicle. If needed, the insertion to the humerus can be divided to gain mobility.
If a muscle flap alone is required, the location of the skin incision is variable. Once the skin is incised and the superficial side of the muscle is exposed, the skin flaps are elevated off the muscle exposing its entire dimensions. The muscle is freed
616 |
Practical Plastic Surgery |
|||
|
|
|
|
Figure AI.5. The latissi- |
|
|
|
|
|
|
|
|
|
mus dorsi muscle flap |
AI |
|
|
|
|
|
|
|
and its blood supply. |
|
|
|
|
|
|
from its origin at the midline and superiorly as described above. Dissection proceeds towards the axilla and the pedicle. If the muscle is to be used as a free flap, adequate pedicle length can easily be achieved. Once the pedicle is clearly identified, the crossing branches to the serratus are divided. The circumflex scapular artery and branches to teres major are also divided. The insertion can be divided once the pedicle is completely dissected.
Serratus Flap
The serratus flap (Fig. AI.6) can be harvested as either a muscle or musculocutaneous, Type III flap. The dominant pedicles are the lateral thoracic artery and branches of the thoracodorsal artery. The muscle is innervated by the long thoracic nerve. The sensory innervation is from the intercostal (2-4) nerves. It is a versatile pedicle flap for coverage of defects of the head, thorax, axilla and posterior trunk. It can also be used in the intrathoracic cavity. By dividing either its origin or insertion, it can serve as a rotational flap or island pedicle flap. It is used as a free flap for coverage in the head and neck or limbs. It can also be used as a functional flap for facial reanimation. It can be harvested with the latissimus muscle as a combined flap. It can also be elevated as an osseomusculocutaneous flap by harvesting a portion of a rib along with the flap since the ribs are vascularized through the attachments of the serratus to the periosteum.
Appendix I |
617 |
AI
Figure AI.6. The serratus flap and its blood supply.
The serratus flap is often harvested without a skin paddle. The skin is incised diagonally across the axilla. The muscle slips are identified. The upper three slips are vascularized by the lateral thoracic artery. The remaining lower slips receive their blood supply from the thoracodorsal branches. Preservation of the upper slips will decrease the chances of scapular winging. Therefore, only the lower three or four slips should be harvested based on the branches from the thoracodorsal artery. The slips are divided from the ribs anteriorly and dissected posteriorly towards the scapula. The muscle is divided and elevated. The long thoracic nerve runs on the superficial surface of the muscle. This nerve should be preserved during the dissection. The thoracodorsal pedicle can be lengthened by dividing the branches to the latissimus.
If an osseomusculocutaneous flap is needed, the serratus is harvested with a portion of the 5th or 6th rib. The muscle slips to the desired rib are preserved, and the rib is dissected in the extrapleural plane.
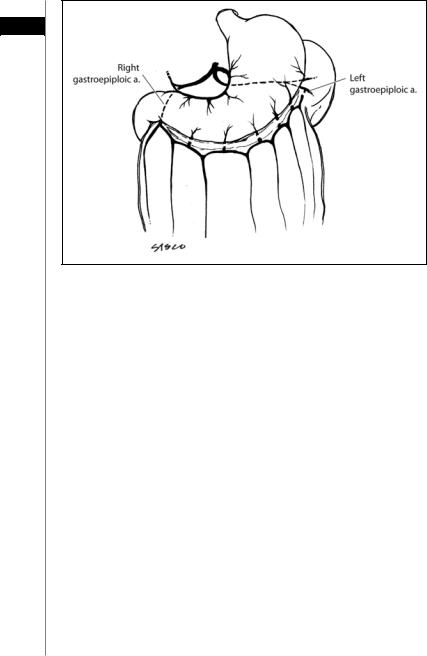
Omental Flap
The omental flap (Fig. AI.7) is a Type III visceral flap. It has two dominant pedicles: the right or left gastroepiploic arteries. It can be used as a pedicle flap for coverage in the head and neck, trunk, intrathoracic region, abdomen, groin and perineum. It is useful as a free flap for head and neck reconstruction or as coverage in the extremities.
The greater omentum lies between the greater curvature of the stomach and the transverse colon. After exposure of the peritoneal cavity, the omentum is released from its attachments to the colon along the antimesenteric border. The vascular branches from the gastroepiploic arch to the greater curvature are divided. The desired pedicle is chosen, and the other pedicle is ligated. When the right pedicle is chosen, the omentum is mobilized to within 3 cm of the pylorus. If it is to be harvested as a free
618 |
Practical Plastic Surgery |
AI
Figure AI.7. The omental flap and its blood supply.
flap, the gastroepiploic artery and vein can be dissected further for increased pedicle length. If the left pedicle is chosen, the right pedicle is divided and the omental dissection continues to within 7 cm of the gastrosplenic ligament.
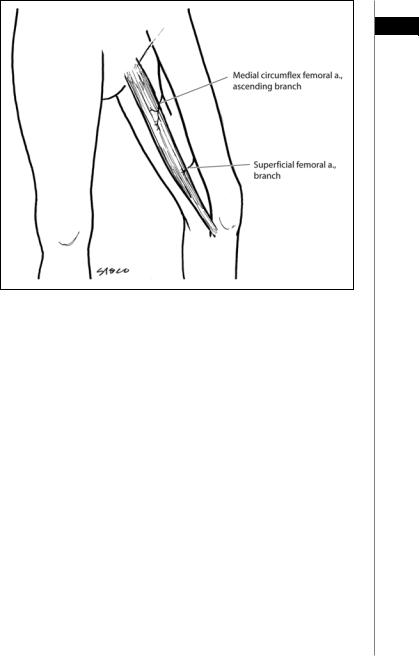
Gracilis Flap
The gracilis flap (Fig. AI.8) can be harvested as either a muscle or musculocutaneous, Type II flap. The dominant pedicle is the ascending branch of the medial circumflex femoral artery. The minor pedicles are the first and second branches of the superficial femoral artery. The muscle is innervated by the anterior branch of the obturator nerve which enters it on its deep surface, superior to the vascular pedicle. The sensory innervation is from the intercostal nerves. It is a versatile pedicle flap for coverage of defects of the abdomen, pelvis, perineum, groin, penis and vagina. The gracilis muscle flap can also serve as a functional flap for facial reanimation. It is also used as a free flap for coverage in the head and neck and extremities.
For muscle flap elevation, a linear incision is made 2-3 cm posterior to a line connecting the pubis and the medial condyle. The gracilis is posterior to the adductor longus. The musculotendinous insertion of the gracilis lies posterior to the sartorius and saphenous vein. The tendon is isolated with a penrose drain and then divided. As the muscle is mobilized proximally, the minor pedicles will be encountered as they enter the medial muscle belly. If the dominant pedicle is chosen, these minor pedicles are divided. The dominant pedicle can be exposed by medial retraction of the adductor longus. It passes over adductor magnus as it enters the gracilis on its deep surface about 10 cm inferior to the pubic tubercle. If additional pedicle length is required, as is the case for a free flap, the pedicle can be dissected proximally after
Appendix I |
619 |
AI
Figure AI.8. The gracilis muscle flap and its blood supply.
division of the branches to the adductor magnus and longus muscles. The anterior branch of the obturator nerve should be identified as it enters the muscle superior to the point of entry of the pedicle.
The skin island, if required, should be a vertical or horizontal ellipse overlying the proximal or mid portions of the muscle. Once the distal gracilis muscle is exposed, the relationship of the skin island to the underlying muscle should be confirmed prior to incising its entire border. If it has been drawn too distally, it should be redrawn in a more proximal position. The skin island should be incised from distal to proximal down to the level of the fascia. The deep surface of the skin island can be sutured to the muscle in order to avoid traction injury to the musculocutaneous perforators. The gracilis musculocutaneous flap does not have a robust and reliable skin paddle. Surgical delay should be considered if a large skin paddle is required.
Radial Forearm Flap
The radial forearm flap can be harvested as an osseofasciocutaneous or fasciocutaneous Type B flap. Its dominant pedicle is the radial artery and minor pedicles are musculocutaneous branches of the radial recurrent artery and the inferior cubital artery. The skin paddle can measure up to 10 x 40 cm, requiring skin grafting of the donor site in most cases. Primary donor site closure can be achieved if a very small skin paddle is used. This flap can be used locally in the arm, forearm or hand for coverage. It is a versatile free flap, often used in head and neck reconstruction.
The harvesting of this flap and the special considerations involved in its use are discussed in Part B of this appendix.
620 Practical Plastic Surgery
|
|
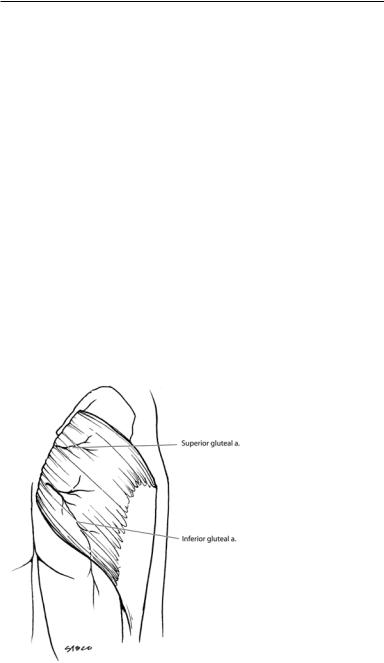
Gluteus Flap |
||
|
|
This flap can be harvested as a musculocutaneous, muscle or fasciocutaneous |
||
AI |
||||
|
flap (see below). It is a Type III flap with two dominant pedicles, the superior and |
|||
|
||||
|
|
inferior gluteal arteries (Fig. AI.9). Minor pedicles not commonly used as sole |
||
|
|
blood supply for the flap include the first perforator of the profunda femoral artery |
||
|
|
and branches of the lateral circumflex femoral artery. The skin paddle can measure |
||
|
|
up to 24x24 cm. This flap is used locally for coverage of pressure sores of the sacrum |
||
|
|
and ischium, as well as in the trochanteric region if other flaps (e.g., TFL flap) are |
||
|
|
not available. Bilateral flaps can be advanced medially to close a large midline sacral |
||
|
|
defect. It can also be used for reconstruction of pelvic and vaginal defects. |
||
|
|
The gluteal fasciocutaneous perforator flap is a Type A flap that can be used locally |
||
|
|
for coverage of spinal defects and pressure sores. It has also been uses successfully as a free |
||
|
|
flap, most notably for breast reconstruction. Most commonly the flap is based on the |
||
|
|
superior gluteal artery perforator, hence the common name for this flap is the SGAP. |
||
|
|
For fasciocutaneous flap harvest, the skin paddle is marked: either a transposition |
||
|
|
or V-Y advancement pattern is used, keeping in mind the ability to close the donor site |
||
|
|
directly. The skin is incised through the superficial fascia, down to the gluteal muscles. |
||
|
|
The flap is elevated along with the muscle fascia. Care is taken to locate the perfora- |
||
|
|
tors. The proximal perforators to be saved are skeletonized to allow greater flap mobil- |
||
|
|
ity. Those that hinder flap mobility are ligated and divided. When used locally, the flap |
||
|
|
is transposed or advanced into the defect and sewn into place with two layers. For the |
||
|
|
free SGAP, the perforators are traced back to the superior gluteal artery, and the pedicle |
||
|
|
is dissected proximally to gain sufficient length. |
||
|
|
For musculocutaneous flap harvest, either a superior or inferior skin paddle can be |
||
|
|
utilized. The superior skin paddle is based on the superior gluteal artery, and the infe- |
||
|
|
rior paddles on the inferior gluteal artery (The entire muscle and buttock skin can be |
||
|
|
|
Figure AI.9. The gluteus |
|
|
|
|
||
|
|
|
muscle flap and its blood |
|
|
|
|
supply. |
|
|
|
|
|
|

Appendix I |
621 |
based on the inferior artery). The muscle flap can be advanced or rotated. The skin and subcutaneous tissue are divided. For rotational flaps, the muscle insertion (greater
trochanter and IT band) is also divided. The inferior and lateral borders of the muscle AI are divided. The muscle is detached from its origin. For ambulatory patients, the infe-
rior portion of the muscle with its insertion and origin should be preserved. The pedicle and the sciatic nerve are located using the piriformis muscle as a landmark (the sciatic nerve emerges from beneath this muscle). The flap is inset into the defect, and the muscle fascia is sewn to the contralateral gluteus maximus fascia. The subcutaneous tissue is closed in a second layer followed by skin. The donor site is closed directly over a suction drain, and additional drains placed under and over the flap. If direct closure is not possible, skin grafting the donor site is an option.
Anterolateral Thigh (ALT) Flap
The ALT flap is a Type B or C fasciocutaneous flap is an extremely versatile free flap used most commonly for head and neck reconstruction. It can also be raised as a purely cutaneous free flap without the underlying fascia. It is based on either septocutaneous or musculocutaneous branches (much more common) of the descending branch of the lateral circumflex artery. A skin paddle up to 12 x 20 cm in size can be harvested; however any flap wider than 10 cm is difficult to close primarily.
The skin island is marked by drawing a line down the lateral thigh: from the ASIS to the superolateral corner of the patella. The midpoint of this line represents the site at which the greatest concentration of perforators can be found. A 6 cm diameter circle (centered at the midpoint of the line) will capture the main perforators and should be included within the flap. The medial border incision is made first. The dissection can be either subfascial or suprafascial. The subfascial dissection is safer and will create a fasciocutaneous flap; however the underlying muscles will bulge out and make the closure more difficult. In addition, there is greater risk of injury to the sensory and motor nerves that travel within and just below the fascia. The suprafascial dissection will yield a purely cutaneous ALT flap, sparing the nerves and muscular fascia. This dissection is challenging due to the smaller size of the perforators above the fascia. The perforators are traced back to the lateral circumflex artery pedicle. In only about 10-15 % of cases is there an adequate septocutaneous vessel. In the majority of cases, the perforators are musculocutaneous and must be followed to the pedicle through the vastus lateralis and rectus femoris muscles.
Once sufficient pedicle length has been obtained, the lateral skin incision can be made. The advantage of not incising the entire skin border early on is most notable in head and neck reconstruction. The harvest of the flap can be performed simultaneously with the resection and recipient site preparation. Prior to making the final skin incision, the size of the required skin island will be known based on the size of the defect and any size adjustments can be made. After the lateral aspect of the flap is raised and joined with the medial dissection, the pedicle is ligated and the flap transferred. A skin island less than 10 cm in width can usually be closed primarily over suction drainage. If this is not possible, the majority of the donor site is closed, and a skin graft is used to cover the remaining central portion.
Suggested Reading
1.Mathes SJ, Nahai F. Reconstructive Surgery: Principles, Anatomy, and Technique. New York: Churchill Livingstone, 1997.
2.Strausch B, Vasconez LO, Findley-Hall EJ. Grabb’s Encyclopedia of Flaps, 2nd edition. Boston: Little Brown, 1998.
