Practical Plastic Surgery
.pdf
552 |
Practical Plastic Surgery |
sterile matrix, and the roof of the nail fold. The germinal matrix, which produces over 90% of nail volume, extends from the proximal nail fold to the distal end of the lunula. The lunula represents the transition zone of the proximal germinal matrix and distal sterile matrix of the nail bed. The sterile matrix (ventral nail) contributes additional substance largely responsible for nail adherence. The roof of the nail fold (dorsal nail), which includes the germinal matrix, is responsible for the smooth, shiny surface of the nail plate. The hyponychium is the area immediately below the fingernail at its cut edge which serves as a barrier to subungual infection and also marks the terminal extension of bone support for the nail bed. The eponychium is the skin covering the dorsal roof of the nail fold. The paronychium is the skin at the nail margin, folded over its medial and lateral edges.
Classification
Van Beek et al have further classified acute fingernail and nail bed injuries as outlined below. This classification system provides a framework for determining the appropriate treatment.
I.Germinal Matrix Injury
•GI: Small subungual hematoma in proximal nail (25%)
•GII: Germinal matrix laceration, large subungual hematoma (50%)
•GIII: Germinal matrix laceration and fracture
•GIV: Germinal matrix fragmentation
•GV: Germinal matrix avulsion
II.Sterile Matrix Injury
•SI: Small nail hematoma (25%)
•SII: Sterile matrix laceration, large subungual hematoma (50%)
•SIII: Sterile matrix laceration with tuft fracture
•SIV: Sterile matrix fragmentation
•SV: Sterile matrix avulsion
|
Treatment |
91 |
It is important that the nail bed be repaired with great attention to detail in order |
|
to restore its function and prevent any uncomfortable or unsightly deformities. Loupe |
|
magnification is recommended, and the use of microsurgical instruments allows |
|
easier handling of the tissue and small needle. |
|
Grade I Injuries |
|
Grade I injuries are treated nonoperatively unless they are painful, for which de- |
|
compression or nail removal can be performed. Decompression of a subungual he- |
|
matoma should be performed to relieve pain if it involves no more than 50% of the |
|
area of the nail. A hole should be placed in the nail plate over the hematoma with |
|
either a heated paper clip or an 18-gauge needle twirled like a drill. For larger subun- |
|
gual hematomas, the nail plate should be removed in order to repair the nail bed. |
|
Grade II, III, and IV Injuries |
|
The first step in treating grade II, III, and IV injuries is to carefully remove the nail |
|
by separating the nail plate from the nail matrix with a Freer elevator. Care must be |
|
taken during this step to avoid injury to the underlying nail bed. An adherent nail may |
|
indicate a grade I injury with limited nail bed involvement. The wound is then irri- |
|
gated and debrided, limiting debridement to contaminated or devitalized tissues. The |
|
nail bed is then repaired under loupe magnification using 5-0 or 6-0 chromic suture. |

Injuries of the Finger |
553 |
If the proximal germinal matrix is injured, visualization may be obscured by the nail fold. Make skin incisions at 90˚ to the nail fold along the lateral border of the nail, then elevate the nail fold to fully evaluate the extent of the injury. If an associated phalangeal fracture is unstable, it may displace the nail bed. Unstable fractures should be pinned with a Kirschner wire, avoiding the distal interphalangeal joint if possible.
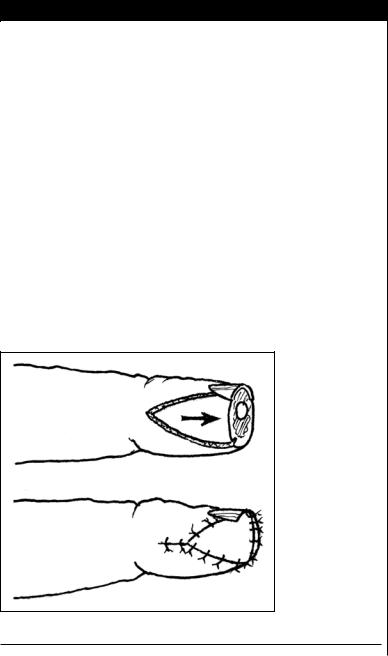
After any repair, the nail plate should be placed back into the nail fold. Replacement of the nail has several important functions: (1) it serves as a template for the new growing nail, (2) it serves as a splint for fractures, (3) it provides a biologic dressing for the nail bed, and (4) it prevents scarring of the nail fold to the nail bed. Using 4-0 or 5-0 nylon sutures, the nail is secured in place with two horizontal mattress sutures placed proximally on both sides of the nail. One or two simple sutures may be placed in the distal aspect of the nail and pulp to further secure the nail. If the nail plate is fragmented or not available, an artificial nail, a Silastic sheet, or a nail-shaped piece of nonadherent gauze is a good substitute. These can be left in place indefinitely, as they will be pushed out as the new nail regrows. Finally, the finger is bandaged to protect the digit and motion is restricted for 7 to 10 days.
Nail-Matrix Avulsions
When the proximal portion of the nail plate has been avulsed from the nail fold and lies on top of it, there is always an associated nail-bed laceration or avulsion of the germinal matrix from its proximal attachment and a fracture or epiphyseal separation. Proximal detachments or avulsions of the germinal matrix must be replaced into the nail fold. Three sutures, one at each corner and one in the middle, are sufficient. Each suture is passed from the outside to the inside of the nail fold, through the proximal edge of the germinal matrix in a horizontal-mattress fashion, and back through the base of the nail fold, exiting dorsally. After all the sutures have been passed, the germinal matrix is cinched into place by pulling proximally on the sutures, which are tied over the dorsum of the nail fold.
If the nail bed injury is associated with a loss of matrix tissue, the detached nail plate should be inspected for remnants of the nail bed that can be used for repair. If
available the avulsed tissue can be carefully removed from the nail plate with a scal- 91 pel and sutured in place as a full-thickness graft directly on the distal phalanx. De-
fects in the sterile matrix with no tissue available for repair should be treated with a split-thickness nail bed graft. Split-thickness sterile matrix grafts are obtained by shaving the donor nail bed with a scalpel blade. The graft must be very thin (about one hundredth of an inch) to prevent a deformity from occurring at the donor site. The graft is then sutured to the surrounding nail bed. Treatment of germinal matrix avulsion with no available tissue for replacement depends primarily on the size and width of the defect. Splitor full-thickness germinal matrix grafts and local bipedicle or distally based nail bed flaps have been employed. If the entire nail bed has been completely or nearly completely avulsed and the distal phalanx remains, the best treatment is the application of a split-thickness skin graft.
Complications
Complications from nail bed repair are usually mild. Various nail deformities can occur at the injury or donor sites. Rarely, permanent loss of the fingernail can occur.
Phalangeal Injuries
Fractures of the phalanges are the most common fractures of the skeletal system, accounting for 10% of all fractures in several large series. The distal phalanx is the

554 |
Practical Plastic Surgery |
most commonly fractured bone of the finger. The middle phalanx is the least commonly fractured because of its high proportion of cortical to cancellous bone. Phalanges of the central digits are longer and sustain more fractures than the border digits.
Anatomy and Terminology
Each finger, except the thumb, has three phalanges: the proximal phalanx, the middle phalanx, and the distal phalanx. The thumb has only two phalanges, proximal and distal. All five digits have metacarophalangeal (MP) and interphalangeal (IP) joints. However, the thumb has only one IP joint, while the other four digits have both a distal interphalangeal (DIP) and proximal interphalangeal (PIP) joint.
Classification
Phalangeal fractures are classified as follows:
•Phalanx involved: distal, middle or proximal phalanx
•Location within the bone: base, shaft, neck, or head
•Pattern: transverse, spiral, oblique, or comminuted
•Displaced or nondisplaced
•Intraarticular or extraarticular
•Closed or open
•Stable or unstable
•Deformity: angulation, rotation, or shortening
•Associated injuries: skin, tendon, nerve, or vessel
Treatment
First and foremost, treat the patient, not the radiograph. Most stable fractures can be treated successfully by nonoperative means. These fractures are functionally stable before or after closed reduction and do well with splinting and/or buddy taping and early mobilization. The goal is restoration of normal function with the three “R’s”: reduction, retention, and rehabilitation. After accurate fracture reduction, the hand should be immobilized in the intrinsic plus or safe position
91with extremity elevation to minimize edema. Movement of the uninvolved fingers should be permitted to prevent stiffness. An exercise program should be directed toward the specific fracture with early mobilization of the injured finger. Repeat radiographs should be performed at 7-10 days to check the reduction. It is important to remember that the PIP joint is the most important joint in the fingers.
Unstable fractures cannot be reduced with a closed method or, if reduced, cannot be held in the reduced position without supplemental fixation. Closed reduction with percutaneous pinning (CRPP) or open reduction with internal fixation (ORIF) are required to provide stability and allow early mobilization. Indications for internal fixation include:
•Uncontrollable rotation, angulation, or shortening
•Multiple digit fractures that are difficult to control
•Displaced intraarticular fractures involving more than 15-20% of the articular surface
•Fracture-subluxation of the thumb and fifth finger carpometacarpal joints
•Unstable fractures: failure of closed manipulation, as in spiral fractures of the proximal phalanx or transverse metacarpal fractures
•Metacarpal head fractures
•Open fractures

Injuries of the Finger |
555 |
For nondisplaced fractures treated in closed fashion, motion can be started within 3 weeks if the fracture is stable. Midshaft proximal phalangeal fractures require 5-7 weeks for complete bony healing. Midshaft middle phalangeal fractures require 10-14 weeks for radiographic healing of the cortical portion of the bone. Fractures requiring open reduction or severely comminuted fractures with disruption of the periosteum take twice as long to heal as simple fractures.
Complications
Loss of motion secondary to tendon adherence at the fracture site and contractures, especially at the PIP joint, are complications of phalangeal fractures. Malunion secondary to volar angulation after fractures near the base of the proximal phalanx may occur. There may be malrotation after spiral or oblique proximal and middle phalangeal fractures. Phalangeal fractures that have been percutaneously fixed may be complicated by pin tract infection. Nonunion results from bone loss, soft tissue interposition, inadequate immobilization or distraction at the fracture site.
Interphalangeal Injuries
IP injuries are subluxations or dislocations secondary to ligament or tendon injury. Joint subluxations occur with disruption of the joint’s soft tissue supporting structures, but with some contact remaining between the joint surfaces. A dislocation is an injury that causes a phalanx to move out of its normal alignment with another phalanx with total loss of contact between the joint surfaces. Dislocations of the DIP joints are rare, usually dorsal, and caused by hyperextension. Dislocations of the PIP joint are most commonly dorsal but can also be volar and rotated in either direction.
Anatomy
The proximal, distal, and thumb IP joints are true hinge joints. Joint stability is provided by the three structures: radial and ulnar collateral ligaments, the volar plate, and the dorsal capsule. The dorsal capsule is very thin and provides minimal stability to the joint. The collateral ligaments and the volar plate are firm structures. 91 The collateral ligaments limit side-to-side movement of the DIP and PIP joints. For dislocation to occur, at least two of these three structures must be disrupted.
Classification
Classification can be based on the status of the skin (closed versus open), the duration of injury (acute versus chronic), the degree of joint displacement (subluxation versus dislocation), the status of the joint surface (dislocation versus fracture-dislocation) and the ability to reduce the joint dislocation (simple versus complex). Joint dislocations and subluxations can be further subclassified based on the direction of displacement of the distal portion of the injured digit relative to the proximal portion (dorsal, volar, lateral, or medial).
Treatment
DIP Joints
Dislocations
To manage acute dorsal DIP joint dislocations, perform a closed reduction, with or without digital block anesthesia, using longitudinal traction of the distal phalanx.
556 |
Practical Plastic Surgery |
Place direct pressure on the dorsal base of the distal phalanx, displacing it distally and palmarly. Postreduction radiographs should confirm congruous reduction in the joint. After joint reduction, assess joint stability and flexor and extensor tendon function. If joint instability is present after joint reduction, splint the joint for 2 to 3 weeks in 10°-20° of flexion. With acute volar DIP dislocations, avoid splinting the DIP joint in hyperextension to prevent dorsal skin wound problems. Splint the digit for 6 weeks or more to promote healing. Open dislocations of the DIP joint require irrigation, debridement, and antibiotics. When the dislocation is chronic (greater than 3 weeks) or irreducible, perform an open reduction. Irreducible DIP joint dislocations may be secondary to an interposed structure, such as the volar plate, a flexor tendon, a fracture fragment or a sesamoid bone. Remove the interposed structure to reduce the joint.
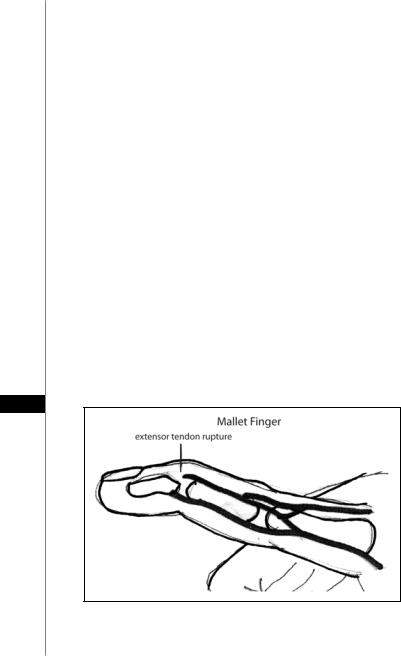
Distal Extensor and Flexor Tendon Rupture/Avulsion
Disruption of the extensor mechanism occurs if there is a sudden forceful flexion of the extended DIP joint. This results in either a disruption of the extensor tendon or an avulsion fracture with varying amounts of bone involvement. On examination, there is a characteristic flexion deformity at the DIP joint and the inability to actively extend this joint, which is known as mallet finger (Fig. 91.4). The treatment consists of continuous splinting of the DIP joint in full extension or even slight hyperextension for a minimum of 6 weeks, followed by night splinting for an additional 2 weeks. The importance of continuous splinting must be stressed because even momentary flexion of the DIP joint during the treatment period could result in resetting the treatment period back to time zero. Splinting can be effective even if initiated several weeks after the injury. Surgery is recommended for those patients with joint subluxation despite splinting, for displaced avulsion fractures with a large articular component (more than 50%). Failed splinting will also require surgery: K-wire fixation of the DIP joint in extension is usually adequate.
91
Figure 91.4. The mallet finger deformity. Disruption of the extensor tendon or an avulsion fracture causes a characteristic flexion deformity at the DIP joint and the inability to actively extend this joint.
Injuries of the Finger |
557 |
|
|
|
|
|
|
|
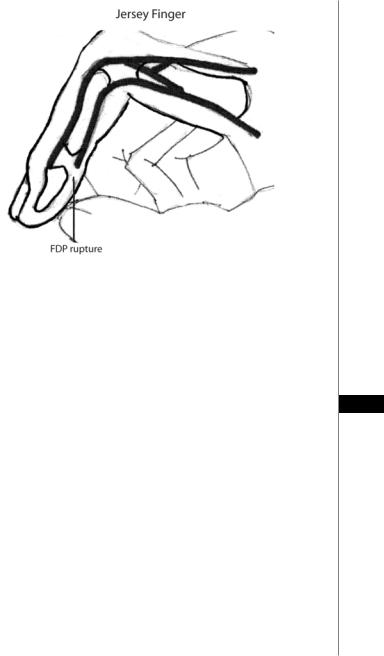
Figure 91.5. The jersey finger deformity. Forced extension of the maximally flexed DIP joint can cause avulsion of the FDP tendon, commonly a result of the ring finger catching on another player’s jersey.
Avulsion of the flexor digitorum profundus tendon, “jersey finger,” results from forced extension of the maximally flexed DIP joint, commonly a result of the ring finger catching on another player’s jersey (Fig. 91.5). The patient presents with the loss of the normal cascade of the fingers and the inability to flex the DIP joint actively. If the tendon retracts into the palm (Type 1 injury), urgent repair is necessary to avoid
progressive degeneration. If the tendon retracts to the level of the PIP joint (Type 2 91 injury) or is associated with a large avulsion fracture that causes the tendon to be held
up at the DIP joint (Type 3 injury), early surgical intervention is preferable. However, these injuries can be repaired as late as 6 weeks after the injury. When these injuries present even later than 6 weeks, “salvage surgery” directed at the DIP joint with either DIP capsulodesis, or DIP joint fusion can be performed.
DIP Ligamentous Injuries
A ligament may be torn by a forceful stretch or blow, leaving the joint unstable and prone to further injury. Unless they accompany a dislocation, nearly all ligament injuries of the DIP joint are partial tears or sprains and thus can be treated nonoperatively. Temporary splinting for a few days for comfort should be followed by an early, vigorous active motion program.
PIP Joints
Dislocations
PIP joint dislocations are frequently associated with an injury to the volar plate, collateral ligament, extensor tendon (central slip) and/or joint articular surface. Dorsal PIP injuries without fracture can usually be reduced by closed means. A digital
558 |
Practical Plastic Surgery |
block is often unnecessary. The volar plate, by necessity is ruptured, usually from the middle phalanx, but the collateral ligaments are rarely ruptured completely from their attachments. Perform reduction with longitudinal traction and direct pressure on the dorsal base of the middle phalanx, displacing it distally and palmarly. Confirm congruous reduction of the joint with post-reduction radiographs. Assess both active and passive stability of the joint after reduction. For stable joints, use a resting splint with the finger compressed and almost fully extended until the digit is pain-free enough to begin early active motion. Protect against hyperextension during early motion by buddy taping the digit to the adjacent finger. Alternatively, one can use an orthoplast hand-based splint to avoid hyperextension. Protect the injured digit, especially during sporting events, by buddy taping it to an adjacent uninjured digit. Reassure the patient that persistent edema and slow resolution of stiffness is expected and continue to compress the digit at night. Decisions for the need for physical therapy can be made after several weeks of observation. Open PIP joint dislocations should be treated with irrigation, debridement, and antibiotics. Chronic and irreducible dorsal PIP dislocations are not common and require open reduction.
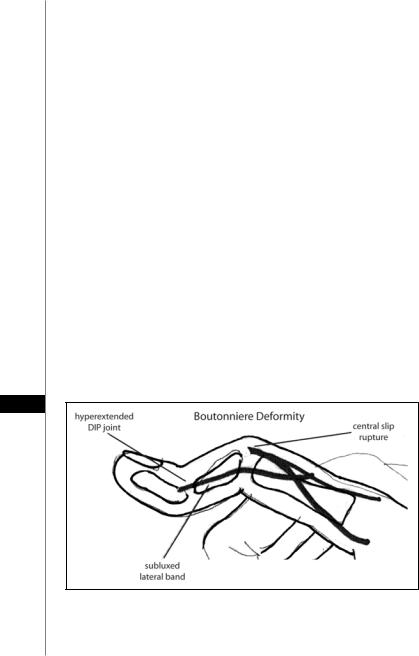
Proximal Extensor and Flexor Tendon Rupture/Avulsion
Palmar PIP joint dislocations involve disruption of the extensor mechanism (central slip) from either forced flexion of the extended PIP joint or a forced volar dislocation of the middle phalanx on the proximal phalanx. The resulting boutonniere deformity leads to not only a flexion deformity of the PIP joint but also a hyperextension of the DIP joint (Fig. 91.6). This characteristic deformity may take several weeks to develop. Therefore, an acutely edematous and tender PIP joint with weak active extension and dorsal tenderness should be treated even in the absence of the classic deformity. It is distinguished from the pseudoboutonniere deformity in that, although active extension is weak or not possible, full passive extension of the PIP joint is easily achieved, and hyperextension of the DIP joint does not exist. Treatment consists of an extension splint immobilizing only the PIP joint worn for a
91
Figure 91.6. The boutonniere deformity. There is a flexion deformity of the PIP joint and a hyperextension of the DIP joint due to disruption of the extensor mechanism. This can occur as a result of forced flexion of the extended PIP joint or forced volar dislocation of the middle phalanx on the proximal phalanx.

Injuries of the Finger |
559 |
minimum of 4 weeks, followed by progressive weaning and nighttime splinting for another 3 weeks. Similar to mallet finger immobilization, maintenance of continuous extension without flexion of the joint should be strictly enforced. Even in the setting of the chronic boutonniere deformity, splinting is the first line of treatment, since surgery often does not provide satisfactory results. Reconstruction is reserved for symptomatic, chronic deformity that fails nonoperative measures.
There are two chapters in this text devoted entirely to lacerations of extensor and flexor tendons.
PIP Ligamentous Injuries
A ligament may be torn by a forceful stretch or blow, leaving the joint unstable and prone to further injury. Forced radial deviation of the thumb results in trauma to the dorsal capsule, the ulnar collateral ligament (UCL), and the ulnar aspect of the volar plate at the MP joint. This injury, known as gamekeeper’s thumb or skier’s thumb, occurs most often when a skier falls on his or her pole with an open hand. Partial tears can usually be managed nonoperatively with a thumb-spica cast. This injury is managed with open repair of the ulnar collateral ligament through an ulnar incision. A Stener’s lesion occurs when the UCL is trapped above the adductor aponeurosis preventing proper healing. The ligament is repaired, and bony avulsions are reduced and stabilized with Kirschner wires, a pullout wire, or screws. Postoperatively the hand is splinted from the IP joint to the elbow for 4 weeks for bony avulsions and 6 weeks for ligament repairs.
Volar Plate Ruptures
Volar plate ruptures of the PIP joint can result from a dorsal PIP joint dislocation or hyperextension injury. The volar plate usually detaches from the middle phalanx, with or without a piece of bone. This injury must be differentiated from the PIP joint fracture-dislocations in which the large size of the intraarticular fracture fragment renders the joint either unstable at full extension, or in a chronically dislocated state. Treat the mild volar plate fracture with a stable joint as any other volar plate injury, with protection against hyperextension by either a temporary
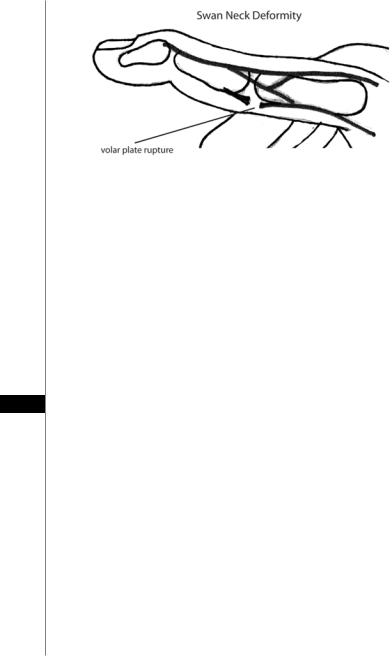
dorsal-block digital splint or by strapping to an adjacent finger for 3 weeks. Encour- 91 age full flexion. Chronic volar plate ruptures can result in a swan neck deformity
(Fig. 91.7). The untreated mallet finger can also lead to hyperextension of the PIP joint from unopposed and overactive pull of the extensor mechanism of the middle phalanx, also resulting in a swan-neck deformity. If the swan neck deformity is secondary to chronic volar plate rupture, nonoperative treatment includes use of an orthoplast splint or a silver, double-ring splint to help PIP joint hyperextension. Symptomatic volar plate ruptures can be helped by surgical intervention, specifically late reattachment or shortening of the volar plate, with or without some form of volar reinforcement.
Complications
Ligament and tendon injury requires joint immobilization and may require operative repair. Joint stiffness can occur and may be further worsened by intraarticular edema and resulting fibrosis. Early joint motion minimizes postinjury stiffness, but preference must be given to joint immobilization until adequate ligament stability has developed. The most common complication of gamekeeper’s thumb is instability of the MCP joint due to failure of repair. It is managed with ligamentous reconstruction with a tendon graft or MCP joint arthrodesis.
560 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 91.7. The swan neck deformity. There is a flexion deformity of the DIP joint and hyperextension of the PIP joint. Chronic volar plate ruptures can lead to this deformity. The untreated mallet finger can also lead to hyperextension of the PIP joint from unopposed and overactive pull of the extensor mechanism of the middle phalanx, also resulting in a swan-neck deformity.
Pearls and Pitfalls
•Mobilization of an injured digit by 3 weeks significantly decreases the chance of permanent loss of motion. The patient should be told to open and close their hand “against air”, and to strive for motion rather than strength.
•The more unstable the reduced dislocation or fracture, the more the injury will require surgical stabilization.
•Rotational deformities do not improve with time and are a strong indication for operative repair.
•One trick that can help when using a removed fingernail as a protective dressing is to dermabond it to the nail bed. It will stay stuck for 1-3 weeks.
91Suggested Reading
1.Allen M. Conservative management of fingertip injuries in adults. The Hand 1980; 12:257.
2.Craig SM. Anatomy of the joints of the fingers. Hand Clin 1992; 8:693.
3.Dray GJ, Eaton RG. In: Green DP, ed. Dislocations and Ligament Injuries in the Digits. Operative Hand Surgery 1978; 3:149.
4.Fassler PR. Fingertip injuries: Evaluation and treatment. J Am Acad Orthop Surg 1996; 4:84.
5.Hart RG, Kleinert HE. Fingertip and nailbed injuries. Emerg Med Clin North Am 1993; 11:755.
6.Rosenthal EA. Treatment of fingertip and nail bed injuries. Orthop Clin North Am 1983; 14:675.
7.Russell RC, Cases L. Management of fingertip injuries. Upper Extremity Trauma and Reconstruction 1989; 94:1298.
8.Van Beek AL, Kassan MA, Adson MH et al. Management of acute fingernail injuries. Hand Clin 1990; 6:23.
9.Zook EG. Anatomy and physiology of the perionychium. Hand Clin 1990; 6:1.