
Practical Plastic Surgery
.pdf
|
442 |
Practical Plastic Surgery |
||
|
|
|
|
|
|
|
|
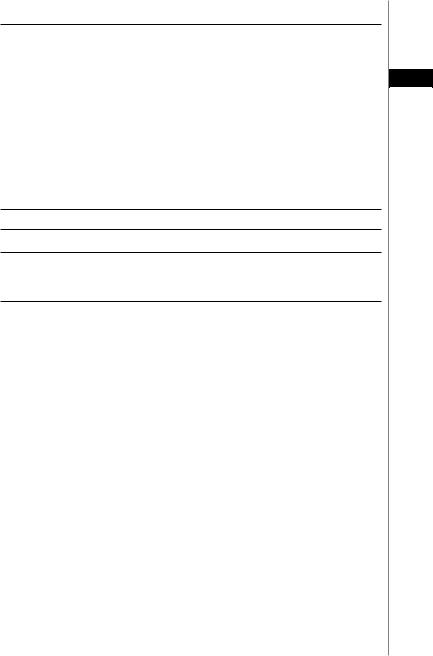
Table 72.2. Fitzpatrick classification system of skin types |
|
|
|
|
|
|
|
|
|
Type |
Skin Characteristics |
|
|
|
I, extremely fair or freckled skin |
Always burns, never tans |
|
|
|
II, fair skin |
Usually burns, sometimes tans |
|
|
|
III, fair to olive skin |
Sometimes burns, always tans |
72 |
||||
|
|
|
IV, olive to brown skin |
Rarely burns, always tans |
|
||||
|
|
|
V, dark brown skin |
Very rarely burns, always tans |
|
|
|
VI, black skin |
Never burns, always tans |
•The main contraindication for superficial peels is the presence of active skin disease such as rosacea, seborrheic dermatitis, atopic dermatitis, psoriasis and vitiligo. Rosacea skin is particularly sensitive to peeling. Consideration for a very superficial peel such as salicylic acid should be given for patients with this skin condition due to the peel’s anti-inflammatory properties.
•As a general rule, Fitzpatrick skin types I-III (Table 72.2) will tolerate all depths of resurfacing with little risk of pigmentary changes. In contrast, Fitzpatrick skin types IV-VI have a higher risk of hyperand/or hypopigmentation, and patients should be aware of this possible outcome. Deep peels should not be performed on patients with these skin types. Superficial peels, especially salicylic acid peels, are still safe in even the most highly pigmented skin.
General Considerations
All patients should be adequately prepared for the procedure. This includes counseling and explanation of all the risks and benefits. It is controversial whether or not topical tretinoin should be used nightly preprocedure as it enhances peel penetration. Use of tretinoin is restricted in the postoperative period until complete reepithelialization and inflammation has subsided. Topical hydroquinone is another potential adjuvant therapy to be considered in the preand postprocedural periods, especially in darker skinned individuals. In the postoperative period, strict sun precautions and sun avoidance must be insisted upon to minimize pigmentary changes.
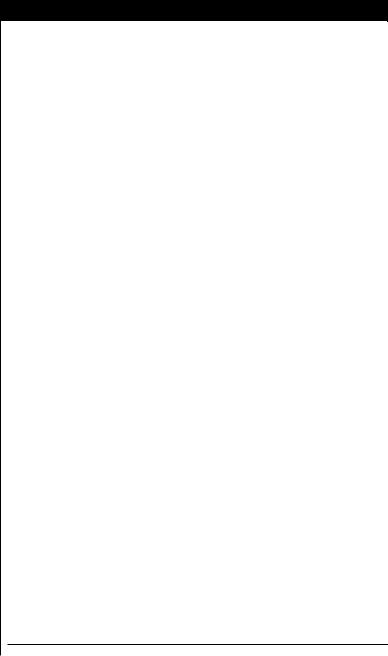
The need for intraoperative sedation and analgesia should be considered mainly for deep peels (Table 72.3). The patient’s own pain threshold, anxiety level, comorbid medical conditions, and willingness to take on the financial burden of heavier sedation are all factors to be considered.
Superficial peels require only gentle face washing. For medium and deep peels, residual oils, debris and excess stratum corneum must be removed with vigorous cleansing prior to applying a chemical peel solution. Cleansing and degreasing assures uniform penetration of the peeling solution and even results without skip areas. If any residual oil is felt after this, the process should be repeated prior to peeling.
Specific markers help to determine the appropriate endpoint for a given chemical peel. This varies depending on the chemical agent used. For example, frosting, or the whitening of skin after the chemical is applied, is an important indicator of how evenly trichloroacetic acid (TCA) been applied. The extent of photodamage, the applicator utilized, and the adequacy and uniformity of defatting all impact the frost achieved. It is not a valuable marker of depth. Table 72.4 reviews the levels of frosting. The following sections will specifically discuss superficial, medium and deep peels and highlight one example in each class.
Chemical Rejuvenation of the Face |
443 |
|
|
|
|
Table 72.3. Examples of anesthesia for facial resurfacing |
|
Superficial Resurfacing Procedures |
|
• No sedation or analgesia is required |
|
Medium-Depth Peels |
72 |
Limited degree of perioperative sedation and analgesia, such as: |
•Topical amide anesthetics
•Regional blocks of the supraorbital, infraorbital and mental nerves
•Oral diazepam
•Intramuscular meperidine hydrochloride
•Intramuscular hydroxyzine hydrochloride
Deep Resurfacing Procedures
•Nerve blockade, local injections of lidocaine and mild sedatives
•Intravenous or general endotracheal tube anesthesia
•Tumescent anesthesia technique
Table 72.4. Levels of frosting of the skin during chemical peeling
Level I Erythema and streaky white frosting
Level II Erythema with a solid white enamel frosting
Level III Solid white enamel frosting without erythema
Superficial Chemical Peeling
Multiple peels will usually be necessary to achieve optimal results. Superficial peels have the advantage of very little stinging or burning during the procedure with little recovery time afterwards. Multiple peels in some circumstances can give results similar to medium-depth or deep peels when the goal of the procedure is destruction of superficial photodamage. There are very light and light superficial peels. Very light peels slough the stratum corneum and stratum granulosum in a process known as exfoliation. Light peels extend deeper, through the entire depth of the epidermis. This stimulates regeneration of fresh, new epithelium. Examples of very light superficial peels include low potency formulations of glycolic acid and other alpha-hydroxy acids, salicylic acid, 10%-20% trichloroacetic acid (TCA) and resorcin. Light superficial peels include 25%-35% TCA, Jessner’s solution and 70% glycolic acid.
30%-70% Glycolic Acid
Weekly or biweekly 40%-70% unbuffered glycolic acid is one method of light peeling. Patient’s skin develops tolerance to glycolic acid peels. Therefore, a typical regime of six peels would start with a low strength glycolic peel of perhaps 30% applied for three minutes. Erythema and patient level of pain are pertinent factors in determining the appropriate endpoint for glycolic acid peels. The peels are spaced one month apart. At the next visit, the patient would be questioned about length of recovery, pain and possible benefits. Only the rare patient would have significant pain or erythema after such a light peel. Assuming she tolerated the first peel well, the next peel could either be 30% left on the skin longer, such as 5 or 6 minutes or the patient could be graduated up to a 40 or 50% peel. At each visit, the process of evaluating the patient and selecting the correct peel and peeling time would be repeated. Unlike TCA

444 |
Practical Plastic Surgery |
peels or salicylic acid peels which self-neutralize, glycolic acid must be rinsed off with water or neutralized with 5% sodium bicarbonate after 2-4 minutes. However, neutralization with bicarbonate may produce heat and some practitioners avoid this.
Medium-Depth Chemical Peeling
Controlled wounding in medium-depth chemical peels extends through the epi-
72dermis and papillary dermis to the upper reticular dermis. The most commonly
used medium-depth chemical peels include combination peels such as solid CO2 + 35% TCA, Jessner’s + 35% TCA and 70% glycolic acid + 35% TCA. Acutely, there is epidermal necrosis and papillary dermal edema. Visible healing occurs over the ensuing 1 to 2 weeks. Patients frequently do not feel comfortable returning to work for several days because they may have light scabs or open areas on their face. Over the next several months there is increased collagen production and organization, which correlates clinically with wrinkle reduction. 50% TCA as a single agent is not used as widely given the frequency of scarring and pigmentary changes. The efficacy of 35% TCA in combination with several agents (see Table 72.1) reaches that of 50% TCA alone without the associated complications. The depth of the peel determines how efficacious it will be, which is determined in part by effective degreasing preprocedure as well as how much of each solution is used. Care must be taken to avoid ocular damage when treating the eyelids.
35% TCA
The combination of 35% TCA with glycolic acid, Jessner’s solution, or solid CO2 generates a white frost almost immediately. A uniform level II or III frosting is the desired endpoint. There should be at least a three to four minute break period before retreating any area to guarantee that maximal frosting has occurred. Retreating over frosted areas should be approached with great caution because penetration can be variable in the previously damaged skin. An acute sensation of burning occurs with peel application; this generally subsides once frosting is present.
Deep Chemical Peeling
Deep chemical peeling is a very safe procedure when performed by an experienced physician. Many newly trained physicians have replaced deep peels with skin laser resurfacing as the latter may provide more control over depth of dermal injury. With deep chemical peeling, injury extends to the midreticular dermis with consequent production of new collagen. Two options exist for deep chemical peeling: TCA solutions and phenol-based compounds. As is true for medium-depth peels, >50% TCA peels have associated complications and are used less frequently.
The Baker-Gordon Peel
This phenol-based peel must be freshly prepared and mixed well prior to use. It can be applied under occlusion to increase penetration and extend injury deeper into the midreticular dermis. The chemical agent is sequentially applied with 15 minute intervals between each of six aesthetic units: forehead, perioral region, right cheek, left cheek, nose and periorbital area after complete cleansing and degreasing. Care must be taken to avoid scarring and ectropion formation when treating periorbital skin. If there is ocular involvement, mineral oil should be used to flush the eyes, as water increases the penetration of phenol. Pain relief should be addressed appropriately. Intravenous hydration with lactated Ringer’s solution prior to and during the procedure helps promote phenol excretion and prevent toxicity.

Chemical Rejuvenation of the Face |
445 |
Surveillance during the perioperative period must include continuous electrocardiography, pulse oximetry and blood pressure monitoring.
Patient’s undergoing deep chemical peels must be completely aware of the significant risk of complications and morbidities including scarring, textural changes and pigmentary disturbances. A key point to mention to patients is that new collagen formation
takes months to occur. Therefore, they can expect significant skin tightening even 6 72 months after their procedure. In addition, phenol is cardiotoxic and is eliminated by the
liver and kidneys. For this reason, preoperative evaluation including complete blood count, liver function tests, basic metabolic panel and a baseline electrocardiogram. Patients with known arrhythmias should not undergo phenol peels. Serious consideration should be given for any patients with known hepatic or renal insufficiency prior to the procedure. Appropriate patient selection cannot be over-emphasized.
Pearls and Pitfalls
It is prudent to start with a low strength concentration for peels to ensure the patient is not unusually sensitive to any ingredient. When a practitioner is just starting to use peels, salicylic acid is a good choice, since its penetration is superficial and it self neutralizes. Another key advantage of salicylic acid is that it is lipophilic and therefore penetrates into the hair follicle. For this reason, it may also be the best peel for acne and may help to at least temporarily shrink pores.
Regarding skin preparation, gentle face washing prior to superficial chemical peels is important. Before medium-depth peels, facial skin can be prepped with application of Jessner’s solution. Deep peels should be preceded by a medium depth peel such as acetone, Jessner’s, or 30% glycolic acid.
During application of any chemical peel, care should be taken to never pass over the patients’ eyes and to very cautiously apply solution to the nasal root or bridge in order to avoid dripping and the solution running into the eyes. Don’t use the spray applicator for rinsing because the partially neutralized solution can run into the eyes. Be careful with heavily soaked saline gauze around the eyes, as a trickle of saline can collect peeling agent. The first round of neutralization is done with moist gauze, and only then is more heavily soaked cool gauze used.
Determining the correct time to neutralize a glycolic peel is tricky, because the depth of injury relates both to the time on the skin as well as the concentration. The two key factors to follow are skin erythema and patient’s pain perception. Tell the patients to alert you if any area develops a 5 out of 10 or higher pain threshold. The other endpoint is erythema. Ideally, you should see a light to medium pink color, almost like a wind burn. Any area that gets deeper red is immediately neutralized. In summary, neutralization times are different for each facial area, and areas that require early neutralization should be noted in the chart.
Many physicians use a fan for reducing the pain of the procedure. There is one exception: don’t use the fan during glycolic peels until you make the decision to neutralize because a genuine assessment of the patient’s pain threshold must be noted. A blowing fan in close proximity to the patient’s face should be utilized once an estimated pain level of 5 out of 10 is reached.
Suggested Reading
1.Brody HJ. Chemical Peeling and Resurfacing. 2nd ed. St. Louis: Mosby, 1997.
2.Drake LA et al. Guidelines of care for chemical peeling. Guidelines/Outcomes Committee: American Academy of Dermatology. J Am Acad Dermatol 1995; 33:497.
3.Glogau RG. Chemical peeling and aging skin. J Geriatr Dermatol 1994; 2(1):30.
4.Mendelsohn JE. Update on chemical peels. Otolaryngol Clin North Am 2002; 35(1):55.
Chapter 73
Fat Injection and Injectable Fillers
Darrin M. Hubert and Louis P. Bucky
Overview
Contour deformities of soft tissues confront the plastic surgeon in both aesthetic and reconstructive endeavors. Atrophy of fat and subcutaneous tissue manifests itself in the characteristics of the aging face. In addition, chronic acne may result in destruction of subcutaneous tissues due to repeated inflammation. Other soft tissue defects include traumatic injuries, secondary cleft deformities, Romberg’s disease (hemifacial atrophy), iatrogenic defects such as those caused by liposuction and mid-face hypoplasia. The ideal soft tissue filler should be safe, predictable, easy to use, readily available and have a reasonable duration. At present, there is no consensus as to a perfect single injectable material for soft tissue volume augmentation. Fillers can be divided into those that can produce volume augmentation and those that can correct fine lines.
Fat Grafting
Autologous fat grafting has a long history. Recently it has regained renewed popularity due to advances in technique that have led to more reliable results. Fat represents the ideal facial soft tissue filler for both aesthetic and reconstructive purposes. The advantages are several. The use of autologous fat obviates the concern for an immunogenic response. The donor tissue is often in abundant supply, even when fairly large volumes are required. This safe procedure is technically easy to perform and generally well tolerated. Patients easily understand the concept of volume loss and are receptive to replacement procedures. Lastly, the majority of facial volume loss over time is due to fat atrophy. Thus replacing similar tissues is preferable.
Variable graft survival with long-term unpredictable success represents the major shortcoming of fat grafting. Typically a percentage of the grafted fat will undergo resorption, which sometimes necessitates additional procedures. Some authors advocate over-correction at the initial procedure in anticipation of losing some volume over time. The literature reports widely disparate results with a two-year average of about 50% (range 30%-70%) persistence of the injected fat. These reports, however, are plagued by differences in the methods of fat harvesting, processing and injection.
Technique
Adipose tissue is extremely fragile. Therefore fat must be harvested with minimal trauma. The entire procedure should create only a minimum of physical and chemical disruption, and the fat specimen should have only limited exposure to the air. The specimen is at no point washed with saline or lactated Ringer’s solution. Strict adherence to sterile technique must be observed. The majority of the time, small
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

Fat Injection and Injectable Fillers |
447 |
volumes of fat may be harvested and injected under local anesthesia. For larger volumes and anxious patients, however, sedation may be required.
Typical harvest sites include the abdominal wall, flanks and hips. A small stab incision is made at the donor site. The fat is obtained with a 10-ml Luer-lock syringe attached to a blunt cannula. Low-pressure suction is applied manually by withdrawing the plunger while passing the two-holed cannula (ByronTM) to minimize tissue trauma. Coleman and others popularized centrifugation of fat to fa-
cilitate the separation of the specimen into three layers. The authors, however, 73 have modified the process and do not employ centrifugation. The syringe is allowed to stand in a vertical position for a period of minutes. Then the specimen is gently injected onto a Telfa® pad and rolled with the end of a blunt instrument,
e.g., an empty scalpel handle. This atraumatic process is continued until the specimen reaches its purified, natural yellow color and achieves a meringue consistency. It is then immediately returned to the 10 ml syringe and subsequently transferred to 1 ml tuberculin syringes for injection with a blunt microinjection cannula (ByronTM).
The recipient site is prepared in a sterile fashion, and a percutaneous puncture is made with iris scissors. Small aliquots (< 0.1 ml) of fat are injected in multiple subcutaneous planes. The puncture site may be closed with a simple 6-0 fast-absorbing plain gut suture. Because fat survival depends on the diffusion of nutrients, over-correction of no greater than 10% is preferred. Significant over-correction or traumatic harvest techniques lead to greater resorption, cyst formation and fibrosis, and should therefore be avoided.
Motion tends to diminish fat survival. Hence, static recipient areas usually result in greater graft survival than do dynamic ones. The malar, periorbital and parasymphyseal regions of the face are more reliable in terms of maintenance of volume. Results with the upper nasolabial fold appear to be better than in the lower marionette region, once again due to an absence of inherent motion. Fat injection in the glabellar region can be enhanced with preoperative botox injection in order to diminish motion and improve graft survival. Lip injection is complicated for two reasons. First, persistent motion in this area leads to unpredictable results, and second, fat grafting to the lips is associated with prolonged edema. However, use of a small 20-gauge cannula seems to decrease postoperative edema in this area. The same small cannula is effective in the nasojugal groove region in order to avoid over-correction and palpability. In addition, the thin skin of the lower eyelid region requires fat grafting to be performed deep to the orbicularis oculi muscle.
Other variables that impact fat survival in the face are the age of the patient, presence of subcutaneous scarring, and degree of the deformity. Secondary procedures typically should occur at six-month intervals in order to diminish inflammation and fibrosis. Other untoward sequelae are extremely rare but can include hematoma, infection, necrosis of overlying tissues and erythema. Ultimately fat grafts are living adipose tissue, and they tend to diminish concurrent with the normal aging changes to the face. Fat grafting, when performed utilizing appropriate care in harvest, processing and injection, can be an extremely useful technique for soft tissue augmentation. It is useful in isolation as well as in combination with other surgical procedures.

448 |
Practical Plastic Surgery |
Other Injectable Fillers
Efforts have been made to develop synthetic fillers for volume augmentation. The advantage of these other fillers lies in the fact that they are essentially available “off the shelf.” RadiesseTM (BioForm Medical, San Mateo, CA) represents a suspension of synthetic bioceramic microspheres (25-45 μm diameter) comprised of calcium hydroxylapatite in a gel carrier. Indications approved by the FDA include
73vocal cord augmentation and filling of maxillofacial defects. Although more common elsewhere, its off-label use for facial soft tissue augmentation is becoming increasingly more common within the United States. It is supplied in single-use, 1.0 ml and 0.3 ml syringes and can easily be injected through a 26-gauge needle. Metabolism is the same as that for endogenous bone fragments. The durability of RadiesseTM, therefore, is significant and ranges from several months to years. It works best in regions with significant soft tissue cover, e.g., the malar area, nasolabial folds, marionette lines and the parasymphyseal region. Likewise, it should be avoided under thin tissues such as the eyelids and oral mucosa. The authors have found RadiesseTM to be particularly useful in patients with HIV-associated soft tissue atrophy or fat grafting failures. The most common complication is palpability.
SculptraTM (Dermik Laboratories, Berwyn, PA) is an injectable suspension of microparticles composed of poly-L-lactic acid, a member of the alpha-hydroxy acid family. It is presently FDA-approved for the treatment of facial lipoatrophy in patients with HIV. Although this synthetic implant is biodegradable, volume effects may still be evident up to two years after injection. For this reason, over-correction is not recommended. However, multiple treatment sessions (3-6) at approximately two-week intervals may be required to achieve optimal effect. No skin test is required. It is supplied as a freeze-dried preparation that is reconstituted in sterile water and 2% lidocaine. Injection involves 0.1 to 0.2 ml aliquots in the deep dermis or subcutaneous planes of the cheek or nasolabial region with a 26-gauge needle. Side effects include bruising, edema and the delayed appearance of subcutaneous papules that are palpable in the region of injection.
Hyaluronic Acid
Other injectable fillers have been developed which are utilized primarily in the treatment of fine lines and wrinkles. Synthetic fillers such as hyaluronic acid are rapidly replacing collagen, long considered the “gold standard” of soft tissue injectable fillers. This is due to three main reasons. First, no skin test is required as is the case with collagen. Second, the longevity of hyaluronic acid is slightly greater than that of collagen. Third, it has an ease of injection similar to that of collagen. Chemically identical across all species, hyaluronic acid consists of a long-chain polysaccharide of repeating disaccharide units of glucuronic acid and N-acetyl glucosamine. Because of this structure, hyaluronic acid avidly binds water, which imparts its significant viscoelastic characteristics. It is ultimately degraded due to hyaluronidase activity although molecular cross-linking slows this degradation process.
Restylane® (Q-Med, Uppsala, Sweden) is a nonanimal stabilized (cross-linked) hyaluronic acid that can be used for volume augmentation. Derived from engineered bacteria, it has an attractive safety profile. Injection typically produces no palpability. However, its lack of longevity (3-6 months) and cost make it a better choice for sensitive areas like the lower eyelids and lips. Restylane® is supplied in

Fat Injection and Injectable Fillers |
449 |
prepackaged 0.5 ml and 1.0 ml sterile syringes at a concentration of 20 mg/ml. A 30-gauge needle is provided for injection into the middle dermis, and over-correction is not recommended.
A second hyaluronic acid gel, Hylaform® (Inamed, Santa Barbara, CA), is FDA-approved. Derived from rooster combs, it should be avoided in individuals with an allergy to any avian protein. It is indicated for facial volume augmentation in wrinkles and folds, where it is injected in a fashion similar to Restylane into the
midto deep dermis. The longevity profile, compared to Restylane, has not been 73 determined. However, its cross-linked nature is associated with less swelling, which
may be of particular importance in the lips.
Collagen
The most abundant protein in the human body, collagen comprises roughly 30% of its dry weight. It is a triple-helix composed of polymers of primarily three amino acids: glycine, proline and hydroxyproline. The most favorable results with collagen are obtained in correction of fine to medium lines and soft, mobile scars. The main drawbacks of collagen include the potential for a skin reaction. Moreover, the duration of collagen is limited to 3-4 months, and it is removed by an inflammatory process which may result in erythema. Of critical importance is the technique of injection: collagen is injected in small volumes within the dermis. Most of the implanted volume is eventually degraded, and often several injection sessions, or “touch-ups,” may be required to achieve long-term volume persistence. This can be prohibitively expensive and time-consuming. Many authors recommend over-correction of lesions whenever possible.
Commercially available collagen has historically been derived from both human (typically of cadaveric origin) and bovine sources. Injectable bovine collagen, FDA-approved since 1981, has been associated with hypersensitivity reactions in 1.3% to 5% of patients. Thus a skin test is recommended before initiation of therapy. Bovine collagen has long been available in two forms, marketed under the names Zyderm® (Inamed, Santa Barbara, CA) and Zyplast® (Inamed). Both are suspensions of dermal collagen in saline solution with lidocaine. These products undergo selective hydrolysis of the terminal peptides to decrease antigenicity. Despite this, however, hypersensitivity skin testing is positive about 3% of the time. The use of Zyderm® and Zyplast® is rapidly waning.
CosmoDerm® (Inamed) and CosmoPlast® (Inamed) are utilized in much the same fashion as Zyderm® and Zyplast®. They are comprised of collagen which is isolated and purified from human dermal fibroblasts grown in culture. As such, no skin test is required. They are dispersed in physiologic saline solution with 0.3% lidocaine. CosmoDerm-1 (35 mg/ml) is injected with a 30-gauge needle into the superficial dermis for shallow scars and fine lines and wrinkles, especially in the perioral region. Over-correction of approximately 1.5 to 2 times is recommended. CosmoDerm-2 is similar to CosmoDerm-1 but, at nearly twice the concentration, it requires less over-correction. CosmoPlast (35 mg/ml) is cross-linked with glutaraldehyde, which increases its longevity. Particularly effective for deeper lines such as the nasolabial folds, it is injected into the mid-to-deep dermis of furrows and scars. These products are supplied in disposable single-use only syringes that may be stored in a refrigerator.

450 |
Practical Plastic Surgery |
Isolagen® (Isolagen, Inc., Houston, TX) is derived from autologous fibroblasts cultured from a 3-mm retroauricular skin biopsy. A period of approximately six weeks is required to produce roughly 1.0 to 1.5 ml for injection. No skin test is required. Living fibroblasts, the cells that produce collagen, are injected with a 30-gauge needle into the superficial dermis. Although Isolagen has not achieved widespread acceptance, investigational studies continue to evaluate this product.
73 Pearls and Pitfalls
The key to effective facial filling is to be able to differentiate between fillers that are used for volume augmentation from fillers that are used to obliterate fine lines. Fat grafting is the gold standard for volume augmentation. Careful harvest, purification and injection of fat are required around the face for volume augmentation. It is most useful in areas where there is minimal motion. Over-correction is routinely not successful, and if secondary corrections are required, waiting six months is typically appropriate. In addition, the use of fat around the eye or superficially to fill fine lines is often fraught with persistent lumps and bumps that are displeasing. RadiesseTM has become an effective filler in patients who fail fat; however, it should not be used in the more sensitive areas of the lips and lower lids.
The addition of hyaluronic acid-based fillers has been a significant improvement due to their increased longevity compared to collagen and their excellent safety profile; however, they are truly not cost effective at this point as a structural volume filler in areas such as the nasolabial folds or malar region. Lastly, the key to effective volume augmentation of the face is to differentiate between soft tissue atrophy or deflation versus gravitational changes and subsequent line development. One should not attempt to overcompensate for gravitational changes with volume augmentation.
Suggested Reading
1.Coleman SR. Facial recontouring with lipostructure. Clinics Plast Surg 1997; 24(2):347.
2.Kanchwala SK, Bucky LP. Facial fat grafting: The search for predictable results. Facial Plast Surg 2003; 19(1):137.
3.Billings Jr E, May Jr JW. Historical review and present status of free fat graft autotransplantation in plastic and reconstructive surgery. Plast Reconstr Surg 1989; 83(2):368.
4.Bergeret-Galley C. Comparison of resorbable soft tissue fillers. Aesthetic Surg J 2004; 24(1):33.
5.Narins RS, Brandt FS, Leyden J et al. A randomized, double-blind, multicenter comparison of the efficacy and tolerability of restylane versus zyplast for the correction of nasolabial folds. Dermatol Surg 2003; 29(6):588.
Chapter 74
Cosmetic Uses of Botulinum Toxin
Leonard Lu and Julius Few
Introduction
The use of botulinum toxin type A (Botox®) for facial aesthetic procedures has gained exponential popularity. In fact, more than 2.2 million Botox procedures were performed in 2003. The widespread use of Botox is attributed to its effectiveness in reducing facial rhytids and also to its short and long term safety record. It is important to note that Botox Cosmetic is currently approved by the FDA for the treatment of glabellar lines; however, its use continues to find new applications in dermatology and plastic surgery (for example, for hyperhidrosis).
Mechanism of Action
Botox is a neurotoxin derived from the bacteria, Clostridium botulinum. It blocks neuromuscular transmission through a three-step process. First, the toxin binds to presynaptic cholinergic motor nerve terminals. Next, the toxin is internalized into the nerve terminal by endocytosis, where it eventually enters the cytoplasm. Finally, Botox inhibits acetylcholine release by cleaving a cytoplasmic protein. The end result is that the muscle contraction is inhibited. However, Botox’s action is not permanent because collateral axonal sprouting establishes new neuromuscular junctions, restoring muscle function.
Storage and Reconstitution
Botox is supplied in a vial with 100 units (U) of dried neurotoxin complex. It can be stored at 2 to 8˚C for up to 24 months. The manufacturer recommends reconstitution of the toxin with 2.5 ml of 0.9% saline to yield a final concentration of 4.0 U/0.1 ml. Although the package insert states Botox should be used within 4 hours of reconstitution, studies have shown that at 4˚C, the drug can be stored up to 6 weeks without a decrease in efficacy. Although there are no special handling precautions when using Botox, it is important to note that alcohol neutralizes the toxin. Therefore, if the practitioner uses alcohol to prepare the skin, it should be allowed to dry before injection.
Injection Technique
Injections should be performed with a tuberculin or insulin syringe (30 or 32-gauge needle). The top of the vial can be removed to avoid dulling the needle when drawing Botox into the syringe. Topical anesthesia with ice or other agents may be beneficial to decrease pain associated with injections but is not necessary. In general, men require higher doses of Botox because of a greater muscle mass. Thicker skin, such as that found in Asians, may also require higher doses. With the exception of the perioral and periocular areas, injections should be made into the muscle
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.
