
- •Introduction
- •Epidemiology
- •Risk factors
- •Sex distribution
- •Maternal factors
- •Ethnicity
- •Intestinal segment length
- •Preterm infants
- •Associated syndromes
- •Family history
- •Associated congenital anomalies
- •Mechanisms/pathophysiology
- •Enteric nervous system development
- •Signalling pathways in HSCR
- •Role of extracellular matrix in HSCR
- •Genetic factors
- •Variants, partial penetrance and epigenetics
- •Disease models
- •Diagnosis, screening and prevention
- •Clinical presentation
- •Diagnosis
- •Rectal biopsy
- •Histopathological evaluation
- •Differential diagnosis
- •Management
- •Preoperative management
- •Surgical treatment
- •Optimal timing of surgery
- •Single-stage versus multistage surgery
- •Optimal surgical approach and technique
- •Determining the extent of aganglionosis
- •Levelling biopsies and intraoperative pathology
- •Postoperative surgical pathology
- •Postoperative complications
- •Postoperative HAEC
- •Quality of life
- •Outlook
- •Genetics and genomics
- •Diagnosis
- •Treatment
- •Patient-centred research
- •Acknowledgements
Primer
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prevalence of bowel functional |
|
|
|
|
|
Adulthood |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Follow-up based on |
|
|||||||
|
|
|
|
|
|
|
|
|
impairment reduces over time |
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
transitional care assessment |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Sexual function and fertility |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• In•lammatory bowel disease |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Familial MTC |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Infancy |
|
|
Childhood |
|
|
Adolescence |
|
|
Psychosocial elements |
|
||||||||||
|
|
|||||||||||||||||||||
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Surgical and medical factors |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Accurate diagnosis |
|
|
|
• Management of HAEC |
|
|
|
• Evaluate bowel function |
|
|
|
Bowel function impairment |
|
|||||||
|
|
of disease level |
|
|
|
• Obstructive symptoms |
|
|
|
• Evaluate urological |
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
Potential social issues |
|
||||||||||
|
|
• Appropriate primary |
|
|
|
• Maintain intestinal microbiota |
|
|
|
function |
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
over time in HSCR |
|
||||||||||
|
|
pull-through |
|
|
|
homeostasis |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
• Multidisciplinary |
|
|
|
|
|
||||
|
|
• Minimize early life |
|
|
• Encourage positive |
|
|
|
assessment of |
|
|
|
|
|
||||||||
|
|
pain and trauma |
|
|
coping skills |
|
|
|
health-care needs |
|
|
|
|
|
||||||||
|
|
• Manage parental stress |
|
|
• Enable participation in |
|
|
|
• Transitional care |
|
|
|
|
|
||||||||
|
|
• Patient support organizations |
|
|
normal activities of daily life |
|
|
|
• Encourage health literacy |
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||
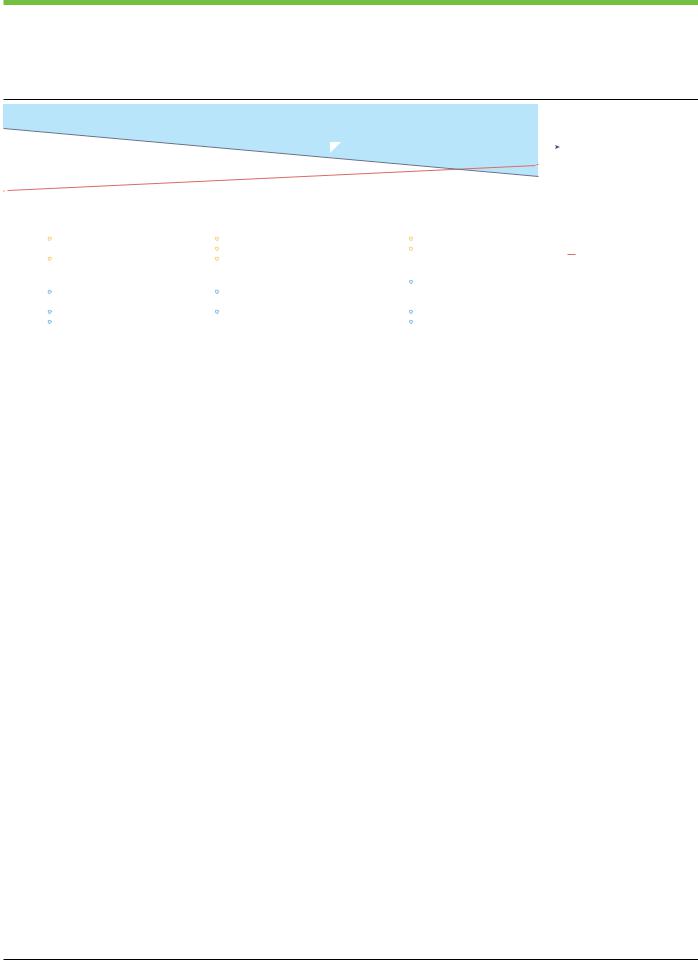
Fig. 7 | Optimizing functional outcomes and quality of life after pull-through |
other medical and psychosocial concerns with a potential impact on quality |
|
||||||||||||||||||||
in Hirschsprung disease. The prevalence of bowel functional impairment in |
of life, which are important to address at appropriate developmental stages |
|
||||||||||||||||||||
rectosigmoid Hirschsprung disease (HSCR) decreases over time, but the need |
to meet the changing health-care needs of patients during growth and |
|
||||||||||||||||||||
for clinicians to encompass the wider potential psychosocial elements that |
into adulthood. HAEC, HSCR-associated enterocolitis; MTC, medullary |
|
||||||||||||||||||||
may be involved increases over time. Patients with HSCR may experience |
thyroid cancer. |
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Quality of life
After undergoing appropriate pull-through surgery for rectosigmoid HSCR, most patients experience favourable bowel functional outcomes in the long-term. However, symptoms of impaired bowel function are common during the first few years after surgery183,184. These symptoms include difficulties with faecal control, impaired rectal sensation, an elevated stooling frequency, episodically obstructive defaecation and enterocolitis. By adulthood, most patients report bowel function similar to that in peers from the general population, but ~10% continue to experience problematic faecal soiling, which can impact their quality of life138.
Although no substantial differences exist in outcomes between Yancey–Soave (endorectal) pull-through and Duhamel (retrorectal) pull-through, an elevated bowel frequency and overall incidence of enterocolitis episodes may be more frequent after Yancey–Soave pull-through than after the Duhamel procedure, whereas constipation and defects in faecal control may be slightly more prevalent after the Duhamel operation than after Yancey–Soave pull-through185. Long-segment and total colonic aganglionosis have more guarded outcomes, with more disease-specific complications, including a greater incidence of HAEC and an increased requirement for attention to growth and nutritional needs linked to a loss of a greater segment of bowel, including small intestine186.
In the presence of a HSCR-associated chromosomal disorder such as Down syndrome, Mowat–Wilson syndrome or cartilage–hair hypoplasia, bowel functional outcomes and quality of life outcomes are generally less favourable and more difficult to predict in individual patients than in patients without an associated disorder. When neurocognitive issues are present, the functional outlook is markedly affected, with rates of faecal soiling and urinary incontinence reaching 50%, and the requirement for a permanent stoma to manage these issues is high, reaching 22%187. In cartilage–hair hypoplasia, cellular immunodeficiency has a major impact on clinical outcome, with an increased risk of infections, lung diseases and malignancy188,189. Multiple inter-dependent factors, including deficits in bowel function, sexual or urinary function or related neuropsychological effects can
impair quality of life in patients190–192. Clustering of these issues may occur in certain individuals and lead to poor outcomes187.
During infancy and early childhood, issues with bowel function are frequent and are often related to functional obstruction and HAEC. In early childhood, the priorities are securing age-appropriate faecal continence and the management of bowel functional symptoms to enable participation in normal activities and social interactions19. Patients who have suboptimal outcomes during this phase should receive close follow-up and aftercare to minimize pain and stress from surgical interventions, encourage parental involvement in the care processandaddressparentalstressrelatedtothechild’scondition138,193.
Preserving intestinal homeostasis, including age-specific development of normal intestinal microbiota, is important in optimizing functional outcomes and health-related quality of life in patients with HSCR194. A multidisciplinary specialized approach to care, including surgical and medical factors, is required to address potential urological complications involved with low pelvic surgery195, gynaecological complications such as female infertility191, and increased risk of familial medullary thyroid cancer and inflammatory bowel disease during adulthood196–199 (Fig. 7).
Transition of care to adult practice should be commenced after puberty in patients who continue to have impaired bowel function or other complications. Follow-up arrangements should be clear for patients and families to support the development of adequate health literacy among patients and positivestrategies for coping with residual symptoms,whichmaybepermanent.Patientsupportorganizationsare available in many parts of the world for peer support and information on personal past experiences with HSCR.
Outlook
Although considerable advances have been made in the diagnosis and treatment of HSCR since its original description in 1886, several outstanding research questions remain to be addressed. There is tremendous potential for emerging technologies, promising new areas of research, and advances from related fields to influence the trajectory of HSCR research in several ways.
Nature Reviews Disease Primers | |
(2023) 9:54 |
14 |

Primer
Genetics and genomics
Despite evidence indicating a crucial role for genetics in the development of HSCR, the exact genetic interactions and pathways involved are still not fully understood. Further research is warranted to unravel the different signalling pathways, which could lead to improved diagnosis and treatment. Researchers will continue to identify new genes associated with HSCR and investigate how different genetic mutations impact the severity of the disease. Furthermore, advances in genomics, proteomics, metabolomics and transcriptomics, and new gene editing technologies, could help researchers better understand the genetic basis of HSCR and potentially develop novel therapies targeting specific genetic mutations.
Diagnosis
Although several diagnostic tests are available for HSCR, they are not alwaysaccurate.Hence,moreresearchisneededtodeveloplessinvasive, more accurate and reliable diagnostic tests for HSCR and its complications,suchasHAEC.Newimagingtechniques,suchasMRIandCTscans, to detect abnormalities in the colon or rectum, including the potential forprenataldetectionofthedisease,mustbeexplored.Machinelearning andartificialintelligencetechnologiesmayhavethepotentialtoimprove the accuracy of diagnostic tests for HSCR. For example, artificial intelligence algorithms are being developed to analyse histological images and identify subtle abnormalities in the colon or rectum that might be missed by human observers200. Moreover, the use of artificial intelligencemaybeparticularlyusefulinsettingswherepathologyexpertise islacking201.Accuratelydeterminingtheextentofaganglionosisduring surgeryiscrucialtoavoidresidualaganglionosisafterpull-throughand thecurrentapproachreliesonintraoperativefrozenbiopsies,whichcan betime-consumingandrequiretheavailabilityofanexperthistopatholo- gist.ConfocallaserendomicroscopyhasbeenusedtovisualizetheENS invitroandinvivo,andmaybecomeausefulreal-timetooltodetermine the length of aganglionosis during pull-through202,203.
Treatment
To date, no consensus exists to suggest the best surgical technique and no evidence is available to suggest that one approach is superior to all others. Further research is needed to determine the most effective surgical technique or subsets of patients who might benefit more from one technique than from another. In parallel, new treatments including robot-assisted approaches and non-surgical approaches are being explored. Multiple groups worldwide have ongoing research programmes employing the use of stem cell therapy to regenerate the missing ganglion cells in the aganglionic bowel or transition zone, or to develop bioengineered intestinal segments, which could potentially restore normal bowel function. Indeed, enteric NCCs transplanted in vitro into the aganglionic gut of a mouse model of HSCR have been shown to migrate, proliferate and differentiate, resulting in successful colonic contractile responses204,205. Moreover, the development of ENS progenitors from human pluripotent stem cells is a promising tool to identify potential cellular targets and develop drug-based strategies for HSCR treatment206. However, safety and quality control, patient selection and timing of interventions have been an enormous challenges in the past few decades.
Patient-centred research
Further research is needed to understand the long-term outcomes of HSCR and to develop strategies to prevent or manage these complications207. Efforts to understand the psychological and social
effects of the condition and to develop interventions to improve the quality of life of affected individuals and their families are warranted. Over the past decade, patient-centred research and family-centred care and research, involving patients and families in the design and implementation of research studies have gained attention. This shift will help ensure that research efforts are prioritized on the needs of patients and families. This approach will enable ‘value-based care’, shifting from improving patient health to improving patient-relevant outcomes208. Advances in patient-centred technologies, such as mobile apps and wearable devices, could be used to monitor bowel function, track symptoms and provide personalized support and advice to patients and their families. These methods have the potential to enable earlier interventions to improve the quality of life of patients with HSCR, which is the ultimate end-goal of treatment.
References
1.\ Best, K. E. et al. Hirschsprung’s disease prevalence in Europe: a register based study.
Birth Defects Res. A Clin. Mol. Teratol. 100, 695–702 (2014).
2.\ Kawaguchi, A. L. et al. Management and outcomes for long-segment Hirschsprung disease: a systematic review from the APSA Outcomes and Evidence Based Practice Committee. J. Pediatr. Surg. 56, 1513–1523 (2021).
3.\ Fusaro, F. et al. Autologous intestinal reconstructive surgery in the management of total intestinal aganglionosis. J. Pediatr. Gastroenterol. Nutr. 68, 635–641 (2019).
4.\ Saxton, M. L., Ein, S. H., Hoehner, J. & Kim, P. C. W. Near-total intestinal aganglionosis: long-term follow-up of a morbid condition. J. Pediatr. Surg. 35, 669–672 (2000).
5.\ Chatterjee, S. & Chakravarti, A. A gene regulatory network explains RET–EDNRB epistasis in Hirschsprung disease. Hum. Mol. Genet. 28, 3137–3147 (2019).
6.\ De Lorijn, F. et al. Diagnosis of Hirschsprung’s disease: a prospective, comparative accuracy study of common tests. J. Pediatr. 146, 787–792 (2005).
7.\ Swenson, O., Rheinlander, H. F. & Diamond, I. Hirschsprung’s disease; a new concept of the etiology – operative results in 34 patients. N. Engl. J. Med. 241, 551–556 (1949).
This article is the first to report a successful surgical reconstruction technique for Hirschsprung disease, that is still the most performed technique nowadays.
8.\ Duhamel, B. New operation for congenital megacolon: retrorectal and transanal lowering of the colon, and its possible application to the treatment of various other malformations [French]. Presse Med. 64, 2249–2250 (1956).
9.\ Yancey, A. G., Cromartie, J. E., Ford, J. R., Nichols, R. R. & Saville, A. F. A modi ication of the Swenson technique for congenital megacolon. J. Natl Med. Assoc. 44, 356–363 (1952).
10.\ Woode, D. et al. Asa G Yancey: The irst to describe a modi ication of the Swenson technique for Hirschsprung disease. J. Pediatr. Surg. 57, 1701–1703 (2022).
11.\ Soave, F. Hirschsprung’s disease: a new surgical technique. Arch. Dis. Child. 39, 116–124 (1964).
12.\ Rehbein, F. & Von Zimmermann, H. Results with abdominal resection in Hirschsprung’s disease. Arch. Dis. Child. 35, 29–37 (1960).
13.\ Smith, B. M., Steiner, R. B. & Lobe, T. E. Laparoscopic Duhamel pullthrough procedure for Hirschsprung’s disease in childhood. J. Laparoendosc. Surg. 4, 273–276 (1994).
14.\ Georgeson, K. E., Fuenfer, M. M. & Hardin, W. D. Primary laparoscopic pull-through for Hirschsprung’s disease in infants and children. J. Pediatr. Surg. 30, 1017–1022 (1995).
This article reports a major advance in surgical management of Hirschsprung disease, with the use of minimally invasive surgery.
15.\ De la Torre-Mondragón, L. & Ortega-Salgado, J. A. Transanal endorectal pull-through for Hirschsprung’s disease. J. Pediatr. Surg. 33, 1283–1286 (1998).
16.\ Langer, J. C., Minkes, R. K., Mazziotti, M. V., Skinner, M. A. & Winthrop, A. L. Transanal one-stage Soave procedure for infants with Hirschsprung’s disease. J. Pediatr. Surg. 34, 148–152 (1999).
17.\ Rintala, R. J. & Pakarinen, M. P. Long-term outcomes of Hirschsprung’s disease.
Semin. Pediatr. Surg. 21, 336–343 (2012).
18.\ Huerta, C. T. et al. Nationwide outcomes of newborns with rectosigmoid versus long-segment Hirschsprung disease. J. Pediatr. Surg. https://doi.org/10.1016/ J.JPEDSURG.2023.01.001 (2023).
19.\ Kyrklund, K. et al. ERNICA guidelines for the management of rectosigmoid Hirschsprung’s disease. Orphanet J. Rare Dis. 15, 164 (2020).
20.\ Chia, S. T., Chen, S. C., Lu, C. L., Sheu, S. M. & Kuo, H. C. Epidemiology of Hirschsprung’s disease in Taiwanese children: a 13-year nationwide population-based study. Pediatr. Neonatol. 57, 201–206 (2016).
21.\ Lof Granstrom, A. et al. Maternal risk factors and perinatal characteristics for Hirschsprung disease. Pediatrics 138, e20154608 (2016).
22.\ Tilghman, J. M. et al. Molecular genetic anatomy and risk pro ile of Hirschsprung’s disease. N. Engl. J. Med. 380, 1421–1432 (2019).
This study provides insight into the complexity of Hirschsprung disease genetics and heritability.
Nature Reviews Disease Primers | |
(2023) 9:54 |
15 |

Primer
23.\ |
Anderson, J. E. et al. Epidemiology of Hirschsprung disease in California from 1995 to 2013. |
56.\ |
Barlow, A., De Graa , E. & Pachnis, V. Enteric nervous system progenitors are |
|
Pediatr. Surg. Int. 34, 1299–1303 (2018). |
|
coordinately controlled by the G protein-coupled receptor EDNRB and the receptor |
24.\ |
Rajab, A., Freeman, N. V. & Patton, M. A. Hirschsprung’s disease in Oman. J. Pediatr. Surg. |
|
tyrosine kinase RET. Neuron 40, 905–916 (2003). |
|
32, 724–727 (1997). |
57.\ |
Nagy, N. & Goldstein, A. M. Endothelin-3 regulates neural crest cell proliferation |
25.\ |
Bradnock, T. J. et al. Hirschsprung’s disease in the UK and Ireland: incidence and |
|
and di erentiation in the hindgut enteric nervous system. Dev. Biol. 293, 203–217 |
|
anomalies. Arch. Dis. Child. 102, 722–727 (2017). |
|
(2006). |
26.\ |
Taghavi, K. et al. Ethnic variations in the childhood prevalence of Hirschsprung disease |
58.\ |
Robertson, K., Mason, I. & Hall, S. Hirschsprung’s disease: genetic mutations in mice and |
|
in New Zealand. ANZ J. Surg. 89, 1246–1249 (2019). |
|
men. Gut 41, 436–441 (1997). |
27.\ |
Xiao, J. et al. Comprehensive characterization of the genetic landscape of familial |
59.\ |
Bondurand, N., Natarajan, D., Barlow, A., Thapar, N. & Pachnis, V. Maintenance of |
|
Hirschsprung’s disease. World J. Pediatr. https://doi.org/10.1007/s12519-023-00686-x |
|
mammalian enteric nervous system progenitors by SOX10 and endothelin 3 signalling. |
|
(2023). |
|
Development 133, 2075–2086 (2006). |
28.\ |
Goldberg, E. L. An epidemiological study of Hirschsprung’s disease. Int. J. Epidemiol. 13, |
60.\ |
Kapur, R. P. Early death of neural crest cells is responsible for total enteric aganglionosis |
|
479–485 (1984). |
|
in Sox10Dom/Sox10Dom mouse embryos. Pediatr. Dev. Pathol. 2, 559–569 (1999). |
29.\ |
Tam, P. K. Hirschsprung’s disease: a bridge for science and surgery. J. Pediatr. Surg. 51, |
61.\ |
Pattyn, A., Morin, X., Cremer, H., Goridis, C. & Brunet, J. F. The homeobox gene Phox2b |
|
18–22 (2016). |
|
is essential for the development of autonomic neural crest derivatives. Nature 399, |
30.\ |
Gunadi et al. NRG1 variant e ects in patients with Hirschsprung disease. BMC Pediatr. 18, |
|
366–370 (1999). |
|
292 (2018). |
62.\ |
Broch, A. et al. Congenital central hypoventilation syndrome and Hirschsprung disease: |
31.\ |
Fadista, J. et al. Genome-wide association study of Hirschsprung disease detects a novel |
|
a retrospective review of the French National Registry Center on 33 cases. J. Pediatr. |
|
low-frequency variant at the RET locus. Eur. J. Hum. Genet. 26, 561–569 (2018). |
|
Surg. 54, 2325–2330 (2019). |
32.\ |
Emison, E. S. et al. Di erential contributions of rare and common, coding and noncoding |
63.\ |
Sasaki, A. et al. Novel PHOX2B mutations in congenital central hypoventilation |
|
Ret mutations to multifactorial Hirschsprung disease liability. Am. J. Hum. Genet. 87, |
|
syndrome. Pediatr. Int. 61, 393–396 (2019). |
|
60–74 (2010). |
64.\ |
Lake, J. I. & Heuckeroth, R. O. Enteric nervous system development: migration, |
33.\ |
Moore, S. W. Chromosomal and related Mendelian syndromes associated with |
|
di erentiation, and disease. Am. J. Physiol. Gastrointest. Liver Physiol. 305, G1–G24 |
|
Hirschsprung’s disease. Pediatr. Surg. Int. 28, 1045–1058 (2012). |
|
(2013). |
34.\ |
Chen, Y. et al. The prevalence and clinical presentation of Hirschsprung’s disease in preterm |
65.\ |
Newgreen, D. F. & Hartley, L. Extracellular matrix and adhesive molecules in the early |
|
infants: a systematic review and meta-analysis. Pediatr. Surg. Int. 38, 523–532 (2022). |
|
development of the gut and its innervation in normal and spotting lethal rat embryos. |
35.\ |
Duess, J. W., Hofmann, A. D. & Puri, P. Prevalence of Hirschsprung’s disease in premature |
|
Acta Anat. 154, 243–260 (1995). |
|
infants: a systematic review. Pediatr. Surg. Int. 30, 791–795 (2014). |
66.\ |
Soret, R. et al. A collagen VI-dependent pathogenic mechanism for Hirschsprung’s |
36.\ |
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in |
|
disease. J. Clin. Invest. 125, 4483–4496 (2015). |
|
the year 2010 with time trends since 1990 for selected countries: a systematic analysis |
67.\ |
Moore, S. W. Advances in understanding the association between Down syndrome and |
|
and implications. Lancet 379, 2162–2172 (2012). |
|
Hirschsprung disease (DS-HSCR). Pediatr. Surg. Int. 34, 1127–1137 (2018). |
37.\ |
Dershowitz, L. B., Li, L., Pasca, A. M. & Kaltschmidt, J. A. Anatomical and functional |
68.\ |
Fu, M. et al. 37/67-laminin receptor facilitates neural crest cell migration during enteric |
|
maturation of the mid-gestation human enteric nervous system. Nat. Commun. 14, 2680 |
|
nervous system development. FASEB J. 34, 10931–10947 (2020). |
|
(2023). |
69.\ |
Nagy, N. et al. Collagen 18 and agrin are secreted by neural crest cells to remodel |
38.\ |
Amiel, J. et al. Hirschsprung disease, associated syndromes and genetics: a review. |
|
their microenvironment and regulate their migration during enteric nervous system |
|
J. Med. Genet. 45, 1–14 (2008). |
|
development. Development 145, dev160317 (2018). |
39.\ |
Friedmacher, F. & Puri, P. Hirschsprung’s disease associated with Down syndrome: |
70.\ |
Nagy, N. et al. Sonic hedgehog controls enteric nervous system development by |
|
a meta-analysis of incidence, functional outcomes and mortality. Pediatr. Surg. Int. 29, |
|
patterning the extracellular matrix. Development 143, 264–275 (2016). |
|
937–946 (2013). |
71.\ |
Dutt, S., Kléber, M., Matasci, M., Sommer, L. & Zimmermann, D. R. Versican V0 and V1 |
40.\ |
Brosens, E. et al. Genetics of enteric neuropathies. Dev. Biol. 417, 198–208 (2016). |
|
guide migratory neural crest cells. J. Biol. Chem. 281, 12123–12131 (2006). |
41.\ |
Moore, S. W. The contribution of associated congenital anomalies in understanding |
72.\ |
Ring, C., Hassell, J. & Halfter, W. Expression pattern of collagen IX and potential role |
|
Hirschsprung’s disease. Pediatr. Surg. Int. 22, 305–315 (2006). |
|
in the segmentation of the peripheral nervous system. Dev. Biol. 180, 41–53 (1996). |
42.\ |
Pini Prato, A. et al. A prospective observational study of associated anomalies in |
73.\ |
Nagy, N. et al. Endothelial cells promote migration and proliferation of enteric neural |
|
Hirschsprung’s disease. Orphanet J. Rare Dis. 8, 184 (2013). |
|
crest cells via β1 integrin signaling. Dev. Biol. 330, 263–272 (2009). |
43.\ |
Pini Prato, A. et al. Congenital anomalies of the kidney and urinary tract in a cohort of |
74.\ |
Akbareian, S. E. et al. Enteric neural crest-derived cells promote their migration by |
|
280 consecutive patients with Hirschsprung disease. Pediatr. Nephrol. 36, 3151–3158 |
|
modifying their microenvironment through tenascin-C production. Dev. Biol. 382, |
|
(2021). |
|
446–456 (2013). |
44.\ |
Hofmann, A. D., Duess, J. W. & Puri, P. Congenital anomalies of the kidney and |
75.\ |
Raghavan, S., Gilmont, R. R. & Bitar, K. N. Neuroglial di erentiation of adult enteric |
|
urinary tract (CAKUT) associated with Hirschsprung’s disease: a systematic review. |
|
neuronal progenitor cells as a function of extracellular matrix composition. Biomaterials |
|
Pediatr. Surg. Int. 30, 757–761 (2014). |
|
34, 6649–6658 (2013). |
45.\ |
Nagy, N. & Goldstein, A. M. Enteric nervous system development: a crest cell’s journey |
76.\ |
Kapur, R. P. Colonization of the murine hindgut by sacral crest-derived neural precursors: |
|
from neural tube to colon. Semin. Cell Dev. Biol. 66, 94–106 (2017). |
|
experimental support for an evolutionarily conserved model. Dev. Biol. 227, 146–155 |
|
This article comprehensively reviews the current understanding of the factors |
|
(2000). |
|
involved in early development of the enteric nervous system, and areas in need |
77.\ |
Huang, T. et al. Direct interaction of Sox10 with cadherin-19 mediates early sacral neural |
|
of investigation. |
|
crest cell migration: implications for enteric nervous system development defects. |
46.\ |
Wallace, A. S. & Burns, A. J. Development of the enteric nervous system, smooth muscle |
|
Gastroenterology 162, 179–192.e11 (2022). |
|
and interstitial cells of Cajal in the human gastrointestinal tract. Cell Tissue Res. 319, |
78.\ |
Burns, A. J., Champeval, D. & Le Douarin, N. M. Sacral neural crest cells colonise |
|
367–382 (2005). |
|
aganglionic hindgut in vivo but fail to compensate for lack of enteric ganglia. Dev. Biol. |
47.\ |
Rolle, U., Nemeth, L. & Puri, P. Nitrergic innervation of the normal gut and in motility |
|
219, 30–43 (2000). |
|
disorders of childhood. J. Pediatr. Surg. 37, 551–567 (2002). |
79.\ |
Burns, A. J. & Le Douarin, N. M. The sacral neural crest contributes neurons and glia to the |
48.\ |
Burns, A. J. & Thapar, N. Advances in ontogeny of the enteric nervous system. |
|
post-umbilical gut: spatiotemporal analysis of the development of the enteric nervous |
|
Neurogastroenterol. Motil. 18, 876–887 (2006). |
|
system. Development 125, 4335–4347 (1998). |
49.\ |
Uesaka, T., Nagashimada, M. & Enomoto, H. Neuronal di erentiation in Schwann cell |
80.\ |
Uesaka, T. et al. Enhanced enteric neurogenesis by Schwann cell precursors in mouse |
|
lineage underlies postnatal neurogenesis in the enteric nervous system. J. Neurosci. 35, |
|
models of Hirschsprung disease. Glia 69, 2575–2590 (2021). |
|
9879–9888 (2015). |
81.\ |
Sribudiani, Y. et al. Identi ication of variants in RET and IHH pathway members in a large |
50.\ |
Uribe, R. A., Hong, S. S. & Bronner, M. E. Retinoic acid temporally orchestrates |
|
family with history of Hirschsprung disease. Gastroenterology 155, 118–129.e6 (2018). |
|
colonization of the gut by vagal neural crest cells. Dev. Biol. 433, 17–32 (2018). |
82.\ |
Karim, A., Tang, C. S. & Tam, P. K. The emerging genetic landscape of Hirschsprung |
51.\ |
Howard, A. G. A. & Uribe, R. A. Hox proteins as regulators of extracellular matrix |
|
disease and its potential clinical applications. Front. Pediatr. 9, 638093 (2021). |
|
interactions during neural crest migration. Diferentiation 128, 26–32 (2022). |
|
This article provides an extensive review of gene mutations and syndromes associated |
52.\ |
Fu, M., Lui, V. C. H., Sham, M. H., Cheung, A. N. Y. & Tam, P. K. H. HOXB5 expression is |
|
with Hirschsprung disease. |
|
spatially and temporarily regulated in human embryonic gut during neural crest cell |
83.\ |
Ke, J., Zhu, Y. & Miao, X. The advances of genetics research on Hirschsprung’s disease. |
|
colonization and di erentiation of enteric neuroblasts. Dev. Dyn. 228, 1–10 (2003). |
|
Pediatr. Investig. 2, 189–195 (2018). |
53.\ |
Ganz, J. Gut feelings: studying enteric nervous system development, function, and |
84.\ |
Mueller, J. L. & Goldstein, A. M. The science of Hirschsprung disease: what we know |
|
disease in the zebra ish model system. Dev. Dyn. 247, 268–278 (2018). |
|
and where we are headed. Semin. Pediatr. Surg. 31, 151157 (2022). |
54.\ |
Anderson, R. B. et al. The cell adhesion molecule l1 is required for chain migration of |
85.\ |
Tang, C. S., Karim, A., Zhong, Y., Chung, P. H. & Tam, P. K. Genetics of Hirschsprung’s |
|
neural crest cells in the developing mouse gut. Gastroenterology 130, 1221–1232 (2006). |
|
disease. Pediatr. Surg. Int. 39, 104 (2023). |
55.\ |
Baker, P. A., Ibarra-Garcıá-Padilla, R., Venkatesh, A., Singleton, E. W. & Uribe, R. A. In toto |
86.\ |
Kuil, L. E. et al. Size matters: large copy number losses in Hirschsprung disease |
|
imaging of early enteric nervous system development reveals that gut colonization is |
|
patients reveal genes involved in enteric nervous system development. PLoS Genet. 17, |
|
tied to proliferation downstream of Ret. Development 149, dev200668 (2022). |
|
e1009698 (2021). |
Nature Reviews Disease Primers | |
(2023) 9:54 |
16 |

Primer
87.\ Gui, H. et al. Whole exome sequencing coupled with unbiased functional analysis reveals new Hirschsprung disease genes. Genome Biol. 18, 48 (2017).
This study identifies for the first time novel genes involved in Hirschsprung disease using whole-genome sequencing, providing novel insights into the development of the enteric nervous system.
88.\ Le, T. L. et al. Dysregulation of the NRG1/ERBB pathway causes a developmental disorder with gastrointestinal dysmotility in humans. J. Clin. Invest. 131, e145837 (2021).
89.\ Brosens, E., MacKenzie, K. C., Alves, M. M. & Hofstra, R. M. W. Do RET somatic mutations play a role in Hirschsprung disease? Genet. Med. 20, 1477–1478 (2018).
90.\ Heuckeroth, R. O. Hirschsprung disease – integrating basic science and clinical medicine to improve outcomes. Nat. Rev. Gastroenterol. Hepatol. 15, 152–167 (2018).
This review provides insights into the pathophysiology of Hirschsprung disease, and future research direction.
91.\ Tam, P. K. & Garcia-Barcelo, M. Genetic basis of Hirschsprung’s disease. Pediatr. Surg. Int. 25, 543–558 (2009).
92.\ Lyonnet, S., Pelet, A., Abel, L. & Bolino, A. A gene for Hirschsprung disease maps to the proximal arm of chromosome 10. Nat. Genet. 4, 346–350 (1993).
This study is the first to show the mutation of the RET gene, the most commonly involved gene in Hirschsprung disease.
93.\ Emison, E. S. et al. A common sex-dependent mutation in a RET enhancer underlies Hirschsprung disease risk. Nature 434, 857–863 (2005).
94.\ Chatterjee, S. et al. Enhancer variants synergistically drive dysfunction of a gene regulatory network in Hirschsprung disease. Cell 167, 355–368.e10 (2016).
95.\ Luzon-Toro, B. et al. What is new about the genetic background of Hirschsprung disease? Clin. Genet. 97, 114–124 (2020).
96.\ Torroglosa, A. Epigenetic mechanisms in Hirschsprung disease. Int J. Mol. Sci. 20, 3123 (2019).
97.\ Strobl-Mazzulla, P. H., Marini, M. & Buzzi, A. Epigenetic landscape and miRNA involvement during neural crest development. Dev. Dyn. 241, 1849–1856 (2012).
98.\ Fujiwara, N., Nakazawa-Tanaka, N. & Yamataka, A. Animal models of Hirschsprung’s disease: state of the art in translating experimental research to the bedside.
Eur. J. Pediatr. Surg. 29, 361–377 (2019).
99.\ Cardinal, T. et al. Male-biased aganglionic megacolon in the TashT mouse model of Hirschsprung disease involves upregulation of p53 protein activity and Ddx3y gene expression. PLoS Genet. 16, e1009008 (2020).
100.\ Garcia, S. B., Minto, S. B., De Marques, I. S. & Kannen, V. Myenteric denervation of the gut with benzalkonium chloride: a review of forty years of an experimental model.
Can. J. Gastroenterol. Hepatol. 2019, 3562492 (2019).
101.\ Fu, M. et al. Vitamin A facilitates enteric nervous system precursor migration by reducing Pten accumulation. Development 137, 631–640 (2010).
102.\ Moore, S. W. Total colonic aganglionosis and Hirschsprung’s disease: shades of the same or di erent? Pediatr. Surg. Int. 25, 659–666 (2009).
103.\ Alnajar, H., Murro, D., Alsadi, A. & Jakate, S. Spectrum of clinicopathological deviations in long-segment Hirschsprung disease compared with short-segment Hirschsprung disease: a single-institution study. Int. J. Surg. Pathol. 25, 216–221 (2017).
104.\ Lewit, R. A., Kuruvilla, K. P., Fu, M. & Gosain, A. Current understanding of Hirschsprungassociated enterocolitis: pathogenesis, diagnosis and treatment. Semin. Pediatr. Surg. 31, 151162 (2022).
This article provides a comprehensive review of our current understanding of Hirschsprung-associated enterocolitis, which is the most severe and frequent complication related to this disease.
105.\ Gosain, A. et al. Guidelines for the diagnosis and management of Hirschsprung-associated enterocolitis. Pediatr. Surg. Int. 33, 517–521 (2017).
106.\ Abbo, O. et al. Necrotizing enterocolitis in full term neonates: is there always an underlying cause? J. Neonatal Surg. 2, 29 (2013).
107.\ Raboel, E. H. Necrotizing enterocolitis in full-term neonates: is it aganglionosis?
Eur. J. Pediatr. Surg. 19, 101–104 (2009).
108.\ Beltman, L., Labib, H., Oosterlaan, J., van Heurn, E. & Derikx, J. Risk factors for complications in patients with Hirschsprung disease while awaiting surgery: beware of bowel perforation. J. Pediatr. Surg. https://doi.org/10.1016/J.JPEDSURG.2022.02.022 (2022).
109.\ Mc Laughlin, D. & Puri, P. Familial Hirschsprung’s disease: a systematic review.
Pediatr. Surg. Int. 31, 695–700 (2015).
110.\ Zani, A. & Montalva, L. in Encyclopedia of Gastroenterology 2nd edn (ed. Kuipers, E. J.) 644–651 (Academic, 2020).
111.\ Garcia, R. et al. Use of the recto-sigmoid index to diagnose Hirschsprung’s disease.
Clin. Pediatr. 46, 59–63 (2007).
112.\ Stranzinger, E., DiPietro, M. A., Teitelbaum, D. H. & Strouse, P. J. Imaging of total colonic Hirschsprung disease. Pediatr. Radiol. 38, 1162–1170 (2008).
113.\ De Lorijn, F., Kremer, L. C. M., Reitsma, J. B. & Benninga, M. A. Diagnostic tests in Hirschsprung disease: a systematic review. J. Pediatr. Gastroenterol. Nutr. 42, 496–505 (2006).
114.\ Doodnath, R. & Puri, P. A systematic review and meta-analysis of Hirschsprung’s disease presenting after childhood. Pediatr. Surg. Int. 26, 1107–1110 (2010).
115.\ Jarvi, K., Koivusalo, A., Rintala, R. J. & Pakarinen, M. P. Anorectal manometry with reference to operative rectal biopsy for the diagnosis/exclusion of Hirschprung’s disease in children under 1 year of age. Int. J. Colorectal Dis. 24, 451–454 (2009).
116.\ Liang, Y., An, T. & Xin, W. Exploring the value of rectal anal canal pressure measurement in the diagnosis of Hirschsprung’s disease. Heliyon 8, e09619 (2022).
117.\ Baaleman, D. F. et al. The not-so-rare absent RAIR: internal anal sphincter achalasia in a review of 1072 children with constipation undergoing high-resolution anorectal manometry. Neurogastroenterol. Motil. 33, e14028 (2021).
118.\ Wright, N. J. et al. Mortality from gastrointestinal congenital anomalies at 264 hospitals in 74 low-income, middle-income, and high-income countries: a multicentre, international, prospective cohort study. Lancet 398, 325–339 (2021).
119.\ Muise, E. D. & Cowles, R. A. Rectal biopsy for Hirschsprung’s disease: a review of techniques, pathology, and complications. World J. Pediatr. 12, 135–141 (2016).
120.\ Friedmacher, F. & Puri, P. Rectal suction biopsy for the diagnosis of Hirschsprung’s disease: a systematic review of diagnostic accuracy and complications. Pediatr. Surg. Int. 31, 821–830 (2015).
121.\ Ambartsumyan, L., Smith, C. & Kapur, R. P. Diagnosis of Hirschsprung disease.
Pediatr. Dev. Pathol. 23, 8–22 (2020).
122.\ Muise, E. D., Hardee, S., Morotti, R. A. & Cowles, R. A. A comparison of suction and full-thickness rectal biopsy in children. J. Surg. Res. 201, 149–155 (2016).
123.\ Meier-Ruge, W. A. & Bruder, E. Pathology of chronic constipation in pediatric and adult coloproctology. Pathobiology 72, 1–106 (2005).
124.\ Kapur, R. P. Calretinin-immunoreactive mucosal innervation in very short-segment Hirschsprung disease: a potentially misleading observation. Pediatr. Dev. Pathol. 17, 28–35 (2014).
125.\ Green, N., Smith, C. A., Bradford, M. C., Ambartsumyan, L. & Kapur, R. P. Rectal suction biopsy versus incisional rectal biopsy in the diagnosis of Hirschsprung disease.
Pediatr. Surg. Int. 38, 1989–1996 (2022).
126.\ Crofie, J. M. et al. At what age is a suction rectal biopsy less likely to provide adequate tissue for identi ication of ganglion cells? J. Pediatr. Gastroenterol. Nutr. 44, 198–202 (2007).
127.\ Veras, L. V. et al. Guidelines for synoptic reporting of surgery and pathology in Hirschsprung disease. J. Pediatr. Surg. 54, 2017–2023 (2019).
128.\ Venugopal, S., Mancer, K. & Shandling, B. The validity of rectal biopsy in relation to morphology and distribution of ganglion cells. J. Pediatr. Surg. 16, 433–437 (1981).
129.\ Aldridge, R. T. & Campbell, P. E. Ganglion cell distribution in the normal rectum and anal canal. A basis for the diagnosis of Hirschsprung’s disease by anorectal biopsy. J. Pediatr. Surg. 3, 475–490 (1968).
130.\ Weinberg, A. G. The anorectal myenteric plexus: its relation to hypoganglionosis of the colon. Am. J. Clin. Pathol. 54, 637–642 (1970).
131.\ Qualman, S. J., Ja e, R., Bove, K. E. & Monforte-Muñoz, H. Diagnosis of hirschsprung disease using the rectal biopsy: multi-institutional survey. Pediatr. Dev. Pathol. 2, 588–596 (1999).
132.\ Yunis, E. J., Dibbins, A. W. & Sherman, F. E. Rectal suction biopsy in the diagnosis of Hirschsprung disease in infants. Arch. Pathol. Lab. Med. 100, 329–333 (1976).
133.\ Kakita, Y., Oshiro, K., O’Briain, D. S. & Puri, P. Selective demonstration of mural nerves in ganglionic and aganglionic colon by immunohistochemistry for glucose transporter-1: prominent extrinsic nerve pattern staining in Hirschsprung disease. Arch. Pathol. Lab.
Med. 124, 1314–1319 (2000).
134.\ Drabent, P., Bonnard, A., Guimiot, F., Peuchmaur, M. & Berrebi, D. PHOX2B immunostaining: a simple and helpful tool for the recognition of ganglionic cells and diagnosis of Hirschsprung disease. Am. J. Surg. Pathol. 44, 1389–1397 (2020).
135.\ Logan, S. J. et al. Calretinin staining in anorectal line biopsies accurately distinguished Hirschsprung disease in a retrospective study. Pediatr. Dev. Pathol. 25, 645–655 (2022).
136.\ Guinard-Samuel, V., Bonnard, A., Peuchmaur, M. & Berrebi, D. A variant pattern of calretinin immunohistochemistry on rectal suction-biopsies is fully speci ic of short-segment Hirschsprung’s disease. Pediatr. Surg. Int. 30, 803–808 (2014).
137.\ Somme, S. & Langer, J. C. Primary versus staged pull-through for the treatment of Hirschsprung disease. Semin. Pediatr. Surg. 13, 249–255 (2004).
138.\ Jarvi K. et al. Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann Surg. 252, 977–981 (2010).
This study evaluated for the first time controlled long-term outcomes and quality of life in adults born with Hirschsprung disease.
139.\ Apte, A., McKenna, E. & Levitt, M. A. Image of the month: decision-making in surgery for late onset Hirschsprung disease. Eur. J. Pediatr. Surg. Rep. 8, e99–e101 (2020).
140.\ Moore, S. W. Total colonic aganglionosis and Hirschsprung’s disease: a review.
Pediatr. Surg. Int. 31, 1–9 (2015).
141.\ Smith, C., Ambartsumyan, L. & Kapur, R. P. Surgery, surgical pathology, and postoperative management of patients with Hirschsprung disease. Pediatr. Dev. Pathol. 23, 23–39 (2020).
142.\ Teitelbaum, D. H. et al. A decade of experience with the primary pull-through for Hirschsprung disease in the newborn period: a multicenter analysis of outcomes. Ann. Surg. 232, 372–380 (2000).
143.\ Kastenberg, Z. J. et al. Perioperative and long-term functional outcomes of neonatal versus delayed primary endorectal pull-through for children with Hirschsprung disease: a pediatric colorectal and pelvic learning consortium study. J. Pediatr. Surg. 56, 1465–1469 (2021).
144.\ Westfal, M. L. et al. Optimal timing for Soave primary pull-through in short-segment Hirschsprung disease: a meta-analysis. J. Pediatr. Surg. 57, 719–725 (2022).
145.\ Stolwijk, L. J. et al. Neurodevelopmental outcomes after neonatal surgery for major noncardiac anomalies. Pediatrics 137, e20151728 (2016).
146.\ Keunen, K., Sperna Weiland, N. H., de Bakker, B. S., de Vries, L. S. & Stevens, M. F. Impact of surgery and anesthesia during early brain development: a perfect storm.
Paediatr. Anaesth. 32, 697–705 (2022).
Nature Reviews Disease Primers | |
(2023) 9:54 |
17 |

Primer
147.\ Grabowski, J. et al. The e ects of early anesthesia on neurodevelopment: a systematic review. J. Pediatr. Surg. 56, 851–861 (2021).
148.\ Zani, A. et al. European Paediatric Surgeons’ Association survey on the management of Hirschsprung disease. Eur. J. Pediatr. Surg. 27, 96–101 (2017).
149.\ Bischo , A., Levitt, M. A. & Peña, A. Total colonic aganglionosis: a surgical challenge. How to avoid complications? Pediatr. Surg. Int. 27, 1047–1052 (2011).
150.\ Lamoshi, A., Ham, P. B., Chen, Z., Wilding, G. & Vali, K. Timing of the de initive procedure and ileostomy closure for total colonic aganglionosis HD: systematic review. J. Pediatr. Surg. 55, 2366–2370 (2020).
151.\ Wood, R. J. & Garrison, A. P. Total colonic aganglionosis in Hirschsprung disease.
Semin. Pediatr. Surg. 31, 151165 (2022).
152.\ Langer, J. C. et al. One-stage transanal Soave pullthrough for Hirschsprung disease: a multicenter experience with 141 children. Ann. Surg. 238, 569–576 (2003).
153.\ Giuliani, S., Honeyford, K., Chang, C. Y., Bottle, A. & Aylin, P. Outcomes of primary versus multiple-staged repair in Hirschsprung’s disease in England. Eur. J. Pediatr. Surg. 30, 104–110 (2020).
154.\ Hutchings, E. E., Townley, O. G., Lindley, R. M. & Murthi, G. V. S. The role of stomas in the initial and long-term management of Hirschsprung disease. J. Pediatr. Surg. 58, 236–240 (2023).
155.\ Langer, J. C. Surgical approach to Hirschsprung disease. Semin. Pediatr. Surg. 31, 151156 (2022).
156.\ Mottadelli, G. et al. Robotic surgery in Hirschsprung disease: a unicentric experience on 31 procedures. J. Robot. Surg. https://doi.org/10.1007/S11701-022-01488-5 (2022).
157.\ Celtik, U., Yavuz, I. & Ergün, O. Transanal endorectal or transabdominal pull-through for Hirschsprung’s disease; which is better? A systematic review and meta-analysis.
Pediatr. Surg. Int. 39, 89 (2023).
158.\ Stensrud, K. J., Emblem, R. & Bjørnland, K. Anal endosonography and bowel function in patients undergoing di erent types of endorectal pull-through procedures for Hirschsprung disease. J. Pediatr. Surg. 50, 1341–1346 (2015).
159.\ Delgado-Miguel, C. & Camps, J. I. Robotic Soave pull-through procedure for Hirschsprung’s disease in children under 12-months: long-term outcomes.
Pediatr. Surg. Int. 38, 51–57 (2022).
160.\ Li, W. et al. Surgical management of Hirschsprung’s disease: a comparative study between conventional laparoscopic surgery, transumbilical single-site laparoscopic surgery, and robotic surgery. Front. Surg. 9, 924850 (2022).
161.\ Payen, E. et al. Outcome of total colonic aganglionosis involving the small bowel depends on bowel length, liver disease, and enterocolitis. J. Pediatr. Gastroenterol. Nutr. 74, 582–587 (2022).
162.\ Pini Prato, A. et al. Skipped aganglionic lengthening transposition (SALT) for short bowel syndrome in patients with total intestinal aganglionosis: technical report and feasibility.
Pediatr. Surg. Int. 36, 1507–1510 (2020).
163.\ Sauvat, F. et al. Intestinal transplantation for total intestinal aganglionosis: a series of 12 consecutive children. J. Pediatr. Surg. 43, 1833–1838 (2008).
164.\ O’Hare, T. J., McDermott, M., O’Sullivan, M., Dicker, P. & Antao, B. A retrospective cohort study of total colonic aganglionosis: is the appendix a reliable diagnostic tool?
J. Neonatal Surg. 5, 44 (2016).
165.\ Reppucci, M. L. et al. Is the appendix a good organ to diagnose total colonic aganglionosis? Pediatr. Surg. Int. 38, 25–30 (2022).
166.\ Lane, V., Levitt, M., Baker, P., Minneci, P. & Deans, K. The appendix and aganglionosis. A note of caution – how the histology can mislead the surgeon in total colonic Hirschsprung disease. Eur. J. Pediatr. Surg. Rep. 3, 3–6 (2015).
167.\ Maia, D. M. The reliability of frozen-section diagnosis in the pathologic evaluation of Hirschsprung’s disease. Am. J. Surg. Pathol. 24, 1675–1677 (2000).
168.\ Shayan, K., Smith, C. & Langer, J. C. Reliability of intraoperative frozen sections in the management of Hirschsprung’s disease. J. Pediatr. Surg. 39, 1345–1348 (2004).
169.\ Langer, J. C. et al. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr. Surg. Int. 33, 523–526 (2017).
170.\ Saadai, P. et al. Guidelines for the management of postoperative soiling in children with Hirschsprung disease. Pediatr. Surg. Int. 35, 829–834 (2019).
171.\ Ahmad, H. et al. A Hirschsprung pull-through, ‘with a twist’. Eur. J. Pediatr. Surg. Rep. 8, e95–e98 (2020).
172.\ Gupta, D. K., Khanna, K. & Sharma, S. Experience with the redo pull-through for Hirschsprung’s disease. J. Indian Assoc. Pediatr. Surg. 24, 45–51 (2019).
173.\ Beltman, L. et al. Transition zone pull-through in patients with Hirschsprung disease: is redo surgery bene icial for the long-term outcomes? J. Pediatr. Surg. https://doi.org/ 10.1016/J.JPEDSURG.2023.02.043 (2023).
174.\ Vickery, J. M., Shehata, B. M., Chang, E. P. & Husain, A. N. Reoperation for Hirschsprung disease: two cases of vanishing ganglion cells and review of the literature. Pediatr. Dev. Pathol. 26, 77–85 (2023).
175.\ Sun, S., Chen, G., Zheng, S., Dong, K. & Xiao, X. Usefulness of posterior sagittal anorectoplasty for redo pull-through in complicated and recurrent Hirschsprung disease: experience with a single surgical group. J. Pediatr. Surg. 52, 458–462 (2017).
176.\ Bokova, E. et al. Reconstructing the anal sphincters to reverse iatrogenic overstretching following a pull-through for Hirschsprung disease. One-year outcomes. J. Pediatr. Surg. 58, 484–489 (2023).
177.\ Chantakhow, S., Tepmalai, K., Singhavejsakul, J., Tantraworasin, A. & Khorana, J. Prognostic factors of postoperative Hirschsprung-associated enterocolitis: a cohort study. Pediatr. Surg. Int. 39, 77 (2023).
178.\ Roorda, D., Oosterlaan, J., van Heurn, E. & Derikx, J. P. M. Risk factors for enterocolitis in patients with Hirschsprung disease: a retrospective observational study. J. Pediatr. Surg. 56, 1791–1798 (2021).
179.\ Menezes, M. & Puri, P. Long-term clinical outcome in patients with Hirschsprung’s disease and associated Down’s syndrome. J. Pediatr. Surg. 40, 810–812 (2005).
180.\ Arnaud, A. P. et al. Di erent fecal microbiota in Hirschsprung’s patients with and without associated enterocolitis. Front. Microbiol. 13, 904758 (2022).
181.\ Pierre, J. F. et al. Intestinal dysbiosis and bacterial enteroinvasion in a murine model of Hirschsprung’s disease. J. Pediatr. Surg. 49, 1242–1251 (2014).
182.\ Gosain, A. et al. Impaired cellular immunity in the murine neural crest conditional deletion of endothelin receptor-B model of Hirschsprung’s disease. PLoS ONE 10, e0128822 (2015).
183.\ Neuvonen, M. I. et al. Bowel function and quality of life after transanal endorectal pull-through for Hirschsprung disease: controlled outcomes up to adulthood. Ann. Surg. 265, 622–629 (2017).
184.\ Davidson, J. R. et al. Long-term surgical and patient-reported outcomes of Hirschsprung disease. J. Pediatr. Surg. 56, 1502–1511 (2021).
185.\ Davidson, J. R. et al. Comparative cohort study of Duhamel and endorectal pull-through for Hirschsprung’s disease. BJS Open 6, zrab143 (2022).
186.\ Stenström, P. et al. Total colonic aganglionosis: multicentre study of surgical treatment and patient-reported outcomes up to adulthood. BJS Open. 4, 943–953 (2020).
187.\ Davidson, J. R. et al. Outcomes in Hirschsprung’s disease with coexisting learning disability. Eur. J. Pediatr. 180, 3499–3507 (2021).
188.\ Vakkilainen, S., Taskinen, M. & Mäkitie, O. Immunode iciency in cartilage–hair hypoplasia: pathogenesis, clinical course and management. Scand. J. Immunol. 92, e12913 (2020).
189.\ Mäkitie, O., Kaitila, I. & Rintala, R. Hirschsprung disease associated with severe cartilage–hair hypoplasia. J. Pediatr. 138, 929–931 (2001).
190.\ Svetano , W. J. et al. Psychosocial factors a ecting quality of life in patients with anorectal malformation and Hirschsprung disease – a qualitative systematic review.
J. Pediatr. Surg. 57, 387–393 (2022).
191.\ Davidson, J. R. et al. Sexual function, quality of life, and fertility in women who had surgery for neonatal Hirschsprung’s disease. Br. J. Surg. 108, E79–E80 (2021).
192.\ Trinidad, S. et al. Long-term male sexual function and fecal incontinence outcomes for adult patients with Hirschsprung disease or anorectal malformation. J. Pediatr. Surg. https://doi.org/10.1016/J.JPEDSURG.2023.04.006 (2023).
193.\ Roberts, K., Brindle, M. & McLuckie, D. Enhanced recovery after surgery in paediatrics: a review of the literature. BJA Educ. 20, 235–241 (2020).
194.\ Neuvonen, M. I. et al. Intestinal microbiota in Hirschsprung disease. J. Pediatr. Gastroenterol. Nutr. 67, 594–600 (2018).
195.\ Neuvonen, M. et al. Lower urinary tract symptoms and sexual functions after endorectal pull-through for Hirschsprung disease: controlled long-term outcomes. J. Pediatr. Surg. 52, 1296–1301 (2017).
196.\ Virtanen, V. B. et al. Thyroid cancer and co-occurring RET mutations in Hirschsprung disease. Endocr. Relat. Cancer 20, 595–602 (2013).
197.\ Granström, A. L., Amin, L., Arnell, H. & Wester, T. Increased risk of in lammatory bowel disease in a population-based cohort study of patients with Hirschsprung disease.
J. Pediatr. Gastroenterol. Nutr. 66, 398–401 (2018).
198.\ Granström, A. L., Ludvigsson, J. F. & Wester, T. Clinical characteristics and validation of diagnosis in individuals with Hirschsprung disease and in lammatory bowel disease. J. Pediatr. Surg. 56, 1799–1802 (2021).
199.\ Sutthatarn, P. et al. Hirschsprung-associated in lammatory bowel disease: a multicenter study from the APSA Hirschsprung disease interest group. J. Pediatr. Surg. 58, 856–861 (2023).
200.\Huang, S. G. et al. Machine learning-based quantitative analysis of barium enema and clinical features for early diagnosis of short-segment Hirschsprung disease in neonate. J. Pediatr. Surg. 56, 1711–1717 (2021).
201.\ Greenberg, A. et al. Automatic ganglion cell detection for improving the eficiency and accuracy of Hirschprung disease diagnosis. Sci. Rep. 11, 3306 (2021).
202.\Shimojima, N. et al. Visualization of the human enteric nervous system by confocal laser endomicroscopy in Hirschsprung’s disease: an alternative to intraoperative histopathological diagnosis? Neurogastroenterol. Motil. 32, e13805 (2020).
203.\Harada, A. et al. Visualization of the human enteric nervous system by probe confocal laser endomicroscopy: a irst real-time observation of Hirschsprung’s disease and allied disorders. BMC Med. Imaging 21, 118 (2021).
204.\Nakazawa-Tanaka, N. et al. Increased enteric neural crest cell di erentiation after transplantation into aganglionic mouse gut. Pediatr. Surg. Int. 39, 29 (2022).
205.\Zhang, L. et al. Cotransplantation of neuroepithelial stem cells with interstitial cells of Cajal improves neuronal di erentiation in a rat aganglionic model. J. Pediatr. Surg. 52, 1188–1195 (2017).
206.\Fattahi, F. et al. Deriving human ENS lineages for cell therapy and drug discovery in Hirschsprung disease. Nature 531, 105–109 (2016).
This is the first description of a human pluripotent stem cell-based platform that can be used both for studying human enteric nervous system development and as a potential cell-based treatment for Hirschsprung disease.
207.\ Smits, R. M. et al. Common needs in uncommon conditions: a qualitative study to explore the need for care in pediatric patients with rare diseases. Orphanet J. Rare Dis. 17, 153 (2022).
Nature Reviews Disease Primers | |
(2023) 9:54 |
18 |
