
Practical Plastic Surgery
.pdf
Common Anomalies of the Hand and Digits |
593 |
|
|
|
|
Table 99.2. Preaxial (thumb) duplications are classified from distal to proximal
Classification |
Site of Duplication |
Type I |
Distal phalanx |
Type II |
Interphalangeal joint (common) |
Type III |
Proximal phalanx |
Type IV |
Metacarpophalangeal joint (common) |
Type V |
First metacarpal |
Type VI |
Carpometacarpal joint |
|
|
index space with a Z-plasty. In addition, of the thumb’s three mobile joints, at least two should be preserved. Long-term outcomes are usually less than optimal, especially in the more proximal duplications. Strength, mobility and function are almost never as good as in the unaffected side.
Syndactyly |
|
|
Preoperative Considerations |
|
|
Syndactyly, or webbing of the digits, is classified based on the extent of webbing |
|
|
and the nature of the interconnected tissue (Table 99.3). |
|
|
Intraopertive Considerations |
|
|
Simple, incomplete syndactyly can often be treated with skin flaps only, sparing |
|
|
the need for skin grafts. Correction of syndactylized digits is usually performed as a |
|
|
staged procedure since simultaneous release of both the radial and ulnar side can |
|
|
compromise vascular supply to the digit. This is a procedure that relies on meticu- |
|
|
lous, atraumatic technique. Zigzag incisions should be used on the palmar surface, |
|
|
and the flaps should be divided equally between the two digits. The volar flap base |
|
|
should be kept wider than the base of the dorsal flap. Full-thickness skin grafts are |
|
|
commonly required, especially for commissure reconstruction. The digits are closed |
|
|
from distal to proximal, preferably using absorbable sutures in young children. In |
|
|
cases of complex syndactyly the bone should be covered with soft tissue and burred |
|
|
down until it is smooth. |
|
|
Postoperative Considerations |
|
|
The web spaces must be packed with gauze dressings so that there is no |
|
|
undesirable healing of raw surfaces to one another. In some centers, dressing |
|
|
Table 99.3. Classification of syndactyly |
99 |
|
Classification |
Description |
|
Simple, complete |
Soft tissue connection only, webbing extends to fingertips |
|
Simple, incomplete |
Soft tissue connection only, webbing terminates |
|
|
more proximally |
|
Complex |
Either bony or cartilaginous connections |
|
Complicated |
Duplicated skeletal parts located in the interdigit space |
|
594 |
Practical Plastic Surgery |
changes are performed under general anesthesia. Postoperative immobilization is essential. Inadequate protection of the surgical site can lead to infection, skin graft loss and dehiscence. Many surgeons will cast the child’s entire arm with the elbow flexed at 90˚. Straight arm or shorter casts are no match for the active, determined child.
Insufficient commissure release or closure under tension at the time of the original surgery can lead to scar contracture at the web space or “recurrence” of the webbing. This complication will often require surgical revision, especially for the first web space, which is undoubtedly the most important one. Additional full-thickness skin grafts or recruitment of local soft tissue is required for release of the web space. Overall, the revision rate for syndactyly repair is about 10%.
Radial Clubhand
Preoperative Considerations
The incidence of this anomaly is 1 in 50,000 births. In can occur as an isolated congenital defect, or as part of a syndromic condition such as VATER syndrome (vertebral, anorectal, tracheoesophageal, renal, and radial anomalies). Radial club hand ranges from mild radial hypoplasia to complete aplasia of the radius (Table 99.4). Syndromic cases are more severe. In most cases, the ulna is subsequently deformed, demonstrating bowing and thickening. The wrist is usually deviated to the radial side, and the muscles of the forearm and wrist are often fused and shortened. The thumb is often hypoplastic or absent. Elbow flexion is minimal but improves with time.
Treatment
Treatment begins with limb stretching by the parents. Nighttime splinting can help maintain the limb in the stretched position. Skeletal traction using an external fixating device is also an option. Once the wrist is in a neutral position, it is stabilized and centralized. The treatment should begin around the age of 6 months. This process greatly relies on the use of tendon transfers. Once the wrist is centralized, K-wire fixation maintains its position for at least three months. If the radial muscles are inadequate for tendon transfers, wrist arthrodesis can be considered. Syndromic radial club hands have a much poorer outcome, since the deformity is usually more severe. Once wrist alignment is achieved, pollicization is performed in a subsequent procedure.
|
|
Table 99.4. Classification of radial clubhand |
|
|
|
|
|
|
|
Classification |
Description |
99 |
|
Type I |
Proximal or distal radial deficiency, very little deviation |
|
|
|
or bowing |
|
|
Type II |
Shortened radius, deviated hand, bowed and thickened ulna |
|
|
Type III |
Partial radius, hand is deviated and ulna is bowed |
|
|
|
(most common) |
|
|
Type IV |
Complete radius aplasia, sublaxed and deviated hand, |
|
|
|
bowed ulna |

Common Anomalies of the Hand and Digits |
595 |
Symphalangism
Defined as fused phalanges at the interphalangeal joints, this condition is seen in syndromic patients such as those with Apert syndrome or Poland syndrome. Both syndromes involve fusion of phalanges primarily in the central three rays. The metacarpophalangeal joints are spared. In addition to syndromic cases, true symphalangism has a genetic basis and presents with PIP involvement, fused digits and long, slender fingers.
Treatment of symphalangism should focus on correcting digital angulation and rotation rather than finger stiffness. PIP joint fusion should be done at 10˚, 30˚, 40˚ and 50˚ for the index, middle, ring and small finger, respectively. The IP joint can be reconstructed using a number of techniques, ranging from silicone caps and spacers to vascularized second-toe joint transfer. Most techniques provide less than optimal results. When possible, autogenous material is preferred in children.
Camptodactyly
Defined as a flexion deformity of the digit or thumb, this condition often involves the PIP joint of the fifth finger. It develops as a result of an imbalance between the forces of flexion and extension at the involved joint. Abnormal insertions of the lumbricals or interossei can result in excessive flexion forces and consequent flexion deformity of the joint. Involved digits will be stiff and have decreased range of motion. On radiographic evaluation, the phalanx will have a flat condyle (instead of the normal rounded shape) and flat articulating surface.
Contractures of less than 50˚ have good outcomes with conservative treatment alone. Stretching and splinting are usually adequate. Contractures greater than 70˚ usually indicate a long-standing deformity, and joint fusion is required. Any surgical release of a contracture must be followed by intensive ranging exercises and splinting at night.
Constriction Ring Syndrome
Other terms used to describe this condition include annular band syndrome, amniotic bands, and congenital amputations. There is no positive inheritance pattern in CRS. It occurs sporadically in utero. The mechanism is believed to be the detachment of strands of the chorionic sac that wrap around a body part of the fetus. Examples include fingers, toes and even entire limbs. The anatomy proximal to the point of constriction is entirely normal. Distal, however, the tissue is deprived of oxygen and develops abnormally. The constricted site has a characteristic ring appearance. This band can be superficial or extend down to the periosteum. It can completely encircle the digit, or only partially span its circumference.
Treatment of CRS consists of excising the scarred, constricting ring, and filling the resulting contour deformity with advancement or rotational flaps. Z-plasties
alone will not correct the problem. Toe-to-thumb transfer works well in these pa- 99 tients, since the anatomy proximal to the constriction site is normal and the tendons, nerves and blood vessels are adequate for reconstruction.
Trigger Thumb
This condition is essentially a stenosing tenosynovitis of the flexor tendon sheath. Many cases are bilateral. The differential diagnosis includes congenital absence of the extensor pollicus longus which results in unopposed flexion forces on the thumb.

596 |
Practical Plastic Surgery |
The children present at a young age with thumbs that lock and trigger upon extension. As the volar plate is stretched, a compensatory hyperextension of the MP joint will occur. A-1 pulley release should be performed by age 2. Prior to that, there is still a possibility of spontaneous resolution of the problem. The treatment of trigger fingers is discussed in greater detail elsewhere in this book.
Pearls and Pitfalls
•Release of the first web space and creation of a mobile, opposable thumb is perhaps the most functional operation a pediatric hand surgeon can perform for syndactyly.
•Adequate release of the first web space can be achieved with a Z-plasty. Although a single large Z-plasty may seem adequate, it is often better to use the four-flap Z-plasty for optimal length and contour within the depth of the web space.
•When releasing syndactylized digits, the skin flaps should be equally distributed between the two digits. It is risky to allot all of the flap tissue to one digit and skin graft the other.
•In thumb polydactyly, the ulnar thumb is usually better. If both thumbs are similar in size, appearance, and function, the one with the better ulnar collateral ligament at the MP joint should be preserved. Occasionally, a new thumb must be created using the best parts from each partner.
•In distal phalanx duplications, the nail should be narrowed and the paronychial fold recreated. In proximal phalanx duplications, the collateral ligaments must be recreated but not using the extensor mechanism. Adequate gliding of an extensor tendon requires a smooth layer beneath it.
•The optimal age for correction of constriction bands and separation of digits is controversial. Many surgeons advocate operating on the child towards the end of the first year of life. Hand and foot procedures should be done before the child begins to explore the environment with his hands and to walk.
Suggested Reading
1.Brown PM. Syndactyly—a review and long term results. Hand 1977; 9(1):16-27.
2.Cohen MS. Thumb duplication. Hand Clin 1998; 14(1):17-27.
3.Graham TJ, Ress AM. Finger polydactyly. Hand Clin 1998; 14(1):49-64.
4.Miura T. Congenital constriction band syndrome. J Hand Surg [Am] 1984; 9A(1):82-8.
5.Steenwerckx A, De Smet L, Fabry G. Congenital trigger digit. J Hand Surg [Am] 1996; 21(5):909-11.
6.Upton J. Congenital anomalies of the hand and forearm. In: McCarthy JG, May J, Littler JW, eds. Plastic Surgery. Vol 8. Philadelphia: W.B. Saunders, 1990.
7.Van Heest AE. Congenital disorders of the hand and upper extremity. Pediatr Clin North Am 1996; 43(5):1113-33.
99

598 |
Practical Plastic Surgery |
3.Hueston posits an “extrinsic theory” that claims that Dupuytren’s disease occurs via nodules that are generated by de novo metaplastic transformation of fibrofatty tissue which will then become cords.
4.Gosset distinguishes cords from nodules. He believes that nodules arise de novo and that cords arise from palmar fascia. Therefore, nodules and cords represent different forms rather than different stages of Dupuytren’s disease (synthesis theory).
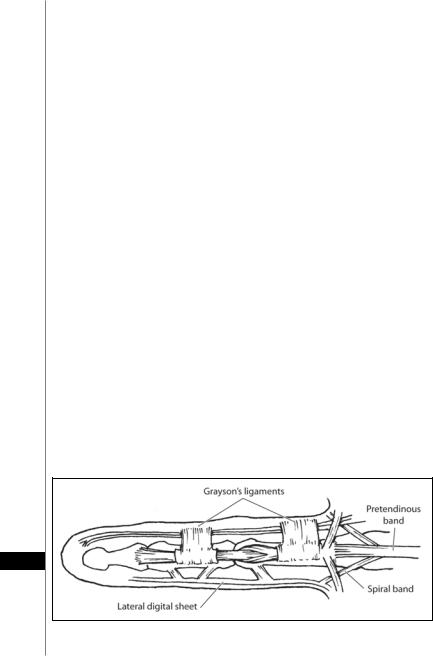
Relevant Anatomy
During the development of Dupuytren’s disease, fascia and ligaments become thickened cords, resulting in MCP, PIP and sometimes DIP joint contractures in the digits. Nodules and cords will form in the palm. MCP joint contracture occurs when the pretendinous bands—the longitudinal extension of the palmar aponeuro- sis—become fibroblastic. PIP joint contracture is common in Dupuytren’s disease and related to the formation of cords: the central cord and the spiral cord. These develop out of four anatomical structures: the pretendinous band, the spiral band, the lateral digital sheet and Grayson’s ligament (Fig. 100.1). With advanced disease, the neurovascular bundle will be displaced superficially and toward the palmar midline. Less common, PIP joint contracture can originate from a single lateral cord derived from the lateral digital sheet; however, this attenuated form does not usually lead to a midline shift of the neurovascular bundle. Natatory ligaments may also be involved, leading to an adduction deformity at the webspaces.
Clinical Presentation
The typical patient with early Dupuytren’s disease is a middle-aged, male Caucasian of northern heritage presenting with palmar nodules (most often at the base of the ulnar digits). The palmar skin becomes more and more atrophic and adherent to the nodules. In later stages MP and PIP flexion contractures, or compensatory DIP joint hyperextensions can be observed due to progressive cord formation proximal to the nodules. Sometimes in more aggressive forms of Dupuytren’s disease, knuckle pad formation on the dorsum of the PIP joint can also be observed.
Nonsurgical Treatment
Many nonsurgical therapies have been evaluated over the last decades, including vitamin E, DMSO, allopurinol, colchicines, α-interferon and calcium-channel
100
Figure 100.1. The primary structures that become pathologic cords in Dupuytren’s disease. (Note that Cleland’s ligament is not involved.)

Dupuytren’s Disease |
599 |
blockers. These treatments have not demonstrated long-term reliability. Inconsistent data exists concerning treatment with ultrasonic therapy and corticosteroid injections. Static or dynamic splinting, either preor postoperatively, is the oldest technique in the treatment of Dupuytren’s but is generally used as an adjunctive modality and not as the principal method of treatment.
The most promising nonsurgical approach under investigation is the ultrasonographic guided percutaneous fasciotomy with collagenase, an enzyme deriving from Clostridium histolyticum. In a recent study, direct injection of collagenase in the contracted cord in select clinical situations showed excellent results in 90% of involved MP joints and 66% of PIP joints. Further studies are needed to confirm the efficiacy and safety of this novel treatment and refine inclusion criteria.
Surgical Treatment
Indications
In and of itself, the existence of the disease does not mean surgery is required. The decision for surgery should be based on the degree of contracture, the extent of involved joints, and the patient’s age and specific situation. It should also be noted that while surgery is the mainstay of treatment for advanced disease, recurrence rates range from 26-80%.
Widely accepted indications for surgery are:
a.Flexion contracture of the MP joint greater than 30˚
b.Flexion contracture of the PIP joint of any degree
c.Concomitant web space contracture, impaired neurovascular status and loss of
articular cartilage Contraindications include:
a.Infected or macerated skin, especially when skin grafts will be required
b.Noncompliant patients
c.Advanced concomitant arthritis
Surgical Principles and Strategies
Surgical treatment varies from simple fasciotomy to regional fasciectomy or subtotal removal of the fascia. Generally, fasciectomy is advocated. On rare occasions, dermatofasciectomy may be required for advanced, recalcitrant cases with extensive involvement of the overlying skin. Incisions are either performed in a longitudinal or transverse fashion in the palm. Oblique Bruner’s incisions can be used for digital incisions. Alternatively, a series of short transverse skin incisions in the palm and phalanges can limit the number and length of scars. This later technique can be particularly useful when the palm and multiple fingers are involved. Less common now is the McCash technique in which an open palm incision is made, and the transverse incision heals secondarily or is covered by a full-thickness skin graft.
For severe contractures in the digits, extreme care must be taken with even the 100 skin incision since the contracture has displaced the neurovascular structures super-
ficially so that the nerve and vessels may literally be up against the dermis. Since the tourniquet is inflated, the vessels may be barely visible. For such severe contractures, it is useful to identify both ulnar and radial neurovascular bundles proximally in the palm and trace them distally into the cord. Separating the scarred structures from the vital digital nerve and vessels will be necessarily tedious. Additionally loss of domain can occur with severe contractures, and it may be necessary to perform

600 |
Practical Plastic Surgery |
grafts or rarely flaps to cover the exposed structures in the digit. Loss of domain in the palm can be allowed to heal secondarily via the McCash technique.
Complications
Early Complications
Early complications include infection, hematoma, skin loss and nerve or vascular injury. Risk of hematoma can be reduced if meticulous cauterization of small bleedings is performed after tourniquet release. The most dreaded complication is irreversible neurovascular injury. The tourniquet should be released to ensure appropriate digital perfusion after contracture release. If ischemia persists, then revascularization procedures with vein grafts may be necessary.
Late Complications
Late complications include recurrence, reflex sympathetic dystrophy (RSD) and loss of flexion. Young patients with a family history are the most prone to recurrence. Recurrence should be differentiated between local recurrence of Dupuytren’s tissue at the former site of resection or as distant recurrence elsewhere in the hand resulting in flexion or extension deformity. Surgical treatment of Dupuytren’s disease poses an increased incidence for development of RSD, with a 3-5 times higher incidence in female patients. Ensuring that the patient is compliant with the postsurgical rehabilitation decreases the risk of subsequent RSD. Overall, 10-20% of all Dupuytren’s patients who undergo surgery experience one or more complication.
Postsurgical Therapy
Postoperative physical therapy with both active and passive range of motion is mandatory. Static splinting may also be instituted to ameliorate persistent contracture.
Pearls and Pitfalls
The use of limited transverse incisions across the palm and digits is an effective way to perform fasciectomies without extensive scarring. Incisions should be placed within preexisting creases and in the case of adjacent digits may be extended in the palm. The putative advantage of limiting incisions is that postoperative rehabilitation is facilitated. If there are sites of severe contracture, delicate extension should be performed after their release. Gentle manipulation and rewarming over time should return perfusion to the digit. Only rarely will persistent ischemia occur. In such cases, the patient should be kept in the recovery area until the surgeon has determined whether revascularization is necessary.
Suggested Reading
1.Saar JD, Grothaus PC. Dupuytren’s disease: An overview. Plast Reconstr Surg 2000; 106:125.
2.McFarlane RM, Jamieson WG. Dupuytren’s contracture: The management of one
100hundred patients. J Bone Joint Surg [Am] 1966; 48:1095.
3.Hueston JT. Dupuytren’s contracture. Lancet 1986; 22(2):1226
4.Lubahn JD. Dupuytren’s disease. In: Trumble TE, ed. Hand Surgery Update 3. Hand, Elbow and Shoulder. Illinois: American Society for Surgery of the Hand, 2003:393-401.

