
Practical Plastic Surgery
.pdf
542 |
Practical Plastic Surgery |
Contraindications to primary tendon repair include: massive soft tissue injuries to the fingers or palm; inadequate skin coverage over the repair; or gross wound contamination. Some surgeons will delay primary repair if the skeletal damage is so severe that postoperative mobilization would not be possible.
Operative Technique
Since tendon transfers, tendon grafts, and arthrodesis are discussed elsewhere in this book, the focus of this chapter is primary repair.
Exposure
Rarely can the entire procedure be performed through the site of injury. There are many options for placement of the incision (Fig. 90.3). Lacerations can be extended in appropriate cases. However, if the neurovascular structures need to be explored, greater exposure is necessary. Longer incisions are usually performed in a zigzag fashion so that flexion lines in the palm and fingers are not crossed at 90˚ angles in order to avoid scar contracture. The surgeon must consider the position of the hand at the time of injury to determine if the tendon ends are likely to be retracted.
Tendon Retrieval
To prevent adhesions, atraumatic technique is essential. Tendon ends do not usually require debridement or shortening. It is important to keep the tendons moist throughout the procedure. In Zone I injuries involving the FDP tendon, retrieval is
90
Figure 90.3. Skin incisions for exposure during flexor tendon repair. Whenever possible, the skin laceration should be incorporated into the incision. Flexion lines in the palm and fingers should not be crossed at 90˚.
Flexor Tendon Repair |
543 |
not usually difficult since the vincula help to anchor the tendon in place. If the DIP joint was flexed at the time of injury, the proximal stump can be retrieved by opening the cruciate pulleys (the A4 pulley should be preserved). A suture placed in the tendon can be used to pull it through the A4 pulley. Piercing the tendon transversely with a 25-guage needle can anchor it in place during repair.
In zone II injuries, the neurovascular bundles should be identified first. Either the C1 or C2 pulley is opened, whereas the A1-A4 pulleys should be preserved whenever possible. If the proximal stump is close and can be visualized, it should be carefully retrieved. A commonly described technique uses a skin hook to snare the tendon. Occasionally, “milking” the tendon towards the incision is sufficient.
If the proximal stump cannot be visualized, the Sourmelis and McGrouther technique is an excellent option. A catheter is passed through the tendon sheath from distal to proximal. The tip of the catheter is exposed via a mid palm incision proximal to the A1 pulley. The catheter is sutured to both tendons and then it is pulled distally, bringing the proximal tendon ends into contact with the distal stumps.
It is critical to ensure that the relationship of FDP and FDS at Camper’s chiasma is maintained. Flexing the DIP and PIP joints will help deliver the distal stump of the FDS or FDP tendons. If insufficient distal tendon is exposed, the distal cruciate synovial sheath should be opened.
If there is insufficient remaining distal FDP stump, the proximal FDP tendon can be anchored to the base of the distal phalanx. A periosteal flap is elevated and a hole is drilled in the bone. A 3-0 suture is placed in the proximal tendon stump and passed through the bone hole to pull the tendon under the periosteal flap. The suture ends are tied over a piece of cotton and a pad-button placed over the nail. An alternative technique involves the use of bone anchors in the distal phalanx.
Suture Technique
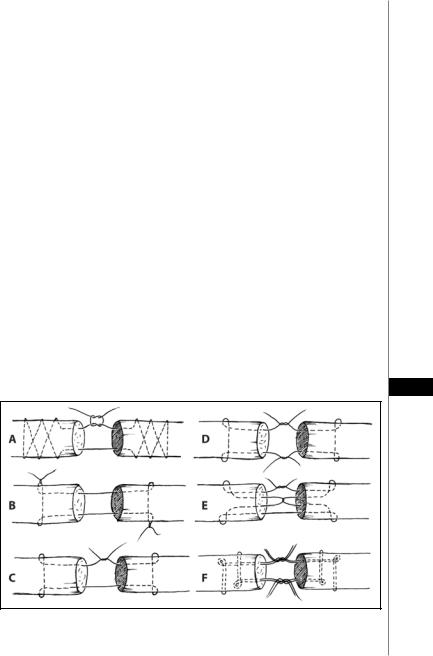
A variety of suturing techniques have been described (Fig. 90.4). 3-0 or 4-0 braided
polyester sutures are best. Locking loops are not necessary and may in fact collapse and
90
Figure 90.4. Representative techniques of end-to-end flexor tendon repair. A) Bunnell repair. B) Kessler grasping repair. C) The original Kessler repair. D) Kessler-Tajima modified repair. E) Interlock repair. F) Double loop repair.

544 |
Practical Plastic Surgery |
lead to gaping. The strength of the repair is proportional to the number of sutures crossing the repair site. Studies have shown that six strands are needed in order to provide a maximally strong repair; however a six-strand repair is technically difficult and may compromise tendon nutrition and healing. As such, most surgeons use a four-strand repair. If one of the two-strand repairs shown in Figure 90.4 is used, an additional horizontal mattress stitch is placed to make it a 4-strand repair.
At the completion of the repair, an epitendinous repair using 5-0 or 6-0 monofilament suture should be run circumferentially around the repair site. This will increase the strength of the repair by up to 20% and decrease the likelihood of gaping. A number of techniques have been described, including a simple running stitch, a running lock loop, a continuous horizontal mattress, and a running-lock suture. The horizontal mattress and running-lock stitch have been shown to be the strongest.
There is ongoing debate as to the benefit of repairing the tendon sheath. Potential advantages include improved tendon nutrition, biomechanics and rate of healing. Disadvantages include the potential for narrowing, which can restrict gliding, and the technical difficulty of sheath repair.
Pulley Reconstruction
It is important to reconstruct the annular pulleys. As a minimum, the A2 and A4 pulleys should be repaired using autogenous material such as tendon, extensor retinaculum, volar plate, or fascia lata. One common technique is the Okutsu “triple loop” method which uses three loops of autogenous material encircling both the tendon and the entire bone. Most autogenous reconstructions, however, become lax with time resulting in bow-stringing of the tendon. The use of alternative alloplastic materials, such as PTFE (Gore-Tex), has shown promise in animal models in terms of biomechanical outcomes, adhesion formation, and foreign body reaction.
Tendon Rupture and Avulsions
90 Normal tendons usually rupture at their insertion or at the musculotendinous junction. Rupture within the substance of the tendon is unusual and is associated with conditions that weaken the tendon such as rheumatoid arthritis, infection, gout, and prior fractures. Treatment often requires tendon grafts or transfers.
Traumatic avulsions tend to occur as a result of forced extension in young males playing contact sports. The FDP tendon, especially in the ring finger, is most commonly involved. Isolated FDS rupture is rare. Severe injuries involve the avulsion of a fragment of bone along with the tendon. Treatment consists of reinserting the tendon into the base of the phalanx using a pullout suture tied over a button or recreating the tendon insertion using bone anchors. Bony avulsion requires open reduction and internal fixation of the bone fragment.
Tendon Healing
Intrinsic Healing
The first 72 hours after repair comprises the inflammatory phase, which includes neovascularization and the arrival of inflammatory cells. This is followed by a 4-week proliferative phase during which collagen and granulation tissue are formed. The remodelling phase, in which the collagen becomes organized and cross-linked, continues after this for 16 weeks. During the inflammatory phase, the strength of the repair is almost entirely due to the strength of the suture. In the early prolifera-

Flexor Tendon Repair |
545 |
tive phase, the strength of the repair decreases. This loss of repair strength can be lessened by stressing the tendon by means of early mobilization with passive motion. During remodelling, the strength of the repair increases toward normal.
Extrinsic Healing
Extrinsic healing produces scar tissue and adhesions between the tendon and the surrounding soft tissues. Early mobilization with passive motion exercises can help decrease this adhesion formation while maximizing tendon excursion. Factors that can worsen adhesion formation are prolonged immobilization, tendon ischemia (e.g., vincula disruption), gaping at the repair site, discontinuity of the sheath, or trauma to the tendon or sheath.
Postoperative Care and Rehabilitation
A large, bulky, compressive dressing should be used. The hand should be immobilized and splinted in the safe position: wrist in midflexion, MP joints flexed 90˚, fingers in full extension. The use of postoperative antibiotics depends on the mechanism of injury and expected risk of infection.
Numerous studies have shown that early postoperative motion stress exercises are beneficial. Repairs that are completely immobilized are half as strong at 3 weeks. This difference between the strength of mobilized and immobilized repairs continues to grow as time progresses. According to Strickland, a good rehabilitation regimen should include the following:
•The wrist and MP joints should be flexed at rest
•The PIP and DIP joints are extended at rest
•Passive flexion of the MP, PIP and DIP joints before wrist extension
•Maintenance of passive digital flexion with the wrist extended
•Frequent application of motion stress
The use of the Kleinert splint after flexor tendon repair has been popular among
hand surgeons. This splint maintains the wrist in partial flexion. The tip of the finger is attached to the volar surface of the forearm with a rubber band, allowing for 90 active extension and passive rubber band flexion. Many modifications of the origi-
nal Kleinert splint are in use today. Full use of the hand should be restricted until 8-12 weeks post repair.
The main complications from primary flexor tendon repair are rupture of the repair (incidence of about 5%), adhesion formation, and joint contracture, a late complication.
Pearls and Pitfalls
•It is essential to use a delicate, atraumatic technique when handling the severed ends of a tendon. Since the entire length of tendon may be required, one cannot rely on “freshening” of the edges to remove any traumatized portions of tendon.
•In zone I injuries of the FDP tendon, anchoring the distal tendon to bone provides a stronger repair than suturing the two ends of tendon back together. However, the FDP tendon should not be advanced more than 1 cm towards the insertion on the distal phalanx since this could result in the quadriga effect.
•If a tendon graft is required, palmaris longus is the best option. If not present, plantaris or extensor tendons of the toes can be used. The needed length of graft can be determined by matching the position of the injured finger to the cascade of the uninjured fingers. The amount of tendon shortening is measured as the finger is brought into the normal cascade.

546 |
Practical Plastic Surgery |
•In grossly contaminated wounds involving flexor tendon injury, repair should be delayed since the risk of infection is high. Once the wound is clean and free of necrotic tissue and purulence, delayed primary repair or reconstruction can be undertaken.
•Establishment of the correct relationship between FDS and FDP (Camper’s chiasma) is essential. This can be difficult when the proximal tendon ends have retracted into the palm.
•Since fingers are often flexed during the time of injury, the tendon laceration is usually distal to the skin laceration.
•When the two ends of the tendon are approximated, the epitenon should be carefully preserved and also brought into approximation. After repair of the tendon with the internal sutures, an epitendinous repair should be performed.
Suggested Reading
1.Brunner JM. The zig-zag volar-digital incision for flexor-tendon surgery. Plast Reconstr Surg 1967; 40:571.
2.Idler RS. Anatomy and biomechanics of the digital flexor tendons. Hand Clin 1985; 1:3.
3.Leffert RD, Weiss C, Athansoulis CA. The vincula; with particular reference to their vessels and nerves. J Bone Joint Surg 1974; 56A:1191.
4.Strickland JW. Flexor tendon injuries: I. Foundations of treatment. J Am Acad Orthop Surg 1995; 3:44.
5.Strickland JW. Flexor tendon injuries: II. Operative technique. J Am Acad Orthop Surg 1995; 3:55.
6.Strickland JW. Development of flexor tendon surgery: Twenty-five years of progress. J Hand Surg 2000; 25A:214.
90

548 |
Practical Plastic Surgery |
insertion of the flexor and extensor tendons. Although maintenance of length, preservation of the nail, and appearance are important, the primary goal of treatment is a painless fingertip with durable and sensate skin. Considerable hand dysfunction results when a painful fingertip causes the patient to exclude the digit from use. The specific wound characteristics determine which method of treatment is optimal for a given patient. It is important to know whether there has been loss of skin or pulp and the extent of such loss. The presence of exposed bone or injury to the nail bed or perionychial tissue must be determined. In the case of amputations, it is important to establish the level and angle of injury.
Anatomy
The fingertip is the end organ for touch and is supplied with special sensory receptors that enable the hand to relay the shape, temperature, and texture of an object. The skin covering the pulp of the finger is very durable and has a thick epidermis with deep papillary ridges. The glabrous skin of the fingertip is well-suited for pinch and grasp functions. Its volar surface consists of a fatty pulp covered by highly innervated skin. The skin of the fingertip is firmly anchored to the underlying terminal phalanx by multiple fibrous septa that traverse the fatty pulp.
Classification
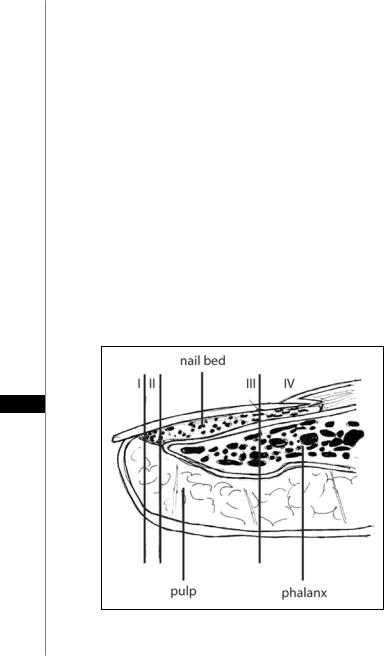
Allen has classified fingertip injuries based on the level of injury (Fig. 91.1):
•Type 1 injuries involve only the pulp
•Type 2 injuries involve the pulp and the nail bed
•Type 3 injuries include partial loss of the distal phalanx
•Type 4 injuries are proximal to the lunula
91
Figure 91.1. Classification of fingertip injuries. Type 1 injuries involve only the pulp; Type 2 injuries involve the pulp and the nail bed; Type 3 injuries include partial loss of the distal phalanx; Type 4 injuries are proximal to the lunula.
Injuries of the Finger |
549 |
|
|
|
|
|
|
|
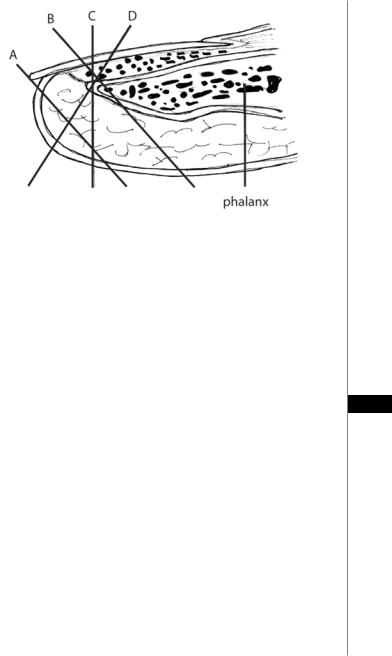
Figure 91.2. The angles of fingertip amputation. A, volar oblique without exposed |
|
bone. B, volar oblique with exposed bone. C, transverse with exposed bone. D, |
|
dorsal oblique with exposed bone. |
|
This classification is useful to help generate a treatment plan. Additionally, tip |
|
amputations should be described in terms of the angle of injury—dorsal oblique, |
|
transverse, and volar oblique, as well as the presence of exposed bone (Fig. 91.2). |
|
Treatment |
|
Type 1 injuries may heal quite well by secondary intention. In contrast, Types 3 |
|
and 4 often require some type of flap coverage. Dorsal oblique and transverse inju- |
|
ries are more suited to local flaps. Volar oblique injuries often require a regional flap. |
|
Type 2 injuries require nail bed repair, which is discussed in the next section. |
91 |
|
Healing by Secondary Intention
The simplest treatment of fingertip injuries is to allow the wound to heal by secondary intention. It is reserved for small defects (8 to 10 mm2 ), with minimal bone exposure and minimal loss of tissue pulp. Local wound care should be performed 2 to 3 times daily with dressing changes. Healing is usually complete by 3 to 6 weeks depending on the size of the defect. In young children, this method provides good results even if larger areas of exposed bone.
Composite Grafts
If an amputated part has been recovered and it is clean and of adequate integrity, use the part for soft tissue coverage. If there is no exposed bone, de-fat the skin and suture it onto the defect. This piece will now function as a full-thickness skin graft. Minimize its thickness to enhance its chances of “taking.” Even if this skin necroses it will still serve as a biologic dressing.
Revision Amputation
A simpler course of action involves shortening the digit or revision amputation. This procedure is indicated in situations in which bone is significantly degloved, and the angle of the injury is such that other options are not appropriate. Take care to limit

550 |
Practical Plastic Surgery |
loss of length, particularly in treating the thumb. This procedure can be performed under local anesthesia in the acute care setting. Develop the flaps to cover the tip of the digit, preferably with volar skin. Using the volar skin rather than the dorsal skin provides a more padded and durable soft tissue cover for the fingertip. Patients can return to their activities as tolerated when the soft tissues have healed.
Skin Grafts
Skin grafts can be used in fingertip injuries where there is skin loss, but adequate subcutaneous tissue is present with no exposed bone. The lack of exposed bone is paramount because skin grafts will not “take” well on bone without intact periosteum. Use this technique for injuries with skin loss of greater than 1.5 cm2. In cases of smaller skin defects, allow the wound to heal by secondary intention. Full-thickness skin grafts provide better sensibility and durability, as well as a better cosmetic result. On the other hand, split-thickness skin grafts have a greater likelihood of “taking.” Excellent hemostasis of the injury site must be obtained to avoid postoperative hematoma formation. Secure the graft with a bolster dressing that is left undisturbed for 5 to 7 days. Start physical therapy after the dressing is removed.
Local Flaps
Local flaps use adjacent local skin with its subcutaneous tissue and normal sensory end organs to cover defects. There are two common advancement flaps used for fingertip injuries—the V-Y advancement flap and the homodigital triangular flap. Both share similar principles in that a “V” incision is made adjacent to the defect. The skin and subcutaneous tissues are advanced forward, and the proximal defect is closed end-to-end. After closure, the proximal portion of the wound forms the vertical line of the “Y.” The homodigital triangular flap, which is dissected more proximally, includes the digital artery within the flap. Range of motion therapy is started 7 to 10 days following local advancement flaps. These flaps are described in Chapter 92.
Regional and Distant Flaps
Regional flaps are defined as flaps taken from other parts of the hand that do not
91use tissue adjacent to the defect. They are well-suited for volar oblique type injuries. Owing to the postoperative immobilization required, the procedure is often discouraged in patients predisposed to finger stiffness. This includes patients older than 50 years of age, those with rheumatoid arthritis, and patients with multiple injured digits. These flaps are also not well suited for young children because of lack of compliance and the fact that simpler methods are usually adequate.
Distant flaps are defined as flaps obtained from areas of the body other than the injured limb and are primarily free-flaps. These procedures are considered in hand injuries with large soft tissue defects and provide thick, fatty coverage with little sensibility. The flaps can be developed from the chest, abdomen, groin, or opposite arm. A more extensive discussion of regional hand flaps can be found in Chapter 92.
Thumb Coverage
The thumb plays a crucial role in prehension and is involved in 50% of the function of the hand. Preservation of length of the thumb is more important functionally than in any other digit. For soft tissue defects that cannot be covered with a V-Y flap and for those measuring no more than about 2 cm in length, the Moberg advancement flap is the procedure of choice because it preserves length and tactile sensibility. For loss of more than two-thirds of the pulp tissue, a cross-finger flap from the dorsal
Injuries of the Finger |
551 |
aspect of the middle finger or a first dorsal metacarpal artery-island pedicle flap from the index finger usually provides satisfactory padding of the thumb and adequate sensibility. The neurovascular-island flap can help restore sensibility and padding to the ulnar side of the thumb pulp if other methods have proved unsatisfactory.
Complications
Cold intolerance after fingertip injury is common. Symptoms rarely resolve but may become more tolerable over time. Failure to resect a sufficient length of each digital nerve stump to avoid neuroma formation results in a persistently painful finger. Complications of skin grafts include hematoma, necrosis of the skin graft, and donor site complications. The resultant suture line in advancement flaps may be the cause of hypersensitivity noted by some patients. Advancement flap complications also include numbness, cold intolerance, and dysesthesias.
Fingernail and Nail Bed Injuries
The fingernail and the underlying nail bed are the most commonly injured part of the hand. The nail bed, which is the supportive tissue underneath the nail, can be damaged by laceration or crush. Development of a subungual hematoma invariably reflects nail bed injury with or without an associated fracture of the distal phalanx. Injuries of the nail bed can be divided into those that involve the germinal matrix and those that involve the sterile matrix. Germinal matrix injuries are generally more serious since nail formation originates from the germinal matrix, and an injury in this region has a higher likelihood of permanently affecting nail growth.
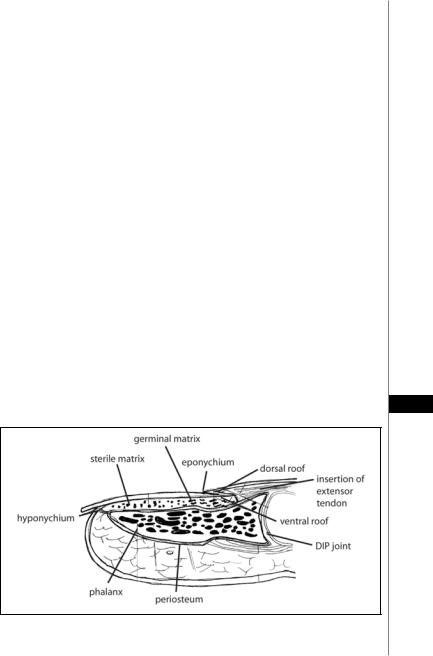
Anatomy
The fingernail protects the fingertip and has a major role in tactile sensation and fine motor skills. The nail complex, or perionychium, includes the nail plate, the nail bed, and the surrounding skin on the dorsum of the fingertip (paronychium). These structures are schematically shown in Figure 91.3. The fingernail is a plate of flattened cells layered together and adherent to one another. The nail bed lies imme-
diately deep to the fingernail. The nail bed is composed of the germinal matrix, the 91
Figure 91.3. Sagittal section of the distal finger illustrating the anatomy of the nail and nail bed.
