
Practical Plastic Surgery
.pdf
Chapter 84
Wrist Fractures
Gil Kryger and Peter E. Hoepfner
Introduction
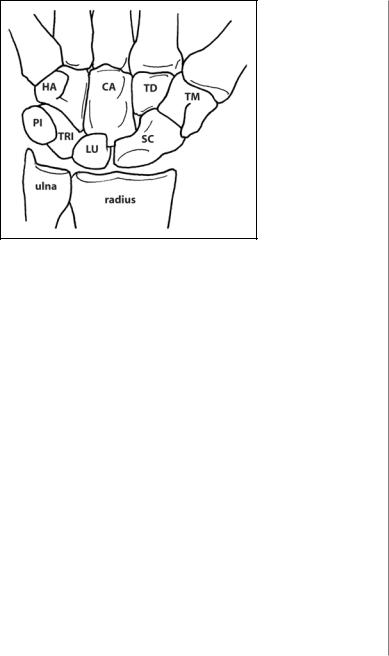
The wrist contains eight bones that are precisely arranged to provide maximum stability and mobility (Fig. 84.1). Although any of these bones can be fractured, the majority of injuries seen clinically and the most morbid injury is fracture of the scaphoid. Fractures of the trapezoid and lunate are extremely rare either as a frac- ture-dislocation injury or as an isolated injury. Fractures of the capitate are uncommon injuries and are usually in association with perilunate, trans-scaphoid, or trans-capitate fracture dislocations. The majority of this chapter will discuss scaphoid fractures and complications of nonunion.
Scaphoid Fractures
Epidemiology
The scaphoid bone (navicular bone) is the most commonly fractured carpal bone (80% of all carpal fractures). Patients, typically young, athletic, and active, fall on an outstretched arm, are injured in a motor vehicle accident, or are injured in sports. Roughly 400,000 fractures occur per year leading to significant morbidity and over 3.5 million days lost from work per year.
Anatomy
The scaphoid is a boat shaped bone with over 80% of its surface is covered by articular cartilage. It articulates with the radius and four of the remaining carpal bones. The scaphoid is the only carpal bone that spans the proximal and distal carpal rows; as such, it is involved in almost every movement of the wrist. It acts as an intercalary segment, connecting the proximal and distal carpal rows. The proximal and distal carpal rows can be thought of as two links in a chain: they are stable when pulled apart, but when compressed they will collapse. The scaphoid prevents this collapse during longitudinal compression of the wrist. However, if the scaphoid is broken (or heals with a fibrous nonunion) or if its ligamentous attachments are disrupted (scapholunate ligament tear), the carpus collapses. The blood supply is based on the superficial palmar branch (volar) and dorsal carpal branch (dorsal) of the radial artery. Both vessels enter the distal half of the scaphoid and supply the proximal pole via retrograde flow only. This retrograde flow is disrupted in proximal pole fractures, resulting in avascular necrosis of the proximal pole. The scapholunate ligament (dorsal), scaphocapitate ligament (palmar) and dorsal intercarpal ligaments are very important for stability. The ligaments also provide a vascular network that nourishes the scaphoid and should be preserved during surgery.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Wrist Fractures |
503 |
Figure 84.1. The carpal bones. HA, hamate. CA, capitate. TD, trapezoid. TM, trapezium. PI, pisiform. TRI, triquetrum. LU, lunate. SC, scaphoid.
Diagnosis |
|
A fracture of the scaphoid should be suspected in all patients complaining of |
|
84 |
|
radial sided pain after a fall, in particular pain over the anatomic snuffbox (dor- |
|
|
|
sally) or over the tubercle of the scaphoid volarly. Pertinent history includes the |
|
mechanism of injury, hand dominance, occupation, hobbies as well as a standard |
|
medical history. |
|
In addition to a thorough hand exam, it is important to examine for tender- |
|
ness of the snuffbox or scaphoid tubercle, pain with dorsiflexion, decreased grip |
|
strength, and dorsal swelling. |
|
Radiographic Examination |
|
The standard radiographs ordered include: AP, lateral, oblique, and PA of the |
|
wrist in ulnar deviation. |
|
If the initial X-ray is negative but the exam is suspicious, an occult fracture may |
|
be present that is not evident on the plain films. A low threshold for suspicion of an |
|
occult fracture is key to its diagnosis. The wrist should be immobilized in a |
|
below-the-elbow thumb spica cast, and the patient should be seen after two weeks. |
|
If the site is still tender after 2 weeks, repeat X-rays should be obtained (95% sensi- |
|
tivity for repeat films). If repeat films are negative, but the patient is still tender, a |
|
bone scan is ordered. Recent data supports the use of CT and MRI in these cases as |
|
well. Patients with established nonunions of the scaphoid may present after an acute |
|
injury that aggravates the old injury. It is imperative to distinguish between an acute |
|
scaphoid fracture and a newly injured nonunion as the treatments are completely |
|
different. Nonunions typically have sclerotic edges at the fracture site whereas acute |
|
fractures will not. |
|
Fracture Classification |
|
Fractures can be categorized as stable or unstable. |
|
Stable fractures may be managed conservatively or with surgery (see below). |
|
Fractures that have not healed after four months of adequate treatment may be |
|
504 |
Practical Plastic Surgery |
84
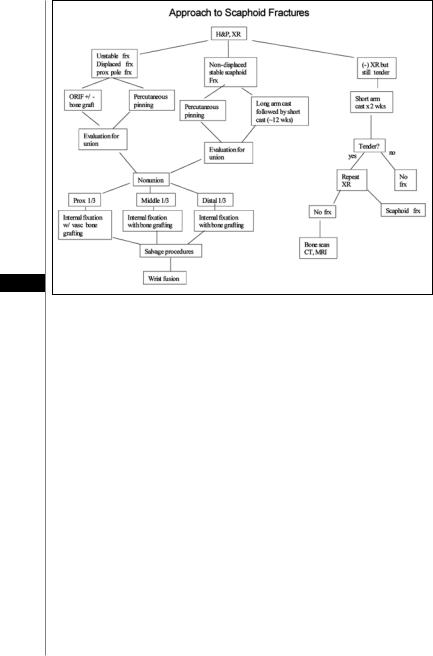
Figure 84.2. Algorithm for the management of scaphoid injuries.
classified as delayed unions with potential to heal if properly immobilized. Delayed unions demonstrate no sclerotic changes at the fracture site (in the presence of fracture widening and cystic changes in adjacent bone). If sclerotic changes are seen radiographically at the fracture site, the diagnosis of nonunion is made.
Unstable fractures are those that have a step-off of greater than or equal to 1 mm, any angulation, motion at the fracture site, or carpal instability. These fractures will progress to nonunion if untreated and always require surgical intervention.
Treatment
An algorithmic approach to the treatment of scaphoid fractures is shown in Figure 84.2.
Acute stable fractures: Historically, these patients were treated conservatively by immobilization for a total of 12 weeks (6 weeks in an above elbow thumb spica cast, followed by a below elbow thumb spica cast for the remaining 6 weeks). Recent studies have demonstrated that percutaneous screw fixation of acute stable scaphoid fractures should be offered to all patients that are surgical candidates. These patients return to work earlier, have earlier bony union, and have less wrist stiffness.
Displaced/unstable fractures: These are generally treated with open reduction and internal fixation. Rarely, some of these fractures may be amenable to percutaneous pinning and closed reduction to minimize soft tissue and blood supply disruption.
Proximal one-third fractures: These fractures always require surgery and should not be immobilized because of the high risk (16-42%) of nonunion and avascular necrosis.

Wrist Fractures |
505 |
Operative Considerations |
|
The patient is placed supine with a well-padded tourniquet on the upper arm. |
|
Regional anesthesia (brachial plexus block) is preferred. Preoperative IV antibiotics |
|
are given. A fluoroscan and power driver are generally required. |
|
Percutaneous screw fixation: A volar approach is used for all fractures except |
|
proximal pole fractures (because of the likelihood of missing a small proximal frag- |
|
ment from the volar side). A percutaneous pin is driven through the long axis of the |
|
scaphoid. This pin acts as a guide for a canulated screw that will span the fracture |
|
and provide compression and rigidity. Commonly used screws are the Accutrack, |
|
AO screw and the Herbert-Fisher cannulated screw. A second parallel pin prevents |
|
rotation while drilling the bone. |
|
Open reduction internal fixation (ORIF): A volar approach is preferred. The |
|
surgeon should avoid stripping the bone of its ligaments as this will adversely affect |
|
blood flow and healing. Accurate reduction is obtained using a custom jig or by |
|
using pins to “joystick” the fragments into alignment. A compression screw provides |
|
rigid fixation and compression. |
|
Bone grafting: In cases of malunion (or severe comminution), the fibrous scar is |
|
removed with curettes back to healthy bleeding bone resulting in a bone gap. Bone |
|
graft can be obtained from the iliac crest or distal radius. A screw with or without |
|
K-wire crosses the fracture and graft. |
|
Postoperative Management |
84 |
Immobilize the wrist in cast or splint (below the elbow) for 2-6 weeks (although some surgeons begin early range of motion immediately after surgery). Strengthening exercises begin roughly 3 weeks after surgery. Radiographs are obtained every 4 weeks until complete union is seen. There is new data that supports the use of adjuvant modalities to accelerate healing. External ultrasound and electromagnetic stimuli have been shown to decrease time to union and may be used in the postoperative period as well as during immobilization when surgery is not needed.
Scaphoid Nonunion
Nonunion occurs in 5-12% of all scaphoid fractures. Distal pole fractures almost always heal (nearly 100% union rate), middle one-third fractures have an 80-90% union rate, while proximal pole fractures have up to a 40% nonunion rate. Motion at the fracture prevents bony union, resulting in a fibrous pseudarthrosis at the fracture site. The highest risk of nonunion is in missed fractures, more proximal fractures, fractures associated with ligamentous injury, and displaced or comminuted fractures. Nonunion invariably results in osteoarthritis and instability of the wrist if not treated properly.
Classification
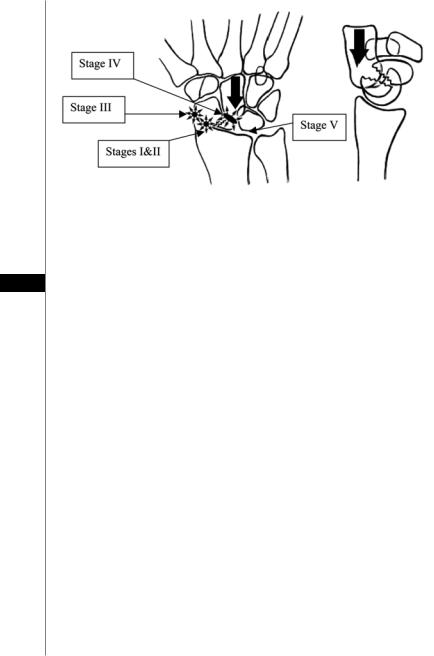
Stable nonunions are termed Stage I. They have a tough fibrous scar that prevents motion across the old fracture line. No degenerative changes are seen, but these will progress to unstable nonunions if not treated.
Unstable nonunions are characterized by motion across the old fracture site and associated arthritis. They are classified as Stages II-V. Stage II scaphoid nonunions have some degree of carpal collapse, but little or no arthritis. As the carpus collapses, the distal carpal row, namely the capitate, migrates proximally into the gap between the scaphoid fragments. The distal scaphoid fracture fragment may be displaced against the radial styloid (Stage III) causing radiostyloid
506 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 84.3. Scaphoid nonunion advanced collapse (SNAC): proximal migration (collapse) of the capitate into the gap between the scaphoid fragments displaces the fragments against adjacent bones resulting in arthritis. SLAC wrist is similar; however the capitate migrates proximally into the gap between the scaphoid and lunate.
84arthritis. Additional collapse disrupts the midcarpal joint and the capitate rubs against the proximal fracture fragment and the radius resulting in midcarpal and radioscaphoid arthritis (Stage IV). Eventually, the distal row (mainly the capitate) pushes the lunate proximally against radius resulting in radiolunate and generalized arthritis (Stage V). Stages IV and V are termed scaphoid nonunion advanced collapse (SNAC, Fig. 84.3).
Treatment of Scaphoid Nonunion
The goal of treatment is to heal the nonunion, stabilize the carpus, and correct carpal collapse, thus relieving symptoms. After debridement of the fibrous scar, bone grafting is always required. The graft can be planned preoperatively to replace specific size and angular deformities. Wedge grafts can be placed on the volar side to correct a “humpback” deformity. Vascularized bone grafts are indicated for all proximal one-third nonunions, avascular necrosis of the scaphoid, as well as for failed nonvascularized bone graft attempts. The graft is generally based on small branches off the radial artery. Most widely used is the 1-2 intercompartmental supraretinacular artery graft (Zaidemburg Graft).
Salvage Procedures
Despite our best efforts to diagnose and fix scaphoid fractures, there will often be injuries that are missed or do not heal properly. The final common pathway of these types of injuries is degenerative arthritis of the wrist. In cases of generalized arthritis and pain, the goal is to achieve a pain-free functional wrist (with 40˚ of flexion and 40˚ of extension).
Starting with conservative approaches, the physician should counsel the patient to avoid overstraining the wrist and provide him with a wrist support. As the main patient complaint is pain, anterior and posterior neurectomies can be performed to reduce pain. Transection of the anterior and posterior interosseus nerves reduces pain and should be done when performing any other salvage procedure. Excision of

Wrist Fractures |
507 |
the radial styloid or of any osteophyte can reduce pain by relieving impingement of the fragment on adjacent bone. The excised fragment can be used as a bone graft. Partial scaphoid excision is removal of the proximal or distal fragment without destabilizing the scapholunate ligament distally.
More complex procedures may be necessary, including scaphoid excision with four-corner fusion of the capitate, lunate, triquetrum and hamate to treat arthritis. Proximal row carpectomy involves excision of the proximal row allowing the capitate to sit in the lunate fossa of the radius. Studies have shown that the results are similar for both procedures with a proximal row carpectomy avoiding the lengthy immobilization required by four-corner fusion. The final salvage procedure for wrist arthritis is total wrist fusion.
Hamate Fractures
Fractures of the body are less common and are associated with fractures of the base of the ulnar metacarpals to form the ulnar component of axial instability patterns and should be treated as such. Nondisplaced isolated fractures can be treated with immobilization.
Hook fractures commonly occur in individuals holding golf clubs, bats or hammers. Patients complain of a dull ache when gripping. Inflammation and displacement can affect the ulnar nerve (paresthesias) or flexor tendons to the ring and small fingers (pain with flexion). Diagnosis is often delayed, but can be made with carpal tunnel views of plain films or CT and bone scans. 84
Acute nondisplaced hook fractures can be immobilized for 6 weeks. Displaced fractures and those that are diagnosed 1-2 months after the initial trauma are best treated with excision of the fracture fragment. Some surgeons advocate stabilization with a 1.5 mm cortical screw. After excision, mobilization is started after 1-2 weeks. With internal fixation, the hand is splinted for 6 weeks with a removable brace.
Triquetrum Fractures
These common fractures often occur in association with other wrist fractures as a result of a fall on an outstretched hand. Most commonly, a dorsal cortex chip is seen on lateral view. These fractures can usually be treated symptomatically. Less common are body fractures which are usually nondisplaced (and missed on x-ray); treatment is 4-6 weeks of immobilization. Large displaced fragments and those that involve the articulating surface require ORIF followed by 4-6 weeks of casting.
Lunate Fractures
These fractures are rare and may be a manifestation of Kienböck’s disease. Treatment of nondisplaced fractures is by cast immobilization (below the elbow thumb spica) for 4-6 weeks. Displaced fractures may require ORIF.
Trapezium Fractures
These rare fractures occur as a result of compression of the trapezium between the radial styloid and thumb metacarpal. Plain films including a carpal tunnel view and oblique view will visualize the fracture; however some authors believe that CT is a better modality to define the injury and the concomitant thumb metacarpal injury. Unstable fractures, or those with 1 mm or more of depression, should be treated with ORIF (often with bone graft). Postoperative immobilization for 4-6 weeks is recommended.

508 |
Practical Plastic Surgery |
Trapezoid Fractures
The least injured carpal bone, fractures of the trapezoid occur as a result of volar forces applied to the index metacarpal to cause dorsal dislocation of the bone. Acute fractures require anatomic reduction and stabilization. If closed reduction is successful, 4-6 weeks of casting (below the elbow thumb spica), or until the fracture is nontender, is needed.
Capitate Fractures
Isolated fractures are rare. Most fractures involve the proximal two-thirds of the bone as part of a perilunate injury. Nondisplaced fractures are immobilized but rotated fragments require ORIF. Diagnosis is by CT.
Pisiform Fractures
Fractures are rare and are treated with immobilization. Nonunions are treated by excision.
Wrist Instabilities
Injuries to the ligaments of the carpus are common and occur alone or in conjunction with the abovementioned fractures. It is important to understand the biomechanics of the wrist to fully understand these injuries, their natural history and treatment. A full discussion of this should be sought in a hand surgery text-
84book. Briefly, the wrist joint can be thought of as three joints: radiocarpal, midcarpal and carpometacarpal. These three joints flex and extend in unison to allow a full range of flexion and extension motions. Additionally, the carpal bones translate during radial and ulnar deviation. With deviation of the wrist towards the radius, the proximal bones (scaphoid, lunate and triquetrum) tend to flex volarly. With ulnar deviation, the scaphoid is extended and is better visualized on AP and PA views.
Diagnosis
As with all ligamentous injuries, the timing of diagnosis and repair is paramount. Acute injuries (<1 week) have maximum healing potential; subacute injuries (1-6 weeks) have decreased healing potential but do not demonstrate fixed deformities or arthrosis; chronic injuries (>6 weeks) usually display fixed deformities and therefore require surgical repair and reconstruction. The key is to diagnose these injuries early to maximize healing without surgery.
Classification
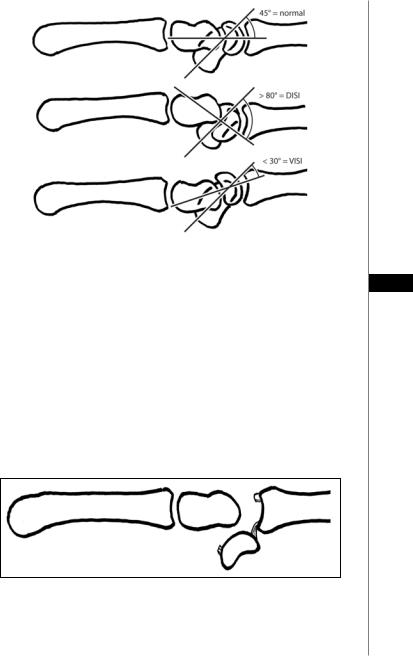
It is useful to categorize these injury patterns based on their radiological appearance (Fig. 84.4). On lateral view, the radius, lunate and capitate are linear while the scaphoid is flexed 45˚ volarly relative to the lunate. When the lunate is angled dorsally, the term dorsal intercalated segmental instability (DISI) is used. Because there is dissociation between the scaphoid and lunate (scapholunate ligament tear), the scaphoid is flexed beyond 80˚ in relation to the lunate.
Much less frequently, the lunate is angled volarly, and the term becomes volar intercalated segmental instability (VISI). The lunate is flexed in the same direction as the scaphoid, and the angle between them decreases to about 30˚. This orientation indicated injury to the LT ligament.
Wrist Fractures |
509 |
|
|
|
|
|
|
|
Figure 84.4. Wrist instability. Shown are the dorsal intercalated segmental insta-
bility (DISI) and the volar intercalated segmental instability (VISI) deformities.
84
Dorsal Intercalated Segmental Instability
The most common cause of the DISI deformity is a disruption of the scapholunate ligament (S-L). This injury should always be suspected in a radial styloid fracture. In advanced stages, the scaphoid is hyperflexed and the term rotatory subluxation of the scaphoid is also used. Mayfield and colleagues demonstrated that there is a predictable pattern of injuries as the S-L is torn, followed by a sequence of tearing of ligaments around the lunate until the carpus is dislocated; this progression correlates with the amount of energy causing the injury. The final stage of carpal dislocation is the volar dislocation of the lunate as the capitate is driven into the radiocarpal joint. Since the lunate is still attached to the radius by its volar ligaments, the lunate dislocates volarly, resting perpendicular to the radius on lateral view. This is often termed the “spilled teacup sign,” and is shown in Figure 84.5.
Figure 84.5. The “spilled teacup sign.” Disruption of the scapholunate ligament can lead to volar dislocation of the lunate as the capitate is driven into the radiocarpal joint. Since the lunate is still attached to the radius by its volar ligaments, the lunate dislocates volarly, resting perpendicular to the radius on lateral view.

510 |
Practical Plastic Surgery |
Diagnosis
Diagnosis is based on pain and tenderness in the snuffbox and over the S-L dorsally, associated with clicking sounds with motion. The Watson scaphoid shift test can be diagnostic. The examiner places his thumb over the scaphoid tubercle volarly, while passively deviating the wrist from ulnar to radial. The scaphoid attempts to flex volarly but is blocked by the examiner’s thumb; because the S-L is disrupted, the proximal pole of the scaphoid rides up over the dorsal lip of the radius and the thumb is removed, and the scaphoid clunks back into the radioscaphoid joint and pain is elicited. The exam and radiographs should always be compared with the contralateral uninjured wrist. On scaphoid views, the scapholunate interval is >2 mm (Terry Thomas sign). As the scaphoid flexes more volarly, it can be seen on stress PA views on end (perpendicular to the radius); the distal pole overlying the proximal pole creates the “scaphoid ring sign”.
Treatment
In acute and subacute settings, without rotatory subluxation of the scaphoid, treatment consists of arthroscopic debridement of the torn ligaments and stabilization of the carpus with K-wires, followed by immobilization in a below-elbow thumb spica for 4-6 weeks. Recently, direct repair of the S-L ligament with dorsal capsulodesis for augmentation has been advocated. In advanced cases termed scapholunate advanced collapse (SLAC), the carpus collapses in a regular pattern. Arthritis begins between the
84scaphoid and radial styloid and progresses to the entire radioscaphoid and capitolunate joints. As in SNAC wrist, the radiolunate joint is spared except in severe cases.
Volar Intercalated Segmental Instability
VISI deformities are much less common than DISI deformities. The most common cause of the VISI deformity is lunotriquetral (L-T) dissociation. These injuries are diagnosed by ulnar sided pain with limited range of motion in association with clunk. The provocative test is the shear test. In this test, the examiner pushes the lunate volarly and the pisiform (and triquetrum) dorsally causing a shearing force at the L-T joint. Pain is considered a positive test.
Treatment
Management of L-T injuries without frank VISI deformity is by immobilization alone. Even chronic complete tears of the L-T ligament can heal with immobilization. For more severe injuries, and those with carpal collapse, limited fusion of the wrist is indicated.
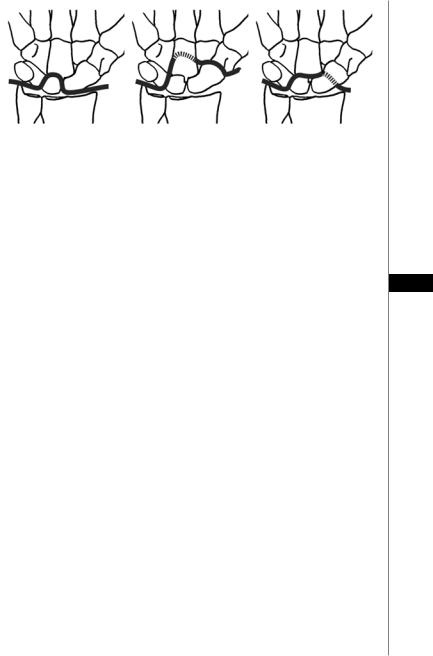
Combined Fracture-Dislocations
Extremely high energy injuries can result in carpal fracture-dislocations. The pattern of injury depends on its path across the carpus: disruption of the S-L, fracture of the scaphoid or fracture of the scaphoid and capitate. Displacement of the carpal bones can compress the neurovascular structures in the wrist resulting in acute carpal tunnel syndromes. Immediate reduction in the emergency room should be attempted, with later operative fixation. Irreducible dislocations should be taken to OR for reduction. Patterns of perilunate fracture-dislocation are shown in Figure 84.6.
Pearls and Pitfalls
•Acute, nondisplaced, nonangulated scaphoid fractures can be treated with an above-elbow thumb spica cast for at least three weeks, followed by an additional period in a below-elbow thumb spica cast with the wrist in mild radial deviation
Wrist Fractures |
511 |
|
|
|
|
|
|
|
Figure 84.6. Perilunate fracture-dislocation patterns: perilunate injury with disrup- |
|
tion of the S-L ligament (left), perilunate injury with fracture of the capitate (center), |
|
and perilunate injury with fracture of the scaphoid (right). |
|
and palmar flexion. However, many patients, especially those who are young |
|
and active, will not agree to lengthy casting protocol. In such cases rigid fixation |
|
is required (as described above). |
|
• Pulsed electromagnetic field therapy (PEMF) has been used to help stimulate |
|
healing in scaphoid nonunions. At the present, it is not widely used; however it |
|
should be considered in cases in which surgery is not an option since it does have |
84 |
a low risk profile. |
•Proximal row carpectomy is an acceptable treatment for scaphoid nonunion. It can be considered even in young active patients, and long-term results have been superior to intercarpal fusion. Excision of the terminal branch of the posterior interosseous nerve during carpectomy may help reduce some of the postoperative pain.
•Hook of the hamate fractures occur in athletes gripping a club, most commonly in golfers. They can be difficult to diagnose. Pain is in the ulnar wrist and worsened by gripping and with little finger flexion against resistance with ulnar deviation of the wrist. If left untreated, they have a high risk of nonunion.
•Capitate fractures are difficult to diagnose by plain radiograph, and a CT scan is often required. The neck of the capitate can fracture in association with a scaphoid waist fracture, termed scaphocapitate syndrome. If missed, the head of the capitate can develop avascular necrosis. This injury should be suspected in a fall on an outstretched hand with the wrist in extension or from a blow to the dorsum during wrist flexion.
•Triquetrum fractures should be suspected in a fall on an outstretched hand combined with a twisting motion of the wrist. These fractures usually do not require surgery and have a low complication rate.
Suggested Reading
1.Blatt G. Scapholunate Instability. In: Lichtman DM, ed. The wrist and its disorders. Philadelphia: WB Saunders Co., 1988.
2.Bond CD, Shin AY, McBride MT et al. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am 2001; 83A(4):483.
3.Gellman H, Caputo RJ, Carter V et al. Comparison of short and long thumb-spica casts for nondisplaced fractures of the carpal scaphoid. J Bone Joint Surg Am 1989; 71(3):354.
4.Mayfield JK. Mechanism of carpal injuries. Clin Orthop Relat Res 1980; 149:45.
5.Trumble TE, ed. Principles of Hand Surgery and Therapy. Philadelphia: WB Saunders Co., 2000.
6.Zaidemberg C, Siebert JW, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg [Am] 1991; 16(3):474.
