
Practical Plastic Surgery
.pdf
472 |
Practical Plastic Surgery |
78
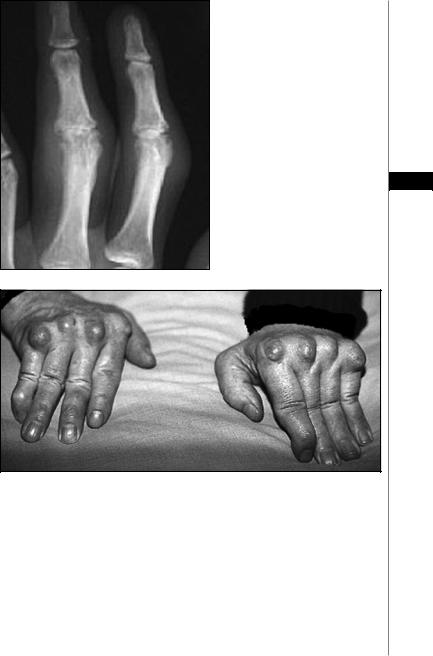
Figure 78.9. Fracture of the hamate bone. Hook fractures commonly occur in golfers, baseball players or construc-
Figure 78.8. Fifth metacarpal fracture, tion workers with a complaint of a dull commonly known as a boxer’s fracture. ache when gripping.
Figure 78.10. Fracture of the distal phalanx, or a mallet fracture. Distal phalanx fractures can occur due to avulsion of a bony fragment attached to the flexor or extensor tendon.

Radiographic Findings |
473 |
78
A B
Figure 78.11. Dislocation of the lunate bone in the P-A (A) and lateral views (B). Note the normal position of the capitate bone with respect to the distal radius. In milder cases, the lunate can sublux dorsally after scapholunate ligament disruption (DISI) and will rarely sublux volarly after lunotriquetral ligament disruption (VISI).
Figure 78.12. Triquetrum fracture. Usually associated with other wrist fractures after a fall on an outstretched arm. This fracture is usually a dorsal cortex chip fracture best seen on a lateral view.

474 |
Practical Plastic Surgery |
Figure 78.13. Avulsion fracture of the ulnar collateral ligament insertion at the base of the thumb, commonly referred to as a gamekeeper’s or skier’s thumb. If the fragment is widely displaced, a Stener lesion can result, requiring surgical intervention.
78 |
|
|
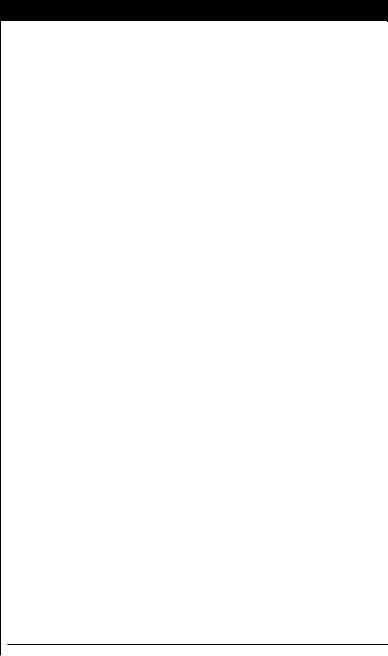
Figure 78.14. Rheumatoid |
|
|
||
|
|
|
arthritis of the wrist, demon- |
|
|
|
strating bony ankylosis of |
|
|
|
the carpus, ulnar deviation |
|
|
|
at the MP joints, and ulnar |
|
|
|
styloid erosions. |
|
|
|
|
Figure 78.15. Late rheumatoid arthritis. There is marked MP joint destruction and narrowing. Weakening of the radial sagittal bands causes ulnar subluxation of the extensor mechanism and subsequent ulnar deviation of the MP joints.
Radiographic Findings |
475 |
Figure 78.16. Rheumatoid arthritis in the fingers. In contrast to osteoarthritis, the IP joints are narrowed with characteristic erosions.
78
Figure 78.17. An illustration of several of the common clinical features of rheumatoid arthritis: symmetrical joint involvement, rheumatoid nodules, ulnar deviation of the MP joints, and swan neck deformity of the digits (IP hyperextension and DIP flexion).
Chapter 79
Examination of the Hand and Wrist
Zol B. Kryger
Observation
The hand should be observed in the resting position. This is termed the position of function. The wrist will be slightly dorsiflexed, the MP joints will be in 45-75˚ of flexion, the PIP joints in about 10˚ of flexion, and the DIP joints will be in 0-10˚ of flexion. Any alterations in the normal resting position should be noted. A single finger fixed in extension can be due to a flexor tendon laceration or rupture. A single finger in fixed flexion may be due to an extensor tendon injury. If the abnormal flexion is chronic, flexor tendon contracture must also be considered. This can be seen in Dupuytren’s disease.
The patient should be instructed to slowly make a fist by flexing the fingers towards the palm. The fingertips should point towards the scaphoid. A finger fracture with rotational deformity can result in one finger overlapping another, or an alteration in the axis of convergence.
Sensory Exam
The hand receives sensory innervation from the median, ulnar and radial nerves. The most reliable method of testing normal sensory discrimination is the two-point discrimination test. The minimal distance at which the patient can distinguish two distinct points of pressure is recorded. Two-point discrimination should be 2-3 mm on the pulp of the fingers. This value can vary based on the individual’s occupation. A measurement of greater than 5 mm is abnormal in most people.
To test median nerve sensation, skin sensibility on the palmer surface of the first three digits should be evaluated. Ulnar nerve injury will result in abnormal sensation of the little finger and ulnar side of the ring finger. Loss of radial nerve sensation will result in loss of sensibility on the dorsum of the hand and in the first web space. In addition, any areas of numbness, tingling or other sensory abnormalities reported by the patient should be noted as this can provide clues as to the nerve that may be involved.
Evaluation of Motor Nerve Function
The most consistent sign of median nerve injury is loss of thenar opponens function. Patients will make a fist without the thumb and index finger folded into the palm. If the flexor pollicus longus (FPL), flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) of the index and middle finger are flexing normally, then the nerve injury has occurred distal to the take off of the anterior interosseous nerve.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

Examination of the Hand and Wrist |
477 |
Signs of ulnar nerve injury include flexor carpi ulnaris (FCU) paralysis, interosseous and thumb adduction loss with a weak “key pinch,” and FDP paralysis of the small and ring fingers. A long-standing injury can present with the classic “claw hand” deformity. In a low lesion of the ulnar nerve just above the wrist, there will be more clawing of the 4th and 5th fingers compared to a high lesion at the elbow. This is known as ulnar paradox and is due to the fact that in a high lesion the flexors will also be paralyzed.
Patients with a radial nerve injury will be unable to extend their wrist or fingers. This can occur following humeral shaft fractures. Injury to the radial nerve in the axilla will result in paralysis of the extensor carpi radialis longus (ECRL) and brevis (ECRB), triceps and brachioradialis muscles. These muscles will atrophy in long-standing nerve injury. Loss of ECRL and ECRB function leads to loss of wrist extension.
Muscle power is assessed on a scale of 0-5, with a score of 5 indicating full power
and a score of 0 being paralysis. 1 is given for just a flicker of muscle contraction, 2 79 for the ability to move with gravity eliminated, and 3 is the muscle strength neces-
sary to lift a joint against the force of gravity. A score of 4 is for muscle power between 3 and 5.
Flexor Tendon Evaluation
Separate evaluation of both FDP and FDS function is important. Division of the FDS without injury to the FDP will not be noticeable in the resting posture. The FDS is evaluated by immobilizing the surrounding fingers in extension and having the patient flex the finger at the PIP joint. FDS to the index finger is evaluated by having the patient perform a firm pulp-to-pulp pinch with the thumb. An injured FDS will cause pseudo mallet deformity of the distal phalanx (flexed DIP, extended PIP), whereas an intact FDS will result in a pseudo boutonniere deformity of the distal phalanx (extended DIP, flexed PIP). FDP is evaluated by immobilizing the PIP and IP joints and evaluating flexion of the isolated DIP joint.
The palmaris longus is present in 85-90% of patients. It courses over the hamate and is identified by having the patient forcibly oppose the thumb and little finger. This tendon is expendable and can be readily used for tendon grafting procedures.
Extensor Tendon Evaluation
Extension of each individual digit at each joint should be examined. It is important to remember that the juncturae tendinum located at the level of the MP joints connects the extensor tendons of extensor digitorum communis (EDC). Therefore, lacerations proximal to the juncturae may not impair digit extension due to the connection to the adjacent digits. Limitation of extension of the DIP joint of the finger is most often due to rupture of the insertion of the extensor tendon into the distal phalanx. This type of injury will produce a mallet finger deformity. If the extensor tendon is disrupted proximal to the PIP joint, a boutonniere deformity may be produced due to hyperextension of the DIP joint by the taught lateral slips.
Evaluation of extensor pollicus longus (EPL) function is performed by asking the patient to place his palm flat on the table and to raise the thumb off of the table. Extension of the thumb alone is not an adequate test of EPL function since extensor pollicus brevis (EPB) and the intrinsic muscles of the thumb will contribute to its extension.

478 |
Practical Plastic Surgery |
Intrinsic Hand Muscle Evaluation
The dorsal interossei are tested by asking the patient to abduct the fingers away from the middle finger, whereas the volar interossei are evaluated by adduction of the fingers towards to the middle finger. The lumbricals are tested by asking the patient to flex the fingers at the MP joints while the IP joints are held in extension.
Thumb Laxity
Instability of the MP joint of the thumb should be assessed. Laxity should be determined by abducting the thumb in both extension and flexion. Thumb laxity is normally greater in extension and should be compared between the two hands. Rupture of the ulnar collateral ligament (UCL) that connects the proximal phalanx of the thumb to the first metacarpal will result in excessive MP laxity. This injury is commonly seen in skiers, skateboarders, and anyone who falls on an extended thumb that is forcefully abducted. The acute injury is termed skier’s thumb, and the chronic
79 injury is referred to as gamekeeper’s thumb.
Vascular Exam
The color of the digits should be observed, and any pallor, hyperemia or cyanosis noted. Capillary refill greater than 2 seconds is not normal. Arterial inflow to the hand is determined by palpating the radial and ulnar artery pulses. The Allen test is performed using the thumb and fingers to compress the radial and ulnar arteries at the wrist. The patient exsanguinates the hand by making a fist several times and then opens the hand so that the fingers are in a relaxed and gently extended position. The examiner then releases pressure from over the ulnar artery. Capillary refill time in the hand is noted. A normal Allen test is refill in less than 5 seconds, and greater than 5 seconds indicates an abnormal Allen test.
Wrist Stability and Motion
Pronation and supination of the wrist are examined with the elbow flexed to 90° and held firmly to the sides in order to stop rotation of the shoulder. From this position, there is usually about 90° of pronation and 90° of supination. Flexion, extension, radial and ulnar deviation should all be compared between the two wrists simultaneously, and any discrepancies should be noted.
Volar and dorsal stability are determined by the examiner exerting axial traction while holding the patient’s forearm with one hand and the metacarpal heads with the other. Volar and dorsal displacement of the wrist in this position is minimal. If wrist laxity is present during volar pressure, midcarpal subluxation may be due to a flexion deformity of the first carpal row (the VISI deformity). If laxity is noted during dorsal pressure, a dorsal deformity (the DISI deformity) may be present.
Bony Landmarks
Patients will often present with focal pain in the hand or wrist. An understanding of the bony landmarks can help identify the structure that may be injured.
Volar Surface
The pisiform is located on the ulnar side of the palm just proximal to the palmar crease. Tenderness at the bony prominence should be assessed. The hook of hamate is 1-2 fingerbreadths towards the midline from the pisiform. The examiner places his thumb IP joint over the pisiform and directs his thumb towards the patient’s

Examination of the Hand and Wrist |
479 |
index finger. The thumb pulp will rest over the hamate. The hook becomes more prominent with wrist flexion.
Dorsal Surface
The anatomic snuff box is located on the radial side of the wrist. Its radial border is EPB and abductor pollicus longus (APL; first dorsal compartment). The ulnar border is EPL (third dorsal compartment). This structure is important because the most commonly fractured carpal bone, the scaphoid, lies below the snuff box. The distal pole of the scaphoid can be palpated in the snuff box with the wrist in ulnar deviation. The scapholunate (SL) joint is the most common site of carpal dislocation. The examiner traces the third metacarpal proximally towards the wrist. The examiner’s finger falls into a depression overlying the SL joint. The lunate is the second most commonly fractured carpal bone. It lies just ulnar to the SL joint. It is palpated with the wrist in flexion during which it is the most prominent area on the dorsum of the wrist. Lister’s tubercle is an easily palpable prominence at the distal
radius that lines up with the third metacarpal. It is easier to palpate it during mild 79 wrist flexion. Recall that it separates the second and third compartments.
Important Provocative tests
Tinel’s sign is a useful test for neuropathy. If percussion at the site of nerve entrapment produces tingling along the course of the nerve or in the digits supplied by the nerve, the test is positive. At the wrist, the volar carpal ligament can be percussed to test for median nerve neuropathy (carpal tunnel syndrome). The test has a low sensitivity (50-70%), but a high specificity (94%).
Phalen’s test is used to provoke median nerve compression. It is performed by having the patient hold both wrists in flexion for a minute by opposing the dorsum of the two hands. If this reproduces the symptoms, the test is positive. It has a sensitivity of 70-80% and a specificity of 80%. The more rapidly the symptoms are produced, the higher the specificity of the test.
Finkelstein’s test is used to test for tenosynovitis of the first dorsal extensor compartment (de Quervain’s disease). The wrist is braced in ulnar deviation while the thumb is passively adducted and flexed. A positive test produces pain at the base of thumb. There may also be point tenderness over the radial styloid.
The grind test is used to assess for arthritis of the carpometacarpal (CMC) joint of the thumb, a common condition that produces pain similar to de Quervain’s tenosynovitis. The examiner exerts axial pressure on the thumb and grinds it against the first metacarpal against the trapezium. A positive test produces pain. In addition, plain radiographs will show arthritic changes—a finding that will be absent in de Quervain’s disease.
The scaphoid shift, or Watson test, is used to test for SL instability or scaphoid fracture, although it has a low sensitivity and specificity. The examiner’s fingers are placed dorsally on the distal radius, while the thumb is placed firmly on the scaphoid tubercle (on the volar surface). The other hand holds the metacarpals, and the wrist is deviated ulnarly which places the scaphoid in extension. As the wrist is moved in radial deviation, the scaphoid is blocked from flexing by the examiner’s thumb. If the SL ligament is injured, the scaphoid will move dorsally under the posterior margin of the radius inducing pain when it touches the examiners fingers. When pressure on the scaphoid is removed, the scaphoid goes back into position with a thunk or clunk. The test should be performed on the uninjured wrist for comparison.

480 |
Practical Plastic Surgery |
The screwdriver test is used to examine the triangular fibrocartilage complex (TFCC). The examiner shakes the patient’s hand and performs alternating supination and pronation of the wrist (i.e., screwing and unscrewing motion). This motion will usually cause ulnar-sided pain at the wrist if a TFCC injury is present. Decreased range of motion may also be apparent.
Pearls and Pitfalls
–Any patient with an acute injury should be asked the following questions:
•When did the injury occur?
•What was the mechanism of injury?
•What was the position of the hand and/or fingers during the injury?
•Was the environment clean or dirty?
•Have any medications been administered by the ER staff such as a local anesthetic?
•Is there a history of prior injury?
•What is the tetanus status?
79– Palpation for specific tender spots is often the most painful part of the physical assessment and should therefore be reserved for the end of the exam.
–A patient complaining of chronic hand or wrist pain should be asked to demonstrate the movements that most accurately replicate the pain.
–In order to avoid missing an important finding on the initial physical exam, it is useful to follow an examination routine such as:
•Observation
•Vascular: Radial and ulnar artery, capillary refill, skin color
•Sensory: Median, ulnar and radial nerves
•Motor: Median, ulnar and radial nerves
•Flexor tendons
•Extensor tendons
•Intrinsic hand muscles
•Wrist stability and range of motion
•Palpation of bony landmarks
•Provocative tests
Suggested Reading
1.Corley Jr FG. Examination and assessment of injuries and problems affecting the elbow, wrist, and hand. Emerg Med Clin North Am 1984; 2(2):295-312.
2.Daniels IInd JM, Zook EG, Lynch JM. Hand and wrist injuries: Part I. Nonemergent evaluation. Am Fam Physician 2004; 69(8):1941-8.
3.Daniels IInd JM, Zook EG, Lynch JM. Hand and wrist injuries: Part II. Emergent evaluation. Am Fam Physician 2004; 69(8):1949-56.
4.Kuschner SH, Ebramzadeh E, Johnson D et al. Tinel’s sign and Phalen’s test in carpal tunnel syndrome. Orthopedics 1992; 15:1297-1302.
5.Skvarilova B, Plevkova A. Ranges of joint motion of the adult hand. Acta Chir Plast 1996; 38(2):67-71.
6.Waylett-Rendall J. Sensibility evaluation and rehabilitation. Orthop Clin North Am 1988; 19(1):43-56.

Chapter 80
Soft Tissue Infections
Zol B. Kryger and Hongshik Han
Introduction
Infections of the hand can range from minor, superficial cases to infections of the deeper spaces of the hand that can potentially become limb-threatening and must be treated aggressively. Trauma is the major cause of hand infections, followed by human bites and animal bites. Staphylococcus aureus (S. aureus) accounts for about two-thirds of all hand infections.
Clinical Presentation
Diagnosis
A thorough history is important. The exact time and nature of the injury should be ascertained since this will guide treatment. For example, S. aureus is often implicated in home and industrial infections, whereas Gram-negative bacteria should also be considered if the infection occurred on a farm setting. Determination of hand position during and after the injury is also important. Accompanying symptoms help determine how extensive the infection has become. The age of the patient is important as well. Hand infections in children may involve different bacteria such as oral flora and Gram-negative rods (e.g., H. Influenza or pseudomonas). Table 80.1 lists the common hand infections and antibiotics used to treat them.
Differential Diagnosis
There are a number of conditions that can simulate a hand infection: acute calcific tendinitis (usually affecting flexor carpi ulnaris), gout or pseudogout, pyogenic granuloma, pyoderma gangrenosum, metastatic cancer, and the necrosis from the brown recluse spider bite, to name a few. Radiographs are required in all suspected hand infections to rule out gas in the soft tissue and occult fracture or osteomyelitis.
The early hand infection may masquerade as ischemia. Findings on exam might include areas of patchy discoloration, edema, slow capillary refill and a mottled, cyanotic appearance. Gross purulence and inflammation may not be observed. Late infections developing 7-10 days after the initial injury indicates an insufficient local host response against bacterial contamination. The wound usually becomes fluctulant with purulent discharge. Late infections are seen more commonly in diabetics or immunocompromised individuals (e.g., transplant recipients, chemotherapy recipients, HIV, and other immune disorders).
Treatment
The principles of treatment are similar in all hand infections. They are summarized in Table 80.2.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
