
Practical Plastic Surgery
.pdf

Finger and Metacarpal Fratures |
513 |
and functional outcome. A useful clinical test is to ask the patient to flex his fingers while observing the position of the nails and comparing them to the other hand. As a rule, all abnormal findings in the injured hand should be compared to the other hand as individual malformation or previous injuries may lead to an inaccurate diagnosis.
Fracture Patterns |
|
|
Phalangeal fractures can be classified according to the following: (1) open or |
|
|
closed; (2) displaced or nondisplaced; (3) the finger and phalanx involved; (4) frac- |
|
|
ture pattern: oblique, transverse, spiral, or comminuted; (5) any associated soft tis- |
|
|
sue or neurovascular injuries. |
|
|
Imaging |
|
|
Negative plain radiographs in three views (posterior-anterior, oblique and lat- |
|
|
eral) are ample for ruling out most phalangeal fractures. If necessary, additional |
|
|
stress views can be obtained in which the injured phalanx is manually stressed. Since |
|
|
this maneuver is usually painful, a digital block with lidocaine can be helpful. CT |
|
|
and MRI are not indicated for the diagnosis of a phalangeal fracture. |
|
|
Transverse fractures of the proximal phalanx are more likely to result in volar |
|
|
displacement of the distal fragment due to traction on the proximal bone by intrin- |
|
|
sic and extensor tendons. Middle phalanx fractures can result in distal fragment |
|
|
displacement either volarly or dorsally, depending on whether the fracture is proxi- |
|
|
mal or distal to the FDS insertion. Fractures of the distal phalanx are usually related |
|
|
to crush injury involving the nail bed. |
|
|
85 |
||
|
||
Treatment Principles |
|
|
The principal goals of treatment are complete functional restoration and full |
|
|
ROM of the injured finger. This is achieved through precise anatomical alignment |
|
|
(open or closed), and early mobilization. Full immobilization (e.g., splinting) should |
|
|
not exceed 3 weeks as the extensor and flexor tendon systems as well as the capsules |
|
|
will begin to irreversibly contract and stiffen. In general, uninvolved joints should |
|
|
be excluded from splinting (e.g., avoid splitting the PIP and MP joints in the setting |
|
|
of a distal phalanx fracture). A meticulous physical examination is key to detecting |
|
|
rotation deformities or poor anatomical reduction. Postreduction splinting plays an |
|
|
important role in the treatment of almost all fractures, and various finger splints are |
|
|
widely available in most acute care settings. Open fractures or extensive soft tissue |
|
|
injury should be treated with antibiotics and tetanus prophylaxis. |
|
|
Nonsurgical Treatment |
|
|
Treatment of finger fractures without any form of surgical fixation consists pri- |
|
|
marily of splinting. The aim of splinting is to immobilize the fractured segment and |
|
|
surrounding joints without interfering with the motion of the uninvolved joints. |
|
|
Stack splints are used to immobilize distal phalanx fractures while allowing full ROM |
|
|
of both the PIP and MP joints. |
|
|
Extraarticular, nondisplaced, stable phalangeal fractures are treated with closed re- |
|
|
duction, splinting and early rehabilitation. Closed reduction is performed using axial |
|
|
traction with concomitant alignment of the bone. For most shaft fractures of the middle |
|
|
or proximal phalanges, “buddy splinting” to the adjacent finger for 1-2 weeks is suffi- |
|
|
cient. In addition, radial or ulnar gutter splints are useful as they leave the remaining |
|
|
digits uninvolved. Postreduction films (2 views) should be obtained after closed reduc- |
|
|
tion and following one week to ensure continued fracture reduction. |
|

514 |
Practical Plastic Surgery |
Surgical Treatment
Surgical fixation and reduction are indicated for any of the following:
•Open fractures
•Unstable fractures
•Dislocated or intraarticular fractures
•Irreducible fractures
Proximal Phalanx Fractures
Different types of shaft fractures, such as transverse, oblique or spiral are in general considered to be unstable and require surgical fixation using two longitudinal K-wires. Intraarticular base fractures of the proximal phalanx are divided into three types: vertical shear fractures, compression fractures, and collateral ligament avulsions. The first two types may have impaction or rotated fragments. If this is the case, fixation is required. Stable and nondisplaced avulsion fractures are treated with splinting alone, using a buddy strap to the adjacent digit. If displacement is evident on radiographs, anatomic reduction is mandatory in order to prevent post-traumatic arthritis or persistent instability. Reduced vertical shear fractures should be stabilized using a percutaneous K-wire or an interfragmentary screw under image magnification. Fractures that have undergone bone-to-bone fixation can usually be mobilized the following day with a buddy strap to the adjacent finger. Ligament-to-bone repairs usually take longer to heal and should not be mobilized for 4 weeks. Compression fractures usually require open reduction with internal fixation (ORIF), especially if there is in an intraarticular
85step off of greater than 2 mm or visible angulation. Intrafragmentary screw fixation, mini-T, or minicondylar plates or used for internal fixation. The addition of a cancellous bone graft is useful to avoid over-compression and incongruity of the fragments.
Middle Phalanx Fractures
Middle phalanx fractures usually do better than proximal phalanx fractures since the DIP joint is functionally less important than the PIP or MP joints. Malunion, or post-traumatic arthrosis of the DIP joint is less severe than in the PIP or MP joints and can be treated without difficulty by arthrodesis. The vast majority of middle phalanx fractures are stable and well aligned. These can be treated with a buddy strap to the adjacent digit or gutter splints. Radiographs should be performed every 5 days for about 2 weeks to detect displacement. In the event of an unstable middle phalangeal shaft fracture, K-wire fixation is sufficient. Open fractures with extensive soft tissue damage may require ORIF.
If a shaft fracture is stable but malaligned after reduction, an extension block cast should be considered as it provides stabilization of the reduction and reduces the risk for PIP joint stiffness. The extension block should be maintained for 4 weeks followed by 2 weeks in a buddy strap. Rotational abnormalities should be ruled out by noting the alignment of the nail beds under active flexion of the fingers towards the palm and comparing them to the healthy hand. Malalignment of a fracture can occur in patients presenting weeks after the initial trauma, with a callus already present or soft tissue interposition. Often, these can no longer be reduced successfully in a closed fashion. Therefore, an ORIF is required, usually accompanied by an osteotomy along with tenolysis and capsulotomy.
Distal Phalanx Fractures
Distal phalangeal fractures are the most common finger fracture. Kaplan’s classification divides them into three types: Type A, or longitudinal; Type B, or comminuted;

Finger and Metacarpal Fratures |
515 |
and Type C or transverse. Type B fractures typically result from a crush injury. This often leads to an exquisitely painful subungual hematoma. Puncture of the nail with a heated paper clip works well to release the trapped blood. Up to 2 weeks of splinting with a Stax splint is sufficient for most cases. Transverse or longitudinal shaft fractures (Type A and C) are mostly stable with minimal displacement. The finger should be splinted (usually 3 to 4 weeks) until evidence of bony union is seen on radiographs. Open and unstable shaft fractures require K-wire fixation after alignment. A detached nail should be replaced and if necessary, secured with suture fixation. The nail helps protect the underlying matrix, prevents scar formation between the nail matrix and eponychium, and guides the direction of growth of the new nail.
Fractures of the base of the distal phalanx are usually unstable and tend to angulate in a dorsal fashion due to the traction of the extensor tendons. Closed fractures are treated by splinting (e.g., using Alumafoam) of the finger in extension for at least 4 weeks. Open fractures of the base are considered to be unstable and tend to have a rotational deformity. Retrograde K-wire fixation is a straight forward method of stabilization.
Condylar Fractures
Meticulous anatomic reduction is essential in condylar fractures, as malalignment can lead to a flexion contracture. A closed reduction will generally not provide an adequate result, requiring ORIF for reconstruction. Unicondylar fractures are usually unstable and often demonstrate a rotation deformity due to traction of the collateral ligament. If closed reduction is attempted by axial traction, a reduction clamp should be used to maintain the repositioned condyle and a 0.028 inch K-wire percutaneously inserted
through the uninjured condyle. Intraoperative films in all three dimensions should be 85 obtained to insure precise alignment of the small but functionally important fragment.
Metacarpal Fractures
Introduction
A fracture of the metacarpal is often termed a “boxer’s fracture” alluding to the etiology, which is usually direct or indirect trauma. Metacarpal fractures account for nearly 40% of all hand fractures. About a quarter of these are located in the neck of the 5th metacarpal bone.
The four metacarpals are tubular bones, each with an intrinsic arch. The 2nd and 3rd carpometacarpal (CMC) joints have almost no range of motion, whereas the 4th and 5th CMC joints provide 15˚ and 25˚ of relative motion, respectively.
Injuries of the metacarpal bone are clinically divided into fractures of the metacarpal base, the metacarpal shaft or neck and the metacarpal head.
Imaging
For most fractures, three-view conventional radiographs are sufficient. Severely comminuted or intraarticular fractures may also require stress views. CT scanning can be helpful for evaluation of questionable intraarticular involvement, since this can be difficult to determine on plain radiographs. The purpose of a CT scan in this setting is to assess the alignment or displacement of the fracture, and to aid in planning the operative approach.
Clinical Findings
Signs and symptoms include pain, hematoma, swelling, reduced motion and crepitus. These findings are common in metacarpal shaft fractures, while fractures of the metacarpal base and neck may have a subtle presentation.

|
516 |
Practical Plastic Surgery |
|
|
|
Fractures of the shaft tend to be shortened and rotated. Rotation deformities must be |
|
|
|
addressed; if untreated they pose a risk for a weakened grip and incomplete fist closure |
|
|
|
due to overlapping fingers. Fractures of the metacarpal base may be impacted since they |
|
|
|
are often caused by an axial load, making the diagnosis easy to miss. Fractures of the |
|
|
|
metacarpal head often present with nothing more than localized swelling and pain. Crepi- |
|
|
|
tus can be heard but should not be elicited since it has no additional diagnostic benefit. |
|
|
|
Treatment |
|
|
|
Most metacarpal fractures are adequately treated with closed reduction followed |
|
|
|
by immobilization in a forearm-based splint. two-view radiographs should be taken in |
|
|
|
the follow-up period in order to confirm that the reduction has been maintained. |
|
|
|
Early mobilization of wrist and fingers is absolutely critical to achieve optimal long-term |
|
|
|
functional results. Apex and dorsal angulation are often seen in shaft fractures. There |
|
|
|
is, however, a certain degree of angulation that is acceptable (up to 10˚ for the second |
|
|
|
and third, up to 20˚ for the fourth, and up to 30˚ for the fifth metacarpal). |
|
|
|
The following is a useful list of the indications for surgical treatment of a meta- |
|
|
|
carpal fracture: |
|
|
|
1. Open fractures |
|
|
|
2. Unstable and extensively displaced fractures requiring stabilization |
|
|
|
3. Nonreducible fractures |
|
|
|
4. Multiple fractures |
|
|
|
5. Old fractures that need to be reduced (>1 week post-trauma) |
|
|
|
6. Failure of nonsurgical treatment |
|
85 |
|
||
|
7. Fractures with extensive soft tissue injury |
|
|
|
|
|
|
Metacarpal Base Fractures
Most base fractures are impacted and are treated by splinting alone and early mobilization. Base fractures of the 5th metacarpal often require surgical treatment if displaced greater than 2 mm. Fractures involving the CMC joint are unstable and have a strong tendency to destabilize after a successful reduction due to traction forces of the surrounding ligaments. Therefore, CMC fractures often need open reduction with pin fixation. Postoperative splinting should be maintained for 2-3 weeks followed by mobilization. The pins should be removed after 6-8 weeks.
Metacarpal Shaft Fractures
In general, metacarpal shaft fractures are treated with reduction and splinting alone. The MP and PIP joint of the affected metacarpal bone are flexed to a 90˚ angle. Reduction is achieved with upward directed traction on the middle phalanx and downward resistance at the level of the proximal metacarpal shaft. Either splinting (extending to the distal palmar crease) or percutaneous pins are employed to maintain the reduction result.
First Metacarpal Fractures
Introduction
Thumb fractures are usually the result of occupational or sporting-related trauma. The thumb consists of a proximal and distal phalanx and a metacarpal bone. The first CMC joint is the articulation of the trapezium and the metacarpal base and provides a wide range of motion. It is stabilized by a number of ligaments, most importantly the anterior and posterior oblique ligaments, the intermetacarpal ligaments, and the dorsal radial ligament. The ROM of the MP joint of the thumb is extremely variable. It has relatively little intrinsic stability, and the stabilizing ligaments are prone to in-

Finger and Metacarpal Fratures |
517 |
jury. The ulnar and radial collateral ligaments stabilize the MP joint on its sides, and the volar plate stabilizes it on the palmar surface.
Fracture Patterns
Metacarpal fractures of the thumb are divided into base, shaft and head fractures. Typical signs of fracture are swelling, decreased range of motion, pain (most notably in base fractures) and occasional crepitus. Shaft fractures are rare due to the stable cortical bone structure and tend to result in apex-dorsal or apex-radial angulation. The most common fractures are of the metacarpal base, and these can be intraarticular (e.g., Bennet fracture) or extraarticular. Base fractures are usually due to a gently flexed metacarpal during an axial force. Adequate imaging of the CMC joint is essential in diagnosing a metacarpal base fracture: a true lateral view of the joint with the palm flat on the plate and wrist and hand pronated 15-35˚ is obtained. The imaging beam is aimed at the CMC joint from a 15˚ oblique angle from distal to proximal.
Extra-Articular
Extraarticular fractures are usually oblique or transverse. Closed reduction with a thumb spica cast for 4 weeks excluding the distal phalanx are usually sufficient. Reduction is obtained with axial traction, palmar directed pressure at the level of the fracture, and pronation of the distal fragment. Percutaneous pin fixation is indicated in cases of an unstable fracture postreduction (more likely in oblique fractures), open fractures, and fractures with angulation greater than 30˚ with shortening.
External or internal fixation is required for extensively comminuted fracture types. 85
Intra-Articular
The Bennett fracture is an intraarticular fracture of the metacarpal base with a volar-ulnar fragment of variable size. The fragment is often kept in anatomic position through the anterior oblique ligament. Restoring full anatomic congruity is mandatory to avoid post-traumatic arthritis. If articular incongruity is less than 2 mm postreduction, the fracture can be stabilized with percutaneous pin fixation. Open or unstable fractures, irreducible fractures, or those with an incongruity greater than 2 mm postreduction are indications for ORIF.
Pearls and Pitfalls
Fractures of the metacarpals and phalanges may be associated with ligamentous injuries (collateral ligaments or carpometacarpal ligaments), and therefore a careful examination for dislocations and joint instability must also be performed. Stiffness is a prime complication of a phalangeal injury. Early mobilization is key to optimal outcome (within 3-4 weeks of injury if possible). Differences in bony healing in the adult and pediatric population should also be recognized. Since children heal faster, they can be splinted for shorter duration compared to adults (with minimally displaced metacarpal fractures for example).
Suggested Reading
1.Blair WF, ed. Techniques in Hand Surgery. Baltimore, Maryland, USA: Williams and Wilkins, 179-284.
2.Stern PJ. Fractures of the metacarpals and phalanges. In: Green DP, Hotchkiss R, Pederson WC, eds. Green’s Operative Hand Surgery. 4th ed. New York: Churchill Livingstone, 1999.
3.Weiss AP, Hastings H. Distal unicondylar fractures of the proximal phalanx. J Hand Surg 1993; 18A:594.
4.Gonzales MH, Hall RF. Intramedullary fixation of metacarpal and proximal phalangeal fractures of the hand. Clin Orthop 1996; 327:47.
Brachial Plexus Injuries |
519 |
|
|
|
|
|
|
|
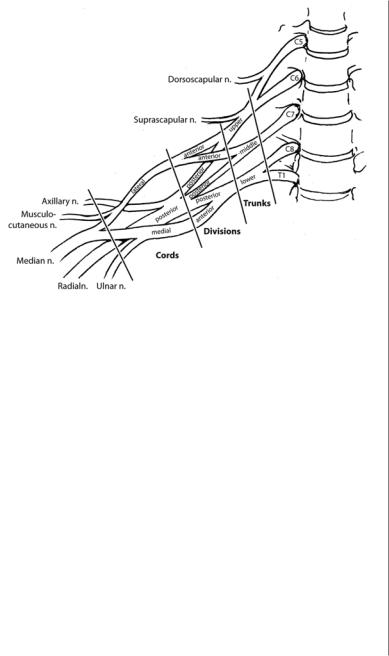
Figure 86.1. The brachial plexus. |
86 |
address life-threatening injuries. As such, the diagnosis of brachial plexus injuries is often delayed until overall stabilization has occurred and mental status has improved.
History and Physical
The mechanism of injury must be accurately determined since prognosis is intimately related to etiology. Manual muscle testing should include observation of muscle atrophy and tone. The British Medical Research Council grading system for muscle function is often helpful for standardized documentation of strength. Passive range of motion should be assessed to check for contractures, followed by active range of motion testing. Median, radial, and ulnar nerve function can be assessed by testing finger and wrist motion. The musculocutaneous nerve is responsible for elbow flexion. Abduction of the shoulder is dependent on the axillary nerve. The posterior cord can be assessed by checking finger and wrist extension, elbow extension, and shoulder abduction. The medial and lateral cords can be assessed via the medial and lateral pectoral nerves, which innervate the sternal and clavicular heads of the pectoralis major, respectively. The sensory examination must be thorough, and should include testing for Tinel’s sign at the supraclavicular fossa and the infraclavicular coracoid process.
Radiographic Evaluation
Plain film radiographic evaluation of the cervical spine and ipsilateral shoulder and scapula can delineate contributing bony injury or consequent bony deformity. Penetrating trauma in the setting of abnormal pulses suggests a hematoma-related
520 |
Practical Plastic Surgery |
plexopathy; an arteriogram may be helpful in this case. On CT myelogram, nerve root avulsion is suggested by demonstration of a meningocele, which results from tearing of the nerve root sleeve.
Injury Patterns
Determining the level of injury is critical to planning operative exposure, determining treatment modality, and assessing prognosis.
Preganglionic Injuries
Root avulsion refers to injury of the nerve root within the intervertebral foramen proximal to the sensory root ganglion. The spinal nerves are attached to the transverse processes in the lower cervical spine. As progressive traction is placed on the nerve root, these attachments are the first to break. The nerve root sleeve is then pulled through the intervertebral foramen and may tear, causing a meningocele. Finally, the nerve root itself avulses. Horner syndrome consists of ipsilateral meiosis, upper eyelid ptosis, and facial anhydrosis; it implies disruption to of the sympathetic fibers traveling through C8-T1 and suggests root avulsion at these levels. Winging of the scapula or weakness of the rhomboid suggests C5 or C6 root injury, respectively, since the long thoracic and dorsal scapular nerves arise from the nerve roots. Since no proximal stump is available for reconstruction, root avulsions may require neurotization.
Postganglionic Injuries
Postganglionic injuries, or ruptures, may have regenerative capacity and can of-
86ten be grafted. Supraclavicular injuries involve the spinal nerves, trunks, or divisions. They manifest most commonly as Erb’s palsy (C5-C6 injury) or total plexus injury. Erb’s palsy includes loss of deltoid, supraspinatus, infraspinatus, biceps, and brachialis function and presents with internal rotation, shoulder adduction, and elbow extension. Total plexus injury presents with a flail arm. Infraclavicular injuries involve the cords and their distal branches. They often present with focal weaknesses in shoulder abduction and flexion with or without deficits in elbow, wrist, or hand strength.
Preganglionic lesions can be differentiated from postganglionic lesions by weakness of the rhomboids, serratus, and supraspinatus in combination with an electrophysiologic profile of normal sensory conduction velocities with absent somatosensory evoked potentials. It may also be possible to see meningoceles on CT myelogram or MRI. However, preand postganglionic injuries may coexist and accurate diagnosis may not be possible until surgical exploration.
Goals of Reconstruction
Terzis and Papakonstantinou suggest the following priorities in reconstructing target muscles:
1.Return function to the supraspinatus and deltoid muscles to stabilize the shoulder and prevent severe neck pain.
2.Restore the biceps via the musculocutaneous nerve, allowing the hand to be brought to the face. Neurotization of the ipsilateral latissimus will also assist biceps function.
3.Attempt to reestablish triceps function.
4.Reconstruct the median nerve.
Brachial Plexus Injuries |
521 |
Surgical Strategies
Low velocity penetrating injuries should be explored immediately and repaired primarily or with nerve graft. Injuries related to gunshot wounds typically result from blast effect rather than by direct nerve injury; as such, spontaneous recovery may be possible. Surgery for closed injuries may be performed 3-6 months after injury, after any spontaneous recovery has been assessed and before irreversible muscle atrophy has occurred.
Neurolysis
The removal of scar tissue surrounding intact nerve fibers, known as neurolysis, may help nerve regeneration.
Nerve Repair and Grafting
When nerve continuity is interrupted distal to the sensory root ganglion, nerve repair or grafting may be beneficial. Primary repair may be attempted for simple nerve lacerations. Nerve grafts, often using the sural, antebrachial cutaneous, or radial sensory nerve, are used to reconstruct traction and crush injuries.
Neurotization
Preganglionic lesions may be treated with neurotization, in which functional nerves are harvested and transferred to distal nerve root stumps. Intraplexus donors, because of their large number of axons, provide the best motor donors for neurotization. Extraplexus motor donors, such as intercostal, phrenic, accessory, and medial pectoral nerves, may be used for multiple-root avulsions. The contralateral C7 nerve root,
combined with a nerve graft, may be also be used. Recently success has been reported 86 using branches of the ulnar nerve to neurotize the musculocutaneous nerve.
Nerve Root Repair and Reimplantation
There have been several recent reports of nerve root repair in which a nerve graft is inserted into the spinal cord and attached to the avulsed distal root. Some have also attempted to reimplant the avulsed root directly into the spinal cord. It is too early to know whether these methods will prove to be successful.
Secondary Procedures
Muscle and tendon transfers may be necessary to augment function. Concomitant release of muscle contractures that develop may be helpful in restoring balanced external rotation and abduction of the upper extremity. In refractory cases, functional free muscle transfer with the gracilis may be necessary to restore distal function.
Postoperative Care
After 2-4 weeks of splinting to prevent traction on the repair, an aggressive regimen of physical therapy, occupational therapy, and electric stimulation should be initiated. Induction exercises, which stimulate the donor nerves used during neurotization should be begun when recipient motor function begins to return. Patient expectations and compliance are paramount in achieving a successful long-term outcome. Secondary reconstruction with muscle transfers and contracture releases may be necessary. Patients in whom primary nerve reconstruction is performed should be counseled on the staged nature of reconstruction.
