
Practical Plastic Surgery
.pdf
402 |
Practical Plastic Surgery |
muscle strain from the forces needed to close the interlabial gap. The treatment for this type of facial anomaly may be to reposition the maxilla superiorly, particularly in the posterior area.
Maxillary sagittal hyperplasia is extremely rare. Patients may complain of a small chin as well. Once again, this is most likely a case of pseudomicrogenia, where the chin appears relatively small due to the prominence of the maxilla in the sagittal plane. These patients will have a convex facial profile associated with maxillary protrusion and an acute nasolabial angle. This form of microgenia can be corrected with repositioning of the maxilla, after which a decision can be made on the need for an adjunct genioplasty.
Evaluation of the Mandible
After a thorough investigation to rule out any maxillary discrepancies, the next step is to evaluate the mandible. For a patient with mandibular hypoplasia with either gross malocclusion or severe hypoplasia (greater than 4 mm), a formal orthognathic work-up is necessary. The risks of advancing or augmenting a chin greater than 5-6 mm include an unnatural appearance, a deep labiomental angle, and the risk of advancing the chin point past the lower central incisor. Severe mandibular sagittal hypoplasia is corrected with a BSSO, and genioplasty should be viewed as an adjunct procedure. Prognathia in the setting of class 3 malocclusion should be corrected by a setback with a BSSO. Isolated true macrogenia in the presence of a normal class 1 occlusion can easily be treated with a genioplasty, setting the chin point back and even reducing chin height if needed.
Indications for Isolated Genioplasty
After careful scrutiny of the skeletal, dental and soft tissue structures, there exist certain cases that are amenable to isolated genioplasty. An isolated genioplasty can be considered if functional occlusion is present and the lower third profile has mild hypoplasia or hyperplasia in the sagittal or vertical plane. A sagittal hypoplasia (3-4 mm) in the setting of functional normo-occlusion with acceptable facial proportions is an ideal candidate for AHMO with advancement. A variation of the standard sliding genioplasty is the “jumping” genioplasty. The “jumping” genioplasty is ideal for sagittal advancement when vertical reduction is needed.
Patients who are considered for isolated genioplasty should have a good overall profile and occlusion. The surgical goals for these patients include creating an aesthetically pleasing facial contour and establishing proportionate facial height. Ideal candidates for a genioplasty are: (1) retrogenia, i.e., recessed chin point with class I occlusion; (2) mild retrognathia (≤4 mm) with a functional occlusion; and (3) macrogenia.
For example, in a patient that may have a long lower third of the face, a reduction genioplasty is performed to reduce the vertical dimension of the chin. Verti-
65cal reduction is done by performing a second horizontal osteotomy that is parallel to the first osteotomy, and a segment of bone is removed. Another indication for an isolated genioplasty may be a mild asymmetry, when the chin does not coincide with facial midline. An oblique triangular wedge of bone can be removed from one side and transplanted to the other side to correct chin asymmetry. In all cases, the chin has to be rigidly fixed by miniplates, wire or screws. A variety of genioplasty is the “jumping” genioplasty. This type of procedure allows the surgeon to both increase the chin projection and shorten the vertical dimension of

Genioplasty, Chin and Malar Augmentation |
403 |
the chin simultaneously. After the osteotomy is completed, the basilar segment is elevated on top of the upper symphysis.
Surgical Technique
Genioplasty can be performed under local anesthesia with IV sedation or under general anesthesia. General anesthesia is more commonly used with this procedure. Lidocaine with epinephrine is infiltrated along the depth of the buccal vestibule. An incision is made in the buccal vestibule, initially perpendicular to the mucosa then perpendicularly to the muscle and bone. The dissection is continued in the subperiosteal plane to identify the mental foramen on both sides. After identification of the mental foramen, the mental nerves should be protected from both direct and traction injury. The osteotomy is done under the apices of the teeth and the mental nerve. Upon completion of the osteotomy, the chin is then rigidly fixated. A step-off (sharp edge) at the posterior part of the genioplasty should be avoided. The contour of the mandible should be smooth. There are a variety of techniques used for fixation of the chin including wires, resorbable or titanium bone plates. Closure should be done in multiple layers. The mentalis muscle must be reapproximated. The muscle layer can also be reattached to the chin using Mitek anchors. We prefer using two Mitek anchors to secure the mentalis muscle to bone. Alternatively, simple reapproximation with two horizontal mattress sutures is acceptable. This prevents ptosis of the mentalis muscle. Nonfixation may result in a “witches chin.” A compressive chin dressing is worn for 5 days postoperatively. The oral mucosa is closed with a running 3-0 chromic suture. The advantage of this procedure is its versatility, reliability and reproducible correction of chin point discrepencies. The disadvantages, when compared to alloplastic augmentation, include increased operative time, bleeding and incidence of mental nerve hypoesthesia.
Chin Augmentation Using an Alloplastic Implant
An alternative to genioplasty in correcting chin hypoplasia is the use of a chin implant. The use of implantable biomaterials and devices plays a potential role in most forms of reconstructive surgery. The common locations for alloplastic augmentation are the chin and malar regions. There are numerous synthetic implantable materials that can be classified as carbon based polymers, noncarbon-based polymers, metals and ceramics. This wide selection allows the surgeon to choose a material tailored to the individual needs of the patient. Silicone (silastic), a noncarbon-based polymer, was one of the first materials used in facial implants. Silicone is resistant to degradation and when fixed against a bony surface its long term stability is very high. Carbon-based polymers include polytetrafluoroethylene (PTFE), polyethylene (PE) and aliphatic polyesters. PE is currently being used in its high density form (HDPE), which allows for contouring by the surgeon. The solid implantable form of HDPE (Medpor®) allows for increased fibrous ingrowth lead-
ing to long-term stabilization of the implant. 65 Alloplastic chin augmentation is a well-accepted technique used in the correc-
tion of mild retrognathia or true retrogenia. The advantages of alloplastic augmentation include the material being readily available without donor morbidity, shorter operating time and less blood loss. The disadvantages include bone resorption, infection, extrusion and displacement.
When an implant is used, either an intraoral or extraoral approach can be used. With the extraoral approach, the incision placement is in a natural crease location.

404 |
Practical Plastic Surgery |
The extraoral approach has a lower rate of infection although it is more difficult to achieve precise placement of the implant. The intraoral technique introduces oral flora into the pocket of dissection, increasing the risk of infection and extrusion.
Malar Augmentation
The malar prominences contribute to aesthetic balance and beauty. Deficiencies or asymmetry in the malar region are usually secondary to trauma, congenital anomalies, such as Treacher Collins syndrome, cancer, or aging. Malar augmentation can be used in either aesthetic or reconstructive practices to achieve symmetry and balance of the face. For example, patients that have undergone repair of a cleft lip and palate may require a LeFort I osteotomy to correct midface deficiency and malocclusion. Correction of the occlusion can be done with the LeFort I osteotomy. The concave profile can be enhanced by malar augmentation (or doing a high osteotomy) to help reestablish overall facial harmony and proportions. In the aging patient, the face may have a tired appearance due to resorption of the maxilla and descent of the malar fat over the zygoma. Malar augmentation may help to create a more youthful appearance.
Preoperative assessment of the deficient or asymmetric malar region is important prior to any augmentation. The facial skeleton can be analyzed using three-dimensional CT generated models from which custom-made implants can be fabricated. Any asymmetries found should be pointed out to the patient and documented. Malar augmentation can be done with autologous bone or with alloplastic implants.
Technique
A number of approaches have been described, including the lower eyelid, coronal, temple and preauricular incisions. However, the most popular approach is by an intraoral incision. This approach leaves no visible scar and allows the procedure to be performed under local anesthesia if desired. The intraoral approach is done through an upper buccal sulcus incision followed by subperiosteal dissection of a pocket in the malar region. It is important to identify the infraorbital nerve and protect it. The implant is contoured and placed after creation of an adequate pocket. It should remain “uncontaminated “during its placement in order to decrease the risk of infection. In the no touch technique, the implant does not come in contact with gloved hands, skin, or oral mucosa in hopes to decrease any bacterial contamination load. Finally, the implant should be secured with either screws, nonabsorbable sutures, or held in place by a tight pocket of periosteum.
Pearls and Pitfalls
Over the long-term, genioplasty is much more durable than alloplastic augmentation of the chin. At some point, most implants will require replacement due to malposition, extrusion, infection or overlying soft tissue changes. Osseous genio-
65 plasty, however, can last a lifetime. It is important to discuss this with the patient. When designing the proposed osteotomy for genioplasty, one has to pay particu-
lar attention to the apices of the teeth and the mental nerve. The intraoral approach provides a simple access without a visible scar. The mental foramen lies on the same vertical plane defined by the second bicuspid tooth, infraorbital foramen and pupil. The mental nerve should be dissected out, retracted superiorly and protected during the osteotomy. The three branches of the mental nerve exit the mental foramen and

Genioplasty, Chin and Malar Augmentation |
405 |
supply general sensation to the chin point. The osteotomy line should be about 3 mm below the mental canal to avoid the route of the inferior alveolar nerve.
Genioplasty by AHMO has also found a functional role in patients with obstructive sleep apnea. Advancement of the genioglossal muscle leads to indirect elevation of the hyoid, thus serving as an adjunct to bimaxillary surgery. A long distance (>15 mm) from the hyoid to the mandibular plane angle can contribute to a decrease in the posterior airway space. By advancing the genial tubercle and muscles, this will indirectly pull the hyoid closer to the mandibular plane and away from the posterior airway.
Suggested Reading
1.Chang EW, Lam SM, Karen M et al. Sliding genioplasty for correction of chin abnormalities. Arch Facial Plast Surg 2001; 3(1):8.
2.Constantinides MS, Galli SK, Miller PJ et al. Malar, submalar and midfacial implants. Facial Plast Surg 2000; 16(1):35.
3.Millard DR. Chin implants. Plast Reconstr Surg 1954; 13(1):70.
4.Spear SL, Kassan M. Genioplasty. Clin Plast Surg 1989; 16(4):695.
5.Spear SL, Mausner ME, Kawamoto Jr HK. Sliding genioplasty as a local anesthetic outpatient procedure: A prospective two-center trial. Plast Reconstr Surg 1987; 80(1):55.
6.Wolfe SA. Chin advancement as an aid in correction of deformities of the mental and submental regions. Plast Reconstr Surg 1981; 67:5.
7.Yaremchuk MJ. Facial skeletal reconstruction using porous polyethylene implants. Plast Reconstr Surg 2003; 111(6):1818.
65
Chapter 66
Augmentation Mammaplasty
Richard J. Brown and John Y.S. Kim
Introduction
Breast augmentation, also known as augmentation mammaplasty, is performed to balance a difference in breast size (developmental or involutional), to improve body contour, or for reconstruction after breast cancer resection. Clinical trials have shown that breast implants are a safe technique for breast augmentation. Attention to detail during patient evaluation and preoperative planning can significantly impact outcomes in breast augmentation. Women requesting the procedure are most commonly in their twenties or thirties. It is imperative to assess a patients’ motivation for seeking augmentation mammaplasty in an effort to avoid dissatisfaction after the procedure. The best candidates for surgery are women who are looking for improvement, not perfection, in physical appearance, and who understand that augmentation only enhances breast size and will not change their social situation.
Anatomy
The female breast is a modified integumentary and glandular structure. The dimensions vary depending on the patients’ body habitus and age. It covers the anterior chest wall from the second rib superiorly to the fourth or fifth rib inferiorly. The upper half overlies the pectoralis major muscle, the lower half overlies the serratus anterior, and part of the lateral breast overlies the axillary fascia. Blood supply to the breast is supplied via the internal mammary artery from the medial aspect, the lateral thoracic artery from the lateral aspect and the third through seventh intercostal perforating arteries. Deep venous drainage accompanies the arterial supply and superficial drainage arises from the subdermal plexus. Lymphatic drainage is primarily from the retromammary plexus located within the pectoral fascia. Sensory innervation is derived primarily from the intercostal nerves. Nipple sensation is derived from the third through fifth anterior cutaneous nerves and the fourth and fifth lateral cutaneous nerves. The anterior branch of the fourth lateral intercostal nerve provides the main sensation to the nipple-areolar complex.
Patient Selection
As with any elective surgery, certain severe systemic illnesses may preclude a patient from being considered an acceptable candidate for augmentation. Severe ptosis is a relative contraindication and may concomitantly require mastopexy. The one absolute contraindication to the subglandular placement of implant is in patients with a history of breast irradiation. Radiation impairs blood supply making the submuscular approach much safer. A strong family history of breast cancer is another relative contraindication to the subglandular approach because a small amount of breast tissue may be obscured during a mammogram when the implant is in the subglandular position. Relatively contraindicated is the patient with severe psychosocial issues, grossly unrealistic expectations, or body dysmorphic disorder.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

Augmentation Mammaplasty |
407 |
Preoperative Planning
History and Physical
The importance of the initial consultation cannot be overemphasized. Determining breast volume, selecting the type and shape of the implant, deciding on placement (subglandular or submuscular) and choosing the surgical approach should all be discussed. Evaluation of anatomic features is an essential element when planning augmentation. Noting asymmetry is important because the patient may be unaware of the problem. In such cases, the surgeon should explain that efforts to correct asymmetry will be attempted, but that perfectly symmetric results are unrealistic. Attempting to meet the patient’s expectations regarding size without compromising a natural appearance is very important. In young healthy patients, routine blood tests are not required. It is, however, important to rule out a personal or family history of clotting disorders. A urine pregnancy test should be performed in most cases.
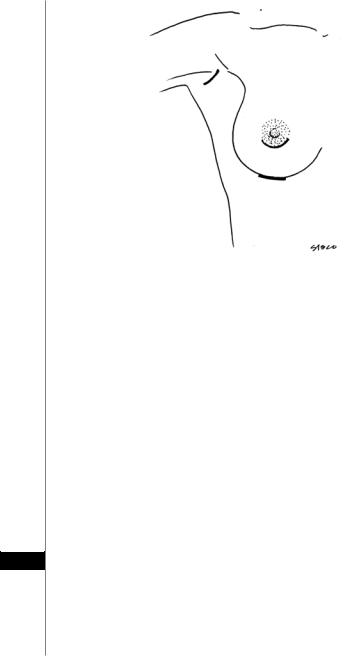
Choice of Incision
The trend in plastic surgery is to minimize scarring by remote placement of access incisions. The position of the incision is important and should be individualized since no single incision works best for all patients. Most surgeons have their own preference as to the surgical approach used in the procedure. In addition, most patients are knowledgeable about the various incisions and have their own preferences as well. The choice of incision should be discussed with the patient in a nonbiased manner highlighting pros and cons of each approach (Fig. 66.1). Currently, there are four commonly used types of incisions: periareolar, inframammary crease, axillary and umbilical. Some patients are candidates for an endoscopic transaxillary or inframammary approach; however results depend in part on the surgeon’s familiarity and experience with endoscopic techniques.
Type of Implant
Silicone gel-filled implants were the most common implants used prior to their removal from the market by the Food and Drug Administration (FDA) and are available only through FDA approved clinical trials. Currently, saline-filled implants are the type of implant most widely used. They can be classified as smooth or textured, round or contoured and as having a high or low profile.
Cancer Detection
It is important to educate patients about the potential long-term effects on breast cancer surveillance. A woman’s risk of developing breast cancer is not affected by breast implants, and to date there is no evidence to support a relationship between silicone or saline implants and breast cancer in humans. Slight modifications in mammographic technique (Eklund displacement technique) may be required for adequate visualization of all breast tissue. Capsular contracture has the greatest im-
pact on mammography. Severe contracture can reduce the accuracy of the mammo- 66 graphic findings. Current recommendations suggest women aged 30 or older should
have baseline and postaugmentation mammograms and should follow the same schedule of routine mammography as all other women. They should also perform monthly self-exams and become familiar with the new feel of their breast tissue. Self-exams are much more likely to detect a breast cancer in augmented patients compared to nonaugmented women.
408 |
Practical Plastic Surgery |
|
|
|
|
|
|
|
Figure 66.1. Commonly used incisions for breast augmentation.
Sensation
Breast and nipple sensation are usually compromised only temporarily (weeks to months) due to nerve stretching from aggressive lateral dissection. Accidental nerve division is uncommon. With the subglandular approach, the reported incidence of nerve injury is 10%, and even lower with the submuscular approach. The degree of sensation loss is directly proportional to the size and diameter of the implant due to the large pocket that must be dissected. Impaired breast sensation is more likely after secondary procedures, especially extensive capsulotomy which may subject sensory nerves to injury.
Pregnancy and Lactation
Many women seek breast augmentation prior to their childbearing years. Breast augmentation is extremely unlikely to impair lactation or breast-feeding, especially when implants are placed in the submuscular position. Many surgeons will advise patients to undergo breast augmentation a minimum of 6 months prior to pregnancy or at least 6 months after the termination of lactation. Breast appearance after childbirth varies in patients who have had augmentation prior to pregnancy. Some will return to their prepregnancy appearance while others do not.
66 Intraoperative Considerations
Inframammary Incision
This is the most common approach for placement of a breast implant. The incision is made just above the imframammary crease, and should be no more than 3-4 cm in length. The surgeon must estimate where the incision will sit in relation to the crease created by the larger enhanced breast. An incision placed too low may be obviously visible. The inframmary incision is a favorite among surgeons because it
Augmentation Mammaplasty |
409 |
|
|
gives complete visualization of the subpectoral plane and offers a great deal of con- |
|
||
|
|||
trol over placement of the implant. If the patient needs revision surgery in the fu- |
|
||
ture, this incision can be reused without the need to create a new scar. A potential |
|
||
problem with this incision occurs when patients decide to undergo an implant ex- |
|
||
change to a different size. This can cause migration of the inframammary fold, thus |
|
||
exposing the original scar. |
|
|
|
Periareolar Incision |
|
|
|
This approach involves an incision within the pigmented areolar tissue and often |
|
||
results in the least conspicuous scar. A medially placed incision avoids the fourth |
|
||
intercostals nerve, which supplies sensation to the nipple-areola complex. Dissection |
|
||
may be carried through the breast parenchyma or towards the imframammary fold |
|
||
subcutaneously around the lower pole of the breast. Since most breast ducts contain |
|
||
bacteria there is an increased risk of infection when dissecting through breast tissue. |
|
||
If a patient is undergoing simultaneous mastopexy, this is a favorable approach since |
|
||
the two procedures may share the same incision. This approach works well with every |
|
||
type of implant and for placement both above and below the pectoralis muscle. |
|
|
|
Transaxillary Incision |
|
|
|
The benefit of this approach is the inconspicuous scar. The incision is in the |
|
||
axilla, where it is only seen when raising the arm. This scar heals well with only |
|
||
slight discolorization, although there is a greater risk of forming a hypertrophic scar |
|
||
compared to incisions at the breast. The implant may be placed on, above or below |
|
||
the muscle with this technique. However, there are many disadvantages to the |
|
||
transaxillary incision. The main disadvantage with this approach is the poor expo- |
|
||
sure obtained during placement of the implant; however this can be improved using |
|
||
the endoscopic technique. It is difficult to create symmetric pockets so patience and |
|
||
skill are required. There is also an increased incidence of paresthesia to the |
|
||
nipple-areolar complex with this approach. Another downside to this incision is in |
|
||
the event of a complication or the need for future corrective surgery, removal of the |
|
||
implant would require conversion to one of the previously discussed incisions. Other |
|
||
potential complications that have been reported are damage to the intercostobra- |
|
||
chial nerve and subclavian venous thrombosis. |
|
|
|
Periumbilical Incison |
|
|
|
Placement of the implant using this approach is restricted to a prepectoral plane, |
|
||
and this approach provides the worst control for dissection of the pockets. Dissection of |
|
||
the superior pole and symmetry of placement are difficult even in the most experienced |
|
||
hands. Complications of hematoma or infection require conversion to one of the previ- |
|
||
ously discussed incisions. The periumbilical approach is the least utilized technique. |
|
||
Location of the Implant Pocket |
|
|
|
Implants are commonly placed in the submuscular position, the subglandular |
|
||
66 |
|||
position, or in a position that combines the two, termed the biplanar approach. In |
|
||
|
|||
the submuscular technique, the implant is placed in a plane below the pectoralis |
|
||
major muscle, whereas in the subglandular approach the implant is deep to the |
|
||
glandular breast tissue but superficial to the muscle. Advantages to submuscular |
|
||
placement include a decreased rate of capsular contracture, and reduced sensory |
|
||
changes in the nipple. In addition, with this technique there is a decreased incidence |
|
||
of hematoma formation since the plane below the muscle is relatively avascular. |
|
||
|
410 |
Practical Plastic Surgery |
||
|
|
Disadvantages to this approach include limitations on the size of the pocket that can |
||
|
|
|||
|
|
be dissected, increased postoperative pain, potential lateral displacement of the im- |
||
|
|
plant and the inability to obtain significant medial fullness, or cleavage. Releasing |
||
|
|
the inferior portion of the pectoralis muscle from its medial sternal attachments can |
||
|
|
help improve cleavage appearance. Advantages to the subglandular approach in- |
||
|
|
clude ease of dissection, the ability to use larger implants and a more predictable size |
||
|
|
and contour. Furthermore, breast ptosis may be better addressed with subglandular |
||
|
|
placement. Disadvantages include an increased risk of capsular contracture, higher |
||
|
|
risk of nerve injury, abnormal contour appearances such as rippling and a greater |
||
|
|
risk of rupture during a future breast biopsy. |
|
|
|
|
Postoperative Considerations |
|
|
|
|
For the first few hours while in the recovery room, the patient’s incisions and |
||
|
|
breasts should be examined for evidence of hematoma. Oral narcotics are given for |
||
|
|
postoperative pain, and the patient should refrain from vigorous activity for the first |
||
|
|
48 hours. A soft elastic bra may be worn after the operation for comfort, support |
||
|
|
and molding of the breast, but is not required. At the first postoperative visit, the |
||
|
|
patient is encouraged to begin massaging her breasts daily. Movement of the im- |
||
|
|
plant against the walls of its cavity helps maintain an expanded capsule and result in |
||
|
|
a softer breast. If used, patients are instructed to remove Steri-strips about two weeks |
||
|
|
postoperatively. At that time, unrestricted activity may commence. |
||
|
|
Complications |
|
|
|
|
Hematoma |
|
|
|
|
One to two weeks prior to surgery patients should discontinue medications that |
||
|
|
may impair platelet activity. The frequency of hematoma formation is less than 2%. The |
||
|
|
best prevention is operative technique utilizing blunt dissection and meticulous hemo- |
||
|
|
stasis. A hematoma may form slowly with no symptoms or rapidly with symptoms such |
||
|
|
as unilateral pain, swelling and fever. Immediate postoperative hematomas should be |
||
|
|
taken back to the operating room for evacuation. Late-onset hematomas that are symp- |
||
|
|
tomatic should be drained due to the risk of infection and capsular contracture. |
||
|
|
Sensory Changes |
|
|
|
|
The incidence of diminished sensation in the nipple is 15%. Most patients expe- |
||
|
|
rience temporary dysesthesia of the nipple that often resolves within several months. |
||
|
|
A small percentage of patients may experience long-term sensory loss in one or both |
||
|
|
nipples, a complication that is most common with the transaxillary approach. Avoid- |
||
|
|
ance of extensive lateral pocket dissection and use of the the submuscular position |
||
|
|
will decrease nerve injury. |
|
|
|
|
Infection or Seroma |
|
|
|
|
The incidence of infection is about 2% and usually manifests 7-10 days postop- |
||
66 |
||||
|
eratively, but may occur at any time. Either the wound or the periprosthetic space |
|||
|
||||
|
|
may be involved. Symptoms include fever, swelling, discomfort, pain, drainage and |
||
|
|
cellulitis of the breast. The two most common organisms are Staphylococcus epidermidis |
||
|
|
or Staphylococcus aureus. Uncomplicated wound infections should be treated with a |
||
|
|
course of antibiotics for 1-2 weeks. Wounds draining pus should be opened, and the |
||
|
|
implant will often need to be removed. If seroma fluid is clinically present, |
||
|
|
ultrasound-guided aspiration with culture and sensitivity should be performed. Posi- |
||

Augmentation Mammaplasty |
411 |
|
|
|
|
Table 66.1. The Baker classification of capsular firmness in |
||||
|
augmented breasts |
|||
|
|
|
|
|
Grade I |
No palpable capsule |
The augmented breast feels as soft as an |
||
|
|
unoperated one |
||
Grade II |
Minimal firmness |
The breast is less soft and the implant can be |
||
|
|
palpated, but is not visible |
||
Grade III |
Moderate firmness |
The breast is harder, the implant can be |
||
|
|
palpated easily, and it can be seen |
||
Grade IV |
Severe contracture |
The breast is hard, tender, painful and cold. |
||
|
|
Distortion is often marked |
|
|
tive culture results should prompt appropriate antibiotic therapy and consideration |
||||
of implant removal. If cultures are negative, seromas may be followed clinically. If |
||||
they do not resolve, then patients should be presented with management alterna- |
||||
tives, including repeat aspiration or implant removal. It is important to remember |
||||
that infection and seroma are both risk factors for subsequent capsular contracture. |
||||
Capsular Contracture |
|
|
|
|
Capsular contracture is the most common cause of dissatisfaction after breast aug- |
||||
mentation. It occurs due to the formation of a fibrous scar that may become thick and |
||||
constrict a soft implant (Table 66.1). Etiology is unknown, but the two main theories |
||||
are hypertrophic scar formation or infection-induced contracture. Saline-filled im- |
||||
plants have a lower incidence of contracture compared to silicone-filled implants. Tex- |
||||
tured surface saline implants have a lower rate of contracture when placed in the |
||||
subglandular position provided the patient has adequate tissue for coverage, while |
||||
smooth surface saline implants have a lower rate of contracture in the subpectoral |
||||
position. Steps to help minimize the risk of contracture include meticulous hemostasis |
||||
and sterile technique. The implant should be soaked in antibiotic irrigation solution |
||||
and handled as little as possible. In addition, creating an adequately sized pocket is |
||||
important. The implant should fit into the pocket without being tight or firm, allow- |
||||
ing mobility during postoperative massage exercises. |
||||
Treatment options include closed or open capsulotomy and capsulectomy. The |
||||
goal of closed capsulotomy is to rupture the scar capsule by manually squeezing the |
||||
breast until there is an audible pop without fracturing the implant. Complications |
||||
such as hematoma, rupture of the implant and migration make this an unfavorable |
||||
procedure. Open capsulotomy is best when capsular contracture is less severe, and |
||||
involves stripping or scoring of the capsule. Capsulectomy, or complete capsule re- |
||||
moval, should be reserved for a firm, thick, calcified capsule. Implants may be re- |
||||
placed and repositioned if necessary with open capsulotomy or capsulectomy. The |
||||
patient may also choose to remove the implants without replacement. |
||||
Implant Displacement |
|
|
66 |
|
|
|
|
||
Asymmetry and displacement are the second most common causes of dissatis- |
||||
faction after breast augmentation. Implants can be placed too high, too low or ex- |
||||
cessively lateral. Displacement may also rarely occur after a capsulotomy procedure. |
||||
Displacement can occasionally be treated conservatively with prolonged taping and |
||||
closed manipulation. More commonly, however, persistent dissatisfaction with dis- |
||||
placement usually culminates in surgical revision. |
||||
