
Practical Plastic Surgery
.pdf
Chapter 77
Anatomy of the Hand
Zol B. Kryger
Introduction
The hand is a magnificently designed, complex organ with a large number of nerve endings, muscles, ligaments, bones and joints. These various structures function in a highly orchestrated manner, producing an organ capable of intricate motion and sensibility. This chapter will cover the anatomy of the fingers, hand and wrist, grouping structures based on their volar, dorsal or intrinsic anatomical location. Relevant clinical correlates will be given throughout. Much of the anatomy presented in this chapter is discussed elsewhere in the Hand Section of this text.
Intrinsic Anatomy
Bones and Ligaments of the Wrist
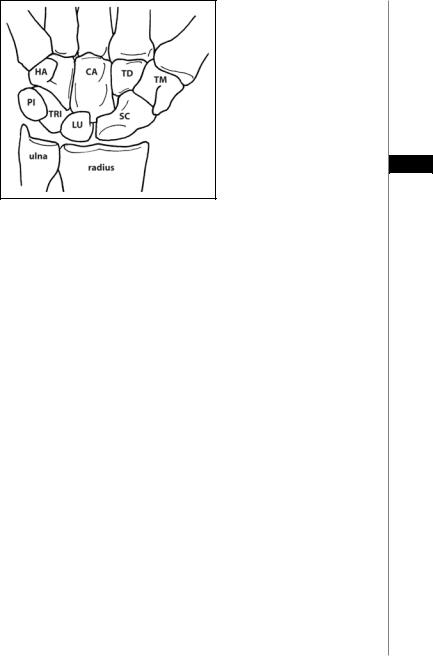
The wrist is composed of the distal radius and ulnar as well as the two rows of carpal bones (Fig. 77.1). The distal radius and ulna are joined by an interosseous membrane which is flexible enough to allow rotation of the radius around the ulna in pronation and supination. Pronator and supinator muscles course between the two bones, and the long flexor and extensor muscles of the wrist and fingers originate from these bones in the forearm. The radius articulates with the lunate and scaphoid at the lunate fossa and the scaphoid fossa. Ligaments join the scaphoid and lunate to the radius, and these articulations can also be the source of arthritic pain. The distal ulna articulates with the triquetrum through the triangular fibrocartilage complex (TFCC). The radius and ulna meet at the sigmoid notch and are joined by the TFCC forming the distal-radial-ulnar-joint (DRUJ), a frequent site of injury and arthritis. The ulna styloid lies most distally and laterally and is frequently involved in fractures of the distal radius. It is easily palpated on the dorsal surface of the wrist.
The proximal carpal row (from radial to ulnar) consists of the scaphoid, lunate, triquetral and pisiform. It has some motion about the radius, with the lunate serving as the fulcrum. The distal row consists of the trapezium, which articulates with the first metacarpal, trapezoid, capitate and hamate. The distal carpal row has very little motion and moves as a unit. The capitate is the fulcrum for this group of bones.
Bones and Ligaments of the Hand and Fingers
The fingers are comprised of three bones, the proximal, middle and distal phalanges. Each phalanx is further subdivided into a shaft, neck and head. The bones articulate at the proximal interphalangeal (PIP) and the distal interphalangeal (DIP) joints. The proximal phalanx articulates with the metacarpal bone at the metacarpophalangeal (MP) joint. There are five metacarpal bones that articulate proximally with the carpal bones at the carpometacarpal (CMC) joints. The first CMC joint (thumb) is very mobile. The second and third CMC joints have almost no mobility. The fourth and
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Anatomy of the Hand |
463 |
Figure 77.1. The carpal bones. HA, hamate. CA, capitate. TD, trapezoid. TM, trapezium. PI, pisiform. TRI, triquetrum. LU, lunate. SC, scaphoid.
77
fifth CMC joints have about 50˚ of mobility to aid in the power grip. The finger metacarpals are interconnected through the deep transverse metacarpal ligament. Lateral stability of the fingers is largely dependent on the radial and ulnar collateral ligaments located at the base of each digit. Rupture of a collateral ligament will result in instability and excess laxity on the side of injury. On the volar surface of these joints is the volar plate to which the collateral ligaments attach. During MP joint dislocations, the volar plate can slip into the joint space and interfere with anatomical reduction.
The thumb has only two phalanges, and thus only a single interphalangeal (IP) joint. The superior motion of the thumb over the digits is largely due to the extremely mobile CMC joint of the thumb. Unfortunately, this is also a common site for osteoarthritis to develop.
Intrinsic Hand Musculature
The intrinsic tendons are the dorsal interosseus muscles, the volar interossei, and the lumbricals. The four dorsal interossei insert onto the proximal phalanges, and abduct the fingers and weakly flex the proximal phalanx. The three volar interossei do not attach to bone but rather insert onto the lateral bands that unite with the lateral slips of the extensor tendons. They adduct the fingers and flex the PIP joint. The lumbricals arise from the tendon of flexor digitorum profundus (FDP) on the palmer side and insert onto the radial lateral band of each finger. They primarily extend the IP joints, as well as functioning as flexors of the MP joints. The intrinsic muscles are innervated primarily by the ulnar nerve, except for the first and second lumbricals, which are innervated by the median nerve. The intricate extensor, flexor and intrinsic systems are interconnected, aligned and stabilized with a system of ligaments found in each finger. The triangular, transverse retinacular and oblique retinacular ligaments perform a variety of complex actions. The pathology of these ligaments is addressed in the chapter on Dupuytren’s disease.
Compartments of the Hand
There are ten compartments in the hand: four dorsal interosseous, three volar interosseous, one thenar, one hypothenar, and one adductor pollicis compartment. In the fingers, the ligaments (Cleland’s, Grayson’s, and transverse retinacular) can also segregate the digit into compartments, resulting in a compartment syndrome of the neurovascular bundle.

464 |
Practical Plastic Surgery |
Volar (Palmar) Anatomy
Wrist
The most superficial tendon of the wrist is the palmaris longus. It is located roughly in the midline and is absent in 10-15% of patients. It is commonly used for tendon grafting procedures. Just radial to this tendon lies the palmar sensory cutaneous branches (PSCB) of the median nerve. It branches off 5-7 cm proximal to the wrist crease and terminates in the subcutaneous tissues overlying the thenar musculature.
Deep to these structures lies the carpal tunnel. The carpal tunnel is a space defined by the concave arch of the carpus enclosed by the transverse carpal ligament (TCL). The scaphoid, trapezium, and sheath of the flexor carpi radialis (FCR) make up its radial margin. The ulnar boundary consists of the triquetrum, the hook of the
77hamate, and pisiform. Ten structures course through the carpal tunnel. These include the median nerve, four flexor digitorum superficialis (FDS) and four FDP tendons, all ensheathed by the ulnar bursa, and the flexor pollicis longus, found at the radial side of the canal and surrounded by the radial bursa. The flexor carpi radialis tendon (FCR) travels through its own separate osteofibrous tunnel. The TCL itself attaches medially to the pisiform and laterally to the tuberosity of the scaphoid bone. The TCL can be severely thickened in carpal tunnel syndrome.
The median nerve is the most superficial structure within the carpal tunnel and is covered by a layer of cellulo-adipose tissue. The nerve lies directly under the TCL in the radiopalmar portion of the canal. The superficialis and profundus tendons of the index finger lie immediately dorsal to the median nerve. The nerve divides distally into five sensory branches and the recurrent motor branch. In 80% of cases, the motor branch arises from the radiopalmar region of the median nerve. In the remainder of patients the origin is in the central location, and a small percentage take-off from the ulnar aspect. Ten percent of patients have multiple motor branches. A sensory communicating branch between the median and ulnar nerves in the palm is present in 80% of patients, with roughly half lying within millimeters of the TCL. Injuries to this nerve have been reported during carpal tunnel release, leading to paresthesias or dysesthesias in the ulnar digits.
Guyon’s canal is located on the ulnar aspect of the wrist and contains the ulnar artery and nerve. Its floor is the TCL and lies just radial to the pisiform.
Palm and Fingers
The skin of the palm is thick and tough due to the stratum corneum. The dermis is actually of similar thickness to the skin of the dorsum of the hand. The palmar skin is firmly anchored to the palmar fascia through a network of vertical fibers. The palmar fascia is also anchored to the underlying metacarpals. Thus edema fluid cannot easily collect in the palm; however an abscess (collar-button abscess) can develop in the tight space of the palm. The palmar fascia extends into the fingers, and a number of the ligaments of the fingers attach to this fascia. In Dupuytren’s disease, this fascia can become thickened and diseased.
The flexor tendons course through the palm en route to the fingers. Superficial to the tendons lies the superficial palmar arch. This arch is the terminating anastomosis between the ulnar artery and the palmar branch of the radial artery. The digital arteries arise from the superficial palmar arch. Deep to the flexor tendons is the deep palmar arch. It too is a terminal anastomosis between the radial and ulnar circulation. The volar metacarpal arteries originate from the deep arch. The rich anastomosis between the radial and ulnar arteries accounts for expendability of the radial artery (e.g., for CABG or free flap) in close to 100% of patients without any long-term sequelae in the hand and fingers.

Anatomy of the Hand |
465 |
The tendon of FDS inserts on the volar aspect of the middle phalanx, and the FDP tendon inserts on the volar aspect of the distal phalanx. FDS flexes the PIP joint and FDP flexes primarily the DIP joint. In the digits, the flexor tendons travel in synovial-lined tunnels called flexor tendon sheaths. The sheaths are anchored to the bones by a series of five annular pulleys, numbered A1-A5 from proximal to distal. The odd numbered pulleys are located over the joints; the even pulleys lie over the bones. There are three thin cruciate pulleys, numbered C1-C3, that maintain tendon motion and collapse during flexion. The palmer aponeurosis lies proximal to the A1 pulley and is often referred to as the A0 pulley. It acts in unison with the first two annular pulleys. Proximal to the entrance into the digital sheath (A1 pulley), the FDS tendon lies palmer to the FDP tendon. At this point, the FDS tendon divides and becomes deep to the FDP tendon. The two portions reunite at
Camper’s chiasma and go on to attach to the middle phalanx. The FDP tendon, 77 after passing through the FDS bifurcation, attaches to the distal phalanx.
Flexor pollicis longus (FPL) is the primary flexor of the thumb. It is the most radial structure in the carpal tunnel. It travels in its own fibrous sheath in the palm and inserts into the base of the distal phalanx of the thumb. The thumb, unlike the fingers, has two annular pulleys, A1 and A2, located over the MP and IP joints, respectively. Lying between them is an oblique pulley that is the most important of these three pulleys.
Fingertip
The fingertip is the end organ for touch, enabling the hand to relay the shape, temperature, and texture of an object. The skin covering the pulp of the finger is very durable and has a thick epidermis with deep papillary ridges. The glabrous skin of the fingertip is well-suited for pinch and grasp functions. Its volar surface consists of a fatty pulp covered by highly innervated skin. The skin of the fingertip is firmly anchored to the underlying terminal phalanx by multiple fibrous septa that traverse the fatty pulp. Hence an infection that develops within the pulp can result in a closed space infection, or felon.
Dorsal Anatomy
Wrist
The extrinsic muscles that extend the hand and fingers enter the wrist through six synovial-lined, dorsal compartments covered by the extensor retinaculum. At the wrist, the tendons are surrounded by a sheath, but this sheath is not present in the hand and fingers. The six compartments are numbered 1-6 from radial to ulnar:
1.Abductor pollicis longus (APL), extensor pollicis brevis (EPB)
2.Extensor carpi radialis brevis (ECRB), extensor carpi radialis longus (ECRL)
3.Extensor pollicis longus (EPL)
4.Extensor digitorum communis (EDC), extensor indices proprius (EIP)
5.Extensor digiti minimi (EDM)
6.Extensor carpi ulnaris (ECU)
The first compartment is commonly involved in stenosing tenosynovitis, termed
de Quervain’s disease. The second compartment contains the radial extensors of the wrist, and this compartment is located beneath the anatomic snuffbox. The hollow of the snuffbox (so named because it was a common site for the placement of snuff ) is easily created by extending and abducting the thumb. The radial artery passes through the snuffbox, and the scaphoid bone is deep to it. Therefore, tenderness in the snuffbox can be seen in scaphoid fractures. The second and third compartments are separated by Lister’s tubercle.

466 |
Practical Plastic Surgery |
Hand and Fingers
The four fingers are extended by EDC; however the communis tendon to the little finger is present only 50% of the time. The index and little fingers also have independent extensor muscles—EIP and EDM, respectively. These tendons usually lie ulnar and deep to the communis tendons to these two fingers.
The EDC tendons are joined proximally to the MP joints by the juncturae tendinum. They are almost always present between the EDC of the middle, ring and little fingers. Thus, lacerations proximal to the juncturae may not impair digit extension due to the connection to the adjacent digits. The tendons inserts proximally into the MP joint volar plate through attachments known as the sagittal bands. Distal to the MP joint, the extensor tendons divide into one central and two lateral slips. The central slip inserts into the middle phalanx and extends the PIP joint. The
77 lateral slips reunite distally and attach to the distal phalanx, extending the DIP joint. The thumb is extended by three tendons: the first metacarpal by APL, the proximal phalanx by EPB, and the distal phalanx by EPL. However, the MP and IP joints of the thumb can both be extended by EPL due to the attachments of the dorsal apparatus. It is worth mentioning that the IP joint of the thumb is extended by the combined actions of all three major nerves: the radial nerve (EPL), the median nerve
(thenar muscles) and the ulnar nerve (adductor pollicis).
Deep to the extensor tendons and proximal to the metacarpals lies the dorsal carpal arch. This is the dorsal anastomosis between the radial and ulnar circulation. The dorsal metacarpal arteries originate from this arch.
Fingertip
The fingernail protects the fingertip and has a major role in tactile sensation and fine motor skills. The nail complex, or perionychium, includes the nail plate, the nail bed, and the surrounding skin on the dorsum of the fingertip (paronychium). The fingernail is a plate of flattened cells layered together and adherent to one another. The nail bed lies immediately deep to the fingernail. The nail bed is composed of the germinal matrix, the sterile matrix, and the roof of the nail fold. The germinal matrix, which produces over 90% of nail volume, extends from the proximal nail fold to the distal end of the lunula. The lunula represents the transition zone of the proximal germinal matrix and distal sterile matrix of the nail bed. The sterile matrix (ventral nail) contributes additional substance largely responsible for nail adherence. The roof of the nail fold (dorsal nail), which includes the germinal matrix, is responsible for the smooth, shiny surface of the nail plate. The hyponychium is the area immediately below the fingernail at its cut edge which serves as a barrier to subungual infection, and also marks the terminal extension of bone support for the nail bed. The eponychium is the skin covering the dorsal roof of the nail fold. The paronychium is the skin at the nail margin, folded over its medial and lateral edges.
Innervation of the Hand and Fingers
The median, ulnar and radial nerves are the primary nerves of the hand and fingers. The first two have both motor and sensory fibers, whereas the radial nerve provides only sensory fibers to the hand. Its motor branches terminate in the arm and forearm.
Median Nerve
The median nerve travels in the forearm between the muscle bellies of FDP and FDS and provides motor input to most of the flexors of the forearm. Just proximal to the wrist, it gives off the palmar cutaneous branch which supplies sensation to the

Anatomy of the Hand |
467 |
thenar region. At the wrist it enters the carpal tunnel, where it is the most superficial of the structures that traverse this tunnel as described above. It then gives off the motor branch which innervates the radial side of the thenar muscles: opponens pollicis, abductor pollicis brevis, the superficial part of flexor pollicis brevis, as well as the two radial lumbricals. Finally, it divides into sensory branches whose territory includes the palmar surface of the thumb, index, middle, and radial side of the ring fingers, and the radial side of the palm (palmar sensory branch). On the dorsal surface, it sends sensory branches to the distal third of the above-mentioned fingers.
The most consistent sign of median nerve injury is loss of skin sensibility on the palmer surface of the first three digits and loss of thenar opponens function.
Ulnar Nerve
The ulnar nerve travels in the forearm ulnar to the FDP muscle belly. It gives off 77 its palmar sensory branch proximal to the wrist. At the wrist it travels in Guyon’s canal, after which it begins to branch into many motor and sensory branches. It innervates all the intrinsic hand muscles except those mentioned above that are innervated by the median nerve. The last muscle innervated by the ulnar nerve is the
first dorsal interosseus nerve. Its sensory territory includes both the palmar and dorsal sides of the little finger and the ulnar side of the ring finger.
A common sensory sign of ulnar nerve injury is the loss of sensibility to the small and ulnar side of the ring fingers. Motor signs include FCU paralysis, interosseous and thumb adduction loss with a weak “key pinch,” and FDP paralysis of the small and ring fingers. A long-standing injury can present with the classic “claw hand” deformity.
Radial Nerve
The radial nerve provides all the motor innervation of the extensor muscles of the forearm. Only the superficial branch of the radial nerve reaches the hand. This purely sensory nerve travels over the radial side of the wrist. It then branches into the dorsal digital nerves that supply the skin on the dorsum of the thumb, index, middle, and radial side the ring fingers (with the exception of the distal third of each which is supplied by the median nerve).
Signs of injury include loss of sensibility on the dorsum of the hand and in the first web space. Patients will be unable to extend their fingers.
Pearls and Pitfalls
A resource that is highly recommended for understanding hand anatomy and anatomic relationships is The Interactive Hand CD-ROM (McGrouther DA, Colditz JC, Harris JM, Eds.) published by Primal Pictures, Inc. 2002. The upper extremity can be rotated and displayed from various angles, and it can be viewed layer by layer from bone to skin.
Suggested Reading
1.Bogumill GP. Functional anatomy of the flexor tendon system of the hand. Hand Surg 2002; 7(1):33-46.
2.Furnas DW. Anatomy of the digital flexors: Key to the flexor compartment of the wrist. Plast Reconstr Surg 1965; 36(3):315-9.
3.In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, eds. Green’s Operative Hand Surgery. 5th ed. New York: Churchill Livingstone, 2005.
4.Lister’s The Hand. In: Smith P, ed. Diagnosis and Indications. 4th ed. New York: Churchill Livingstone, 2002.
5.Rockwell WB, Butler PN, Byrne BA. Extensor tendon: Anatomy, injury, and reconstruction. Plast Reconstr Surg 2000; 106(7):1592-603.
Chapter 78
Radiographic Findings
Zol B. Kryger and Avanti Ambekar
Introduction
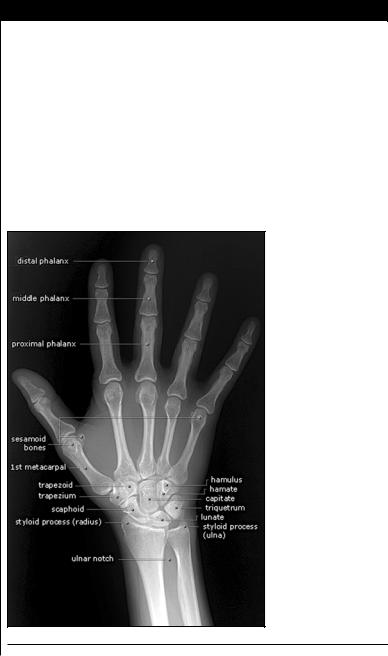
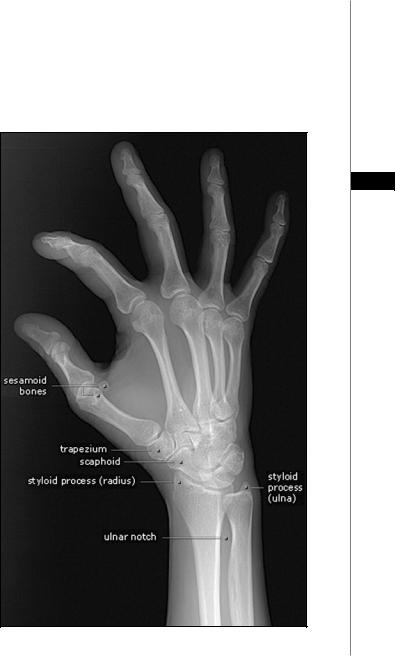
Radiologic diagnosis of bony hand injury and deformity is often successfully achieved with conventional radiographs, despite advances in cross-sectional imaging. At least two orthogonal views should be performed routinely. Special views, such as the scaphoid view, can be helpful in selected cases. The images shown in this chapter were obtained and reprinted with permission from the website http:// www.gentili.net.
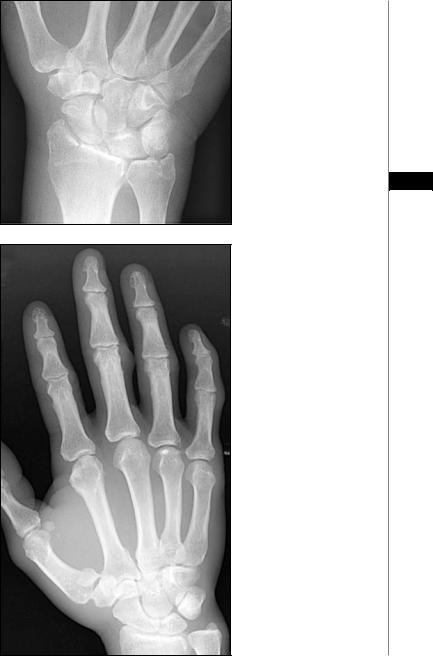
Figure 78.1. P-A view of a normal hand radiograph.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
Radiographic Findings |
469 |
A Systematic Approach
An organized evaluation is required for all image interpretation. The patient’s name, date of exam, correct body part, and laterality (right or left side) should be verified prior to analyzing the image. The exam should be assessed for quality and completeness. Attention can then be turned to film interpretation. The bones, joint spaces, and soft tissues should be sequentially inspected. Each feature should be evaluated in a systematic fashion (e.g., from proximal to distal). All abnormalities should be confirmed on a second view.
78
Figure 78.2. Oblique view of a normal hand radiograph.

470 |
Practical Plastic Surgery |
Figure 78.3. Osteoarthritis of the hand, with joint space narrowing and adjacent bony sclerosis. The DIP joints and 1st CMC joint (thumb) are characteristically involved.
78
Figure 78.4. Osteoarthritis of the fingers. Note greater involvement of the DIP joints compared to the IP joints.
Figure 78.5. Fracture of the scaphoid bone. The scaphoid is the most commonly fractured carpal bone, accounting for 80% of all carpal fractures. It is often the result of a fall on an outstretched hand. Scaphoid fractures are at high risk for nonunion and avascular necrosis.
Radiographic Findings |
471 |
Figure 78.6. Fracture of the radial styloid, also termed a chauffeur’s fracture. A scapholunate ligament tear often accompanies this fracture.
78
Figure 78.7. Fracture of the first metacarpal base, If it is intra-articular, it is referred to as a Bennett fracture. If it also demonstrates comminution, it is called a Rolando fracture.
