
Practical Plastic Surgery
.pdf
72 |
Practical Plastic Surgery |
|
|
|
|
Table 15.1. Normal bacterial skin flora
Bacteria
Staphylococcus
Micrococcus
Peptococcus
Corynebacterium
Brevibacterium
Propionibacterium
Streptococcus
Neisseria
Acinetobacter
but also the local bacterial flora that is present on intact skin. These wounds occur in the setting of various pathologies and are usually chronic in nature before being brought to the attention of a plastic surgeon. Unlike most surgical incisions, these wounds heal by secondary intention and are always colonized by bacteria. They require extensive granulation tissue formation and keratinocyte migration for closure, involving endothelial cells and fibroblasts for the purposes of neovascularization and matrix production, respectively. For this to occur, macrophages and a varying
15milieu of growth factors must be present. Along with neutrophils, macrophages also act to disinfect the wound, killing foreign organisms by the generation of peroxide and superoxide radicals. The clinical spectrum of bacterial invasion exists on a continuum from least to most severe: contamination, colonization, local infection or critical contamination, invasive infection and sepsis.
•Contaminated wounds have nonreplicating organisms within their borders. These wounds will go on to heal normally.
•Colonized wounds have replicating bacteria, but these bacteria are nondestructive and contained within the wound. A hallmark of colonization is that it does not delay the wound healing process.
•Local infection or critical contamination is an intermediate level of bacterial invasion characterized by granulation tissue that has an unhealthy appearance, and wound healing that may be delayed. In this type of wound, however, tissue invasion is not present. This stage is notable for the absence of other signs of infection such as cellulitis or pus formation.
•Invasive infection occurs once bacteria have invaded through the wound bed, tissue destruction has begun, and an aggressive immune response is present. Signs and symptoms of invasive infection include pain, edema, erythema and fever. The finding of a chronic, nonhealing wound, often with pus formation and tissue necrosis is often evident.
•Sepsis occurs when the infection spread systemically, and cardiovascular instability and organ-system dysfunction develop.
The Molecular Biology of Bacterial Infection
Low levels of bacteria in wounds actually help to promote wound healing by stimulating brisk monocyte and macrophage activity. However, as their number or virulence increases, the tissue response to their presence disrupts and prolongs the inflammatory phase of wound healing, depletes the components of the complement cascade, interferes with normal clotting mechanisms, and alters leukocyte function. The level of pro-inflammatory cytokines, including interleukin-1 and
The Chronic Infected Wound and Surgical Site Infections |
73 |
tumor necrosis factor-alpha, rises and stays elevated. Elevated levels of matrix metalloproteinases and a lack of their inhibitors lead to tissue breakdown and growth factor inhibition. Bacteria also compete with local cells for oxygen, reducing its availability to these cells and stimulating an angiogenic response, leading to friable granulation tissue that is prone to bleeding.
Bacteria in Wounds
Classic teaching is that wounds with greater than 105 organisms/gram should be considered infected whereas those with a lower bacterial count should not. Although studies do show that wounds with bacterial counts higher than this heal more slowly and have a higher rate of infection, a more practical approach to diagnosing the infected wound is encouraged. As wounds mature, not only do the species of organisms present in the wound change, the wounds begin to carry a higher level of bioburden, meaning a higher baseline number of colonies without being infected. Conversely, the more virulent bacteria, such as beta-hemolytic streptococcus and some rare Clostridium species, can easily cause infection at lower quantitative levels than the more commonly occurring species (Table 15.2). Finally, the status of the patient’s immune response has a role in the patient’s likelihood of developing an infected wound. Therefore, the surgeon is encouraged to study the appearance of the wound and the overall clinical picture when deciding whether a wound is infected.
Although it is important to note the classic signs and symptoms of infection 15 including erythema, edema, fever and an elevated white blood cell count, recent studies attempting to establish evidence-based criteria for the determination of a chronic wound infection have shown that increasing pain, friable granulation tissue,
foul odor and wound breakdown are the most sensitive indicators.
Bacteria in chronic wounds often establish a biofilm. This is an extracellular, polysaccharide-rich matrix in which the organisms are embedded. Within this glycocalyx is a system of channels, like a primordial circulatory system, that allows the bacteria to remain viable with less direct dependence on the host tissue. Cells in this environment become more sessile and less metabolically active. As a result, they are resistant to host immune responses and antibiotic therapy. Biofilms often coat foreign and implanted material, making infections in this setting more difficult to treat, and certain bacteria such as Pseudomonas aeruginosa have a predilection to biofilm production.
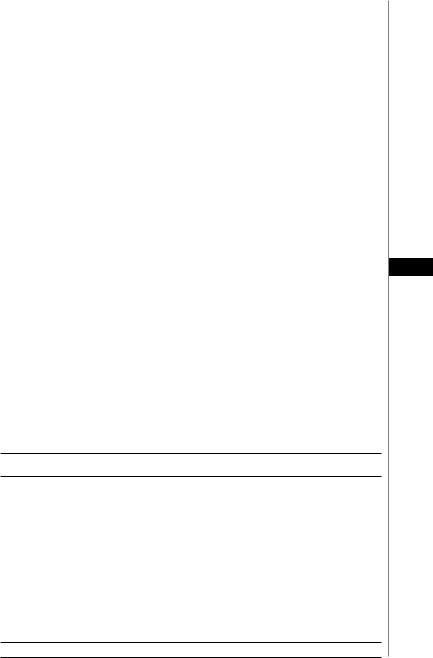
Table 15.2. Bacteria commonly infecting chronic wounds
Bacteria |
Occurrence (%) |
Staphylococcus aureus |
20 |
Coagulase-negative staphylococci |
14 |
Enterococci |
12 |
Escherichia coli |
8 |
Pseudomonas auruginosa |
8 |
Enterobacter species |
7 |
Proteus mirabilis |
3 |
Klebsiella pneumonia |
3 |
Other streptococci |
3 |
Candida albicans |
3 |
Group D streptococci |
2 |
Reproduced with permission from: Barie PS. Surgical Infections 2002; 3:S-9.

74 |
Practical Plastic Surgery |
Clinical Evaluation
A thorough history includes information related to the chronicity of the wound, any changes to the wound appearance, and details that should make the clinician suspicious of a more invasive bacterial involvement (e.g., pain, fever). Mitigating factors such as comorbid conditions that could lead to immunosuppression, the use of any immunosuppressive medications, previous radiation in the wound area and the overall functional status of the patient are important to explore. In addition to a white blood cell count and blood cultures, laboratory tests can include the erythrocyte sedimentation rate and C-reactive protein. Although not specific, in a patient with no recent history of surgery or acute illness, their value is in helping to determine the level of systemic response to a wound and in helping to determine the presence of a deep wound infection.
When examining a wound, its depth and width should be measured and a careful inspection and probing should be done. Attention to findings such as erythema at least 5 mm beyond the wound edges, expressed pus, necrotic debris or granulation tissue that is dark, friable or heaped above the wound edges can help to determine the extent of infection. Foreign bodies such as old strands of gauze should be removed and the presence of underlying foreign material such as sutures or mesh should be ruled out. Care must be taken to ensure that wounds overlying osseous
15structures do not have any exposed bone at their base that would suggest the presence of osteomyelitis.
As stated earlier, bacterial cultures can help to make a diagnosis and guide appropriate therapy. In a wound that has been appropriately cleaned and prepared, a swab of the deeper tissue can give a qualitative notion of which bacteria are present. It does not, however, allow the clinician to quantitate the amount of bacteria within the wound. For this, the gold standard is a biopsy culture. A punch biopsy is taken and ground into a liquid state from which serial dilutions are cultured. A measure of colonies per milligram can then be reported.
Treatment
Antibiotics are ineffective in penetrating chronic, nonhealing wounds. Debridement is the best option for clearing bacterial loads and removing nonviable tissue. If not performed, necrotic material can release endotoxins that inhibit keratinocyte migration and matrix production, and can prolong the inflammatory response, promoting matrix-destroying proteases.
Methods of debridement include sharp, mechanical, chemical and biodebridement.
Sharp, or surgical debridement affords the luxury of speed, since it can be performed at the bedside with nothing more than scissors and a pair of forceps. More extensive debridement may require anesthesia, and should be performed in the operating room.
Mechanical debridement is the eradication of dead tissue by the sequential changes of dressings that are inserted moist into the wound and removed after they are allowed to dry. Exudative and necrotic tissues adhere to the drying gauze and are pulled out of the wound with the gauze. This technique has only a limited ability to remove structurally intact or strongly adherent devitalized tissue. The classic “wet-to-dry” dressing is a mechanically debriding dressing.
Chemical debriding agents are enzymatic compounds that break down tissue. They are most effective in moderately sized areas of necrosis or in those patients that

The Chronic Infected Wound and Surgical Site Infections |
75 |
will not tolerate an operation. In order to gain maximum benefit, larger eschars should be cross-hatched or excised to allow for better penetration of the agent. The papain-containing cream, Accuzyme®, is commonly used for this purpose.
Biodebridement involves the application of sterile maggots into a wound for periods of 48-72 hours. The maggots feed on, and thus remove dead tissue before being irrigated out. This process can be repeated as necessary. Needless to say, it is not a commonly used technique.
Antibiotics do have a role in the treatment of chronic, infected wounds once debridement has achieved healthy wound borders. Empiric antibiotics should be selected based on the bacteria that are likely to be involved. For example, empiric antibiotics for wounds near the oropharynx and diabetic foot wounds should include coverage for anaerobic species. The Gram stain can give a general idea of whether Gram-positive, Gram-negative or a combination of bacteria is present. Once culture results return over the subsequent 2-3 days, antibiotic coverage should be tailored to the involved organisms. Topical antibiotic preparations can help to reduce bacterial load and can be used with some success in an adjuvant setting in the select wound population. Prudence should be taken with their use, however, because many of these preparations also impair the function of the superficial cells necessary for wound healing. They should never be used in wounds related to venous disease, as these wounds are more prone to sensitivity reactions. Examples include:
iodine or iodophor paint, sodium hypochlorite solution, hydrogen peroxide, acetic 15 acid, antibiotic creams or the newer cadhexomer iodine and nanocrystalline silver.
For wounds that arise in the setting of underlying pathology, treating the disease process can increase the speed and likelihood of wound healing. For venous stasis ulcers, reducing edema fluid with Unna boot compression, elevation and diuresis can improve oxygen delivery and thus cellular function. Patients with diabetic foot ulcers should have their blood sugar strictly controlled given the deleterious effects of hyperglycemia on neutrophil and monocyte function. If ischemia is believed to be contributing to the etiology or chronicity of a wound, smoking cessation and elimination of dehydration and anemia should all be considered in the treatment plan. Ultimately arterial revascularization with or without surgical reconstruction using local or microvascular flaps may be necessary.
Hidradenitis Suppurativa
This condition is due to infection of the apocrine sweat glands, most commonly in the axillary, perineal and groin regions. It results in recurrent, draining abscesses and sinus tracts that can lead to severe pain and debilitation. Lesions in the axilla that heal may scar and secondarily cause contracture limiting arm motion. Active infection should be treated with a 1-2 week course of oral antibiotics and is usually due to Gam positive cocci. Cultures should always be taken since other bacterial infections can occur, and the antibiotic should be appropriately selected.
Surgical treatment consists of full-thickness excision of the infected dermis and any involved subcutaneous fat. Primary closure can be obtained in smallto moderate-sized wounds without active infection. Larger defects, or those that are grossly infected, should not be closed primarily. They should be allowed to granulate with dressing changes, followed by split-thickness skin grafting or healing by secondary intention. Incomplete excision of the involved tissue is common due to retained sinus tracts or deep infected glands. When this occurs, there is a high likelihood of recurrence and skin graft failure.

76 |
Practical Plastic Surgery |
Surgical Site Infections
Definitions
Overall, surgical site infections (SSIs) are the leading cause of nosocomial infections, accounting for 38% of these complications. By definition, to be an SSI, an infection must occur within 30 days of the operation. SSIs can be broken down into three general categories. Superficial incisional SSIs involve only the skin or subcutaneous tissue of the incision. Signs and symptoms of this type of infection may include pain, swelling, redness, warmth and tenderness. Deep incisional SSIs demonstrate either purulent drainage from deeper tissue, a deep incisional dehiscence, or an abscess in the depth of the incision. Lastly, organ or deep space SSIs involve infections in manipulated regions other than the skin and subcutaneous tissue that was opened during the procedure. By definition, these infections must contain purulent drainage, positive cultures with fluid aspiration or documentation of the presence of an abscess. If a foreign body such as mesh or titanium was left in the wound an SSI can occur up to one year postoperatively.
Risk Factors
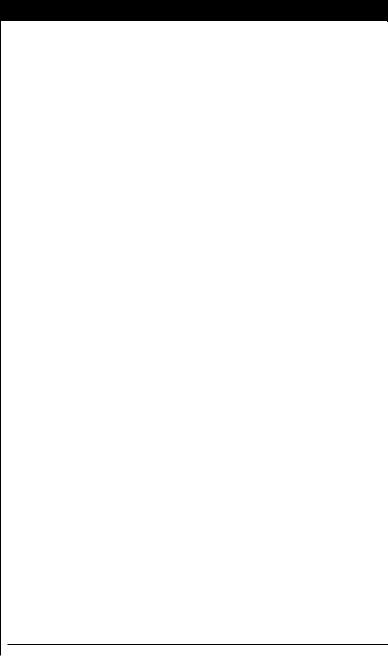
Generally speaking, the overall well being and the severity of any comorbid conditions determine how susceptible a patient is to wound infections (Table 15.3). The
15American Society of Anesthesiology rates patients’ operative risk according to their level of illness and comorbidities, termed the ASA class. There is a close correlation between the severity of the preoperative risk and the risk of wound infection. Furthermore, greater operative time is also associated with an increased risk of developing an SSI.
When planning an operation, the surgeon must consider the level of expected contamination. Clean surgical procedures are those that involve only skin and the musculoskeletal soft tissue and carry approximately a 2% chance of developing an SSI (although it must be noted that wound infection rates are probably underreported). Clean-contaminated procedures are those that involve the planned opening of a hollow viscus (e.g., the respiratory, biliary or gastrointestinal tracts) and have a 7-15% risk of becoming infected. Contaminated procedures are those that introduce nonsterile, bacteria-rich contents into the wound for a short period of time (e.g., penetrating abdominal trauma, unplanned enterotomies) and lead to SSIs in 20% of cases. Dirty procedures take place in an infected setting (e.g., bowel resection for an abscess related to Crohn’s disease, removal of infected prosthesis). Approximately 20-40% of these wounds will become infected if closed primarily.
Bacteria and Prophylaxis
Whereas most SSI are caused by skin derived Gram-positive cocci, including Staphylococcus aureus, coagulase-negative staphylococci such as Staphylococcus epidermidis and Enterococcus species, site-specific pathogens, may infect wounds. Consideration for Gram-negative bacilli should be given to any wound that is located near the site of bowel injury or repair, and when either bowel or tracheopharyngeal structures are violated, both enteric aerobic bacteria such as Escherichia coli and anaerobic bacteria such as Bacteroides fragilis may be of concern.
Prophylaxis for clean surgery is controversial. It is generally accepted that when bone is violated (e.g., during cranial vault reconstruction) or when a prosthesis is inserted, preoperative antibiotics are indicated. Less convincing data exists for straightforward soft tissue surgery (e.g., scar revisions).

The Chronic Infected Wound and Surgical Site Infections |
77 |
|
|
|
|
Table 15.3. Risk factors for the development of a surgical site infection (SSI)
Patient factors |
Anemia (postoperative) |
|
|
|
Ascites |
|
|
|
Chronic inflammation |
|
|
|
Corticosteroid therapy (controversial) |
|
|
|
Obesity |
|
|
|
Diabetes |
|
|
|
Extremes of age |
|
|
|
History of irradiation |
|
|
|
Hypocholesterolemia |
|
|
|
Hypoxemia |
|
|
|
Malnutrition |
|
|
|
Peripheral vascular disease |
|
|
|
Recent operation |
|
|
|
Remote infection |
|
|
|
Skin carriage of staphylococci |
|
|
Environmental factors |
Skin disease in the area of infection (e.g., psoriasis) |
|
|
Contaminated medications |
15 |
||
|
Inadequate disinfection/sterilization |
|
|
|
Inadequate skin antisepsis |
|
|
Treatment factor |
Inadequate tissue oxygenation |
|
|
Drains |
|
||
|
Emergency procedure |
|
|
|
Hypothermia |
|
|
|
Inadequate antibiotic prophylaxis |
|
|
|
Prolonged preoperative hospitalization |
|
|
|
Prolonged operative time |
|
|
When choosing an antibiotic agent, the following factors should be considered:
•It should have minimal side-effects and be safe for the patient.
•It should have a narrow spectrum of coverage for the expected organisms.
•It should not be overused (making it less likely that bacteria have developed resistance).
•It should cover typical infections that are specific for the institution.
•It can be used for a brief period of time (less than 24 hours).
Long prophylactic courses have been associated with an increased risk of nosocomial infections and multi-drug resistance. For clean and most clean-contaminated cases, a first-generation cephalosporin should be used. If a patient has a documented penicillin allergy, clindamycin is an alternative. Only in the setting of a hospitalized patient in an institution that carries a high rate of methicillin-resistant S. aureus (MRSA), should vancomycin be considered for prophylaxis.
It is important to recall that the timing of the antibiotic dose determines its effectiveness. Preoperative prophylaxis should be closed within two hours of incision time. Given too early, the antibiotic can be cleared before the case is started. Some benefit can be gained from intraoperative dosing if antibiotics are not given before the case begins, but no benefit has been shown when the first dose is given

78 |
Practical Plastic Surgery |
after the case ends. This loss of benefit after skin closure is related to the fact that sutured wounds exist in a low blood flow state owing to vasoconstriction, the use of electrocauterization for hemostasis, and the constrictive effects of the suture closure. Therefore, antibiotics will not reach the surgical site. In extremely lengthy cases, redosing intraoperatively is recommended.
Prevention and Treatment
In the weeks to months before a planned operation, much can be done to maximize the immune state and wound healing capabilities of the patient. Smokers should be encouraged to stop at least one month prior to their surgery. Smoking is a known vasoconstrictor that can reduce oxygen delivery to wounded tissue, and its effects have been found to last weeks beyond the point of smoking cessation.
The nutritional status of the patient should be taken into consideration as well. Obese patients should be encouraged to lose as much weight as possible while maintaining a healthy, protein-rich diet, and in the malnourished hospitalized patient, even a short 5-7 day course of parenteral or enteral nutrition has been shown to significantly reduce the risk of SSIs.
Studies show that having a patient take a preoperative shower with an antiseptic soap (e.g., hexachlorophene) can reduce skin bacterial load. However, shaving the planned surgical site with a razor either the night before surgery or immediately
15preoperatively should be discouraged due to the transient bacterial infestation that it promotes. Studies report greater than a 3-fold increase in infection rates with shaving versus hair clipping (5.6 vs. 1.7%). Finally, known S. aureus carriers should have their nasal orifices treated with topical 2% mupirocin.
Intraoperatively, care should be taken to keep the patient warm and well hydrated. This will improve blood flow to the wound and maximize oxygen delivery. Even 30 minutes of preoperative warming can reduce patient risk for SSI by two-thirds in some cases. Adequate oxygenation is important for cellular function and bacterial destruction via superoxide and peroxide formation. Case length should be kept to a minimum, given the fact that infection rates almost double for each hour an operation lasts. Tissues should be handled gently and electrocautery for hemostasis should be kept to a minimum. During the case, wounds should be kept moist and retractors should be released periodically to restore blood flow. The smallest possible suture diameter should be used to minimize foreign material in the wound (studies show that on average, surgeons use sutures one size larger than needed), and the prudent use of drains should be encouraged. By acting as a conduit for bacterial invasion and preventing epithelial closure of wounds, drains probably cause more SSIs than they prevent and they should be removed as soon as possible. Antibiotic prophylaxis of an indwelling drain is never indicated. High pressure pulse irrigation and topical antiseptic washes have been proven to be of some benefit in the contaminated or dirty wound. Both during the case and postoperatively, blood glucose concentration should be kept under tight control (80-110 mg/dl). And finally, postoperative nutrition should be optimized.
Controversy exists on whether it is appropriate to close contaminated wounds primarily. Studies in adults show that this practice can lead to a higher rate of wound failure and a greater cost of care. It is recommended that a delayed primary closure of the incision be used. This involves either placing untied sutures during the case that can later be cinched down, or using adhesive strips for closure when the wound is ready. Until the time when the wound appears to have minimal debris and no

The Chronic Infected Wound and Surgical Site Infections |
79 |
apparent progressing erythema, wet-to-dry, twice daily packing should be used (usually for 4-5 days).
Pearls and Pitfalls
Antibiotic prophylaxis of clean surgical procedures (e.g., elective operations on skin and soft tissue) is controversial based on a single randomized trial that showed benefit in breast and groin hernia surgery. The controversy persists because the incidence of superficial surgical site infection was so high (4%, versus an expected incidence of about 1%) in the placebo group. Evidence that antibiotic prophylaxis is indicated for soft tissue procedures of other types is lacking entirely, and prophylaxis cannot be recommended. If administered, antibiotic prophylaxis should be given before the skin incision is made, and only as a single dose. Additional doses are not beneficial because surgical hemostasis renders wound edges ischemic by definition until neovascularization occurs, and antibiotics cannot reach the edges of the incision for at least the first 24 hours. Not only is there lack of benefit, prolonged antibiotic prophylaxis actually increases the risk of postoperative infection.
Increasingly in the practice of plastic surgery, there is a tendency to leave closed-suction drains in place for prolonged periods in the erroneous belief that the incidence of wound complications is reduced by prolonged drainage. Nothing could be further from the truth. Data indicate that the presence of a drain for more than
24 hours increases the risk of postoperative surgical site infection with MRSA. Closed 15 suction drains must be removed as soon as possible, ideally within 24 hours. Prolonged antibiotic prophylaxis is often administered to “cover” a drain left in place
for a prolonged period. This is a prime example of error compounding error, and is a practice that must be abandoned.
Suggested Reading
1.Barie PS. Surgical site infections: Epidemiology and prevention. Surg Infect 2002; 3:S-9.
2.Bratzler DW. Antimicrobial prophylaxis for surgery: An advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis 2004; 38:1706.
3.Classen DC, Evans RS, Pestotnik SL et al. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 1992; 326:281.
4.Edwards R, Harding KG. Bacteria and wound healing. Curr Opinion Infect Dis 2004; 17:91.
5.Hunt TK, Hopf HW. Wound healing and wound infection: What surgeons and anesthesiologists can do. Surg Clin N Am 1997; 77:587.
6.Nichols RL. Surgical wound infection. Am J Med 1991; 91:3B.
7.Platt R, Zaleznik DF, Hopkins CC et al. Perioperative antibiotic prophylaxis for herniorrhaphy and breast surgery. N Engl J Med 1990; 322:153.
8.Schultz GS, Sibbald RG, Falanga V et al. Wound bed preparation: Systematic approach to wound management. Wound Rep Regen 2003; 11:S1.
9.Wysocki AB. Evaluating and managing open skin wounds: Colonization versus infection. AACN Clinical Issues 2002; 13:382.
Chapter 16
Diabetic Wounds
Roberto L. Flores and Michael S. Margiotta
Epidemiology
Diabetes is currently one of the most common diseases in the United States with approximately 800,000 new cases diagnosed annually. This number is expected to increase with the growing incidence of obesity in this country, particularly among the young. Diabetes is the seventh leading cause of death in the United States with an annual health care cost at several billion dollars. For patients with diabetes, foot disease is the most common cause of hospitalization and up to one in five are expected to develop foot ulceration within their lifetime. Additionally, the relative risk of lower extremity amputation is 40 times greater in diabetics. The strongest risk factor for lower limb loss, diabetes accounts for half of all lower extremity amputations in the United States. Of diabetics undergoing amputation, 50% are expected to have another amputation within five years.
The reconstructive plastic surgeon should be well versed in the pathophysiology, evaluation and treatment of the diabetic foot. Our role in treatment is to protect the limb by optimizing wound healing and providing soft tissue coverage to exposed bone, tendon, muscle and nerve, with the goal of delaying or averting amputation.
Pathophysiology
The pathogenesis of diabetic foot ulcers is due to the combined effects of ischemia, neuropathy and infection.
Ischemia
Both macrovascular and microvascular circulation are impaired by diabetes. Macrovascular occlusive disease secondary to atherosclerosis is well characterized among diabetics. The relative risk of developing peripheral arterial disease is 2 to 3 times higher in diabetic versus nondiabetic patients. Additionally, diabetics tend to have a faster progression of disease from intermittent claudication to limb-threatening ischemia compared with their nondiabetic counterparts. The cause of the accelerated atherosclerosis observed in diabetics is likely a result of dyslipidemia, enhanced platelet adhesiveness and endothelial injury/dysfunction. The spatial pattern of large vessel disease also differs between the two groups. In the lower extremity, nondiabetics tend to have proximal disease, which affects the superficial femoral and popliteal arteries. Diabetics tend to have distal disease affecting the tibial and peroneal arteries, with the superficial femoral and proximal popliteal vessels spared from advanced disease. The arteries of the foot, especially the dorsalis pedis, are typically affected to a lesser degree, allowing for extreme distal bypass reconstruction in select patients.
Microvascular disease involves a nonocclusive microcirculatory impairment, characteristically affecting the capillaries and arterioles of the kidneys, retina and peripheral nerves. The sequelae of this process results in the characteristic complications of
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

Diabetic Wounds |
81 |
nephropathy, retinopathy and neuropathy commonly seen in diabetic patients. Microcirculatory disease may also impair wound healing and increase susceptibility to wound infection. The physiologic mechanisms underlying microcirculatory disease have not been fully elucidated. Nonenzymatic glycosylation of the capillary basement membrane, seen in diabetics, may increase vascular permeability, leading to protein transudation and local edema. The well-characterized thickening of the capillary basement membrane is thought to impair migration of leukocytes to diseased areas.
Neuropathy
Peripheral neuropathy, a common complication in diabetics, poses a lifetime risk approaching 60%, and is seen in up to 80% of patients presenting with foot disease. The disease process includes sensory, motor and autonomic neural dysfunction. The pathogenesis remains to be fully elucidated, but the mechanism is likely due to both metabolic and microvascular defects. Diabetic neuropathy affects all nerve fibers with a predilection to the longest and finest fibers, leaving the nerves innervating the distal lower extremity most susceptible. Neuropathic disease characteristically affects the lower legs symmetrically, with a distal to proximal progression.
Sensory nerve disease initially involves vibratory fibers, followed by pain and temperature fibers, and ultimately, all sensory nerves leading to the insensate foot. Poorly fitting shoes, small stones and particulate matter can lead to undetected focal trauma, which can later develop into full-thickness ulceration. In addition to diminished sensibility, patients with sensory neuropathy may experience burning, tingling and hy- 16 peresthesia in affected areas. These sensory changes, fortunately, diminish with time.
Motor dysfunction leads to atrophy and weakness of the intrinsic muscles of the foot, resulting in an imbalance between the flexor and extensor mechanisms, clawing of the toes and increased prominence of the metatarsal heads. The resultant claw-foot deformity creates abnormal pressure points along the plantar metatarsal heads, tips of the toes and the dorsal surface of the PIP joints. Combined with an insensate foot, the pressure points become susceptible to undetected focal trauma, skin breakdown and foot ulceration.
Autonomic neuropathy leads to loss of sympathetic tone and increased arteriovenous shunting in the foot, resulting in decreased nutrient flow. Deinnervation of sweat glands results in dry skin, predisposing to skin cracking and local infection. In addition, loss of sympathetic innervation to the bone may lead to increased bone blood flow, resulting in osteopenia and “bone washout.”
The combination of advanced sensory, motor and autonomic dysfunction contributes to the development of the Charcot foot, a deformity now seen almost exclusively in diabetics. The combination of foot deformity, walking on an insensate foot, and bone resorption results in joint instability, leading to bone and joint destruction. Breakdown of the tarsometatarsal joints and eversion of the plantar arch create the characteristic “rocker-bottom” foot. The deformity creates new pressure points on the plantar surface, which can lead to ulceration and represents a total breakdown of foot architecture.
Infection
Diabetic foot infections are the end result of the combined effects ischemia and neuropathy. The lesion typically starts as a neglected or unrecognized infection in the insensate foot. A break in skin integrity, such as a puncture wound, a neuropathic ulcer, an ingrown nail or a crack in the skin allows bacteria to locally disseminate. Poor tissue perfusion, diminished sensibility and an impaired inflammatory response lead to a rapid progression of what would otherwise be a local infection. The bacterial flora
