
- •NEONATAL DERMATOSIS
- •OUTLINE
- •SKIN FUNCTION IN THE NEONATE
- •ECCRINE SWEATING
- •SEBACEOUS GLAND SECRETION
- •PREVELANCE OF NEONATAL DERMATOSIS
- ••Cutaneous manifestations were observed in 90.5% of the newborns.
- ••With respect to mode of delivery, Vaginally delivered neonates showed significant association with
- •TRANSIENT PHYSIOLOGICAL CHANGES
- •VERNIX CASEOSA
- ••Golden yellow staining - Haemolytic disease of the newborn and postmaturity.
- •FUNCTIONS
- •PERIPHERAL CYANOSIS/ ACROCYANOSIS
- ••The cyanotic hue disappears on warming the extremities.
- •HARLEQUIN COLOUR CHANGE
- ••Wide variation in the duration of attacks, but generally between 30 seconds- 20
- ••As skin matures, this vascular phenomena disappears.
- •CUTIS MARMORATA
- •MONGOLIAN SPOT
- ••Cause-arrested embryonal migration of melanocytes from neural crest to epidermis resulting in dermal
- ••Lesions also occur on the buttocks, dorsal trunk and extremities.
- •SEBACEOUS GLAND HYPERPLASIA
- •SEBACEOUS GLAND HYPERPLASIA
- •MILIA
- •MILIA
- •PALATE-EPSTEIN’S PEARL
- •DESQUAMATION (PHYSIOLOGICAL SCALING OF
- •MACULAR HEMANGIOMA
- •MINIATURE PUBERTY
- ••Scrotal hyperpigmentation and labial hypertrophy-most common findings in miniature puberty .
- ••Enlargement of breast tissue with thick milk-like secretion (witch’s milk) may be seen.
- •SUCKING BLISTERS
- •NEONATAL OCCIPITAL ALOPECIA
- ••The roots in the occipital area do not enter telogen until term, therefore
- •NEONATAL ACNE/ NEONATAL CEPHALIC
- •No additional treatment is needed -usually resolves spontaneously within four months without scarring.
- •LANUGO
- •ANETODERMA OF PREMATURITY
- ••It is non progressive and persistent.
- •SKIN DISORDERS IN THE NEONATE
- •ERYTHEMA TOXICUM NEONATORUM
- ••Commonly seen-term infants, rare in preterm and low birth weight infants.
- ••Could be an innate immune response of a newborn infant to commensal microbes
- •Diagnosis :
- •TRANSIENT NEONATAL PUSTULAR MELANOSIS
- ••It is transient, benign, self-limiting dermatoses of unknown aetiology characterised by 3 types
- •One hour after birth, flaccid vesiculopustules and superficial erosions with minimal surrounding erythema
- •MILIARIA
- ••Miliaria rubra and miliaria crystallina-common in neonates.
- •MILIARIA CRYSTALLINA
- ••Delicate and generally rupture within 24 hr, and are followed by bran-like desquamation.
- •MILIARIA RUBRA (‘PRICKLY HEAT’)
- ••Lesions occur in -flexural areas, especially around the neck and in the groins
- ••Frequently, some lesions are pustular (miliaria pustulosa), but this does not necessarily indicate
- •Management
- •DIAPER DERMATITIS (NAPKIN DERMATITIS OR
- •Three common types of diaper dermatitis are are -
- •Treatment :
- •APLASIA CUTIS CONGENITA
- ••Aplasia cutis congenita may be associated with under lying embryologic malformations like
- •BACTERIAL INFECTIONS
- ••Common skin problems seen in neonates in India.
- •IMPETIGO
- ••Varnish coloured crust is seen.
- •When bullae spread, rupture, and involve large areas, infection may spread systemically, causing
- •DIAGNOSIS :
- •STAPHYLOCOCCAL SCALDED SKIN SYNDROME(SSSS)
- ••The site of blister cleavage is the granular layer.
- ••The first sign of the disease - faint, macular, orange red, scarlatiniform eruption
- •TREATMENT :
- •OMPHALITIS
- •ECTHYMA GANGRENOSUM
- ••Predisposing factors- prematurity, renal failure, neutropenia and immunodeficiencies, necrotizing enterocolitis and bowel surgery.
- •VIRAL INFECTIONS
- •NEONATAL HERPES SIMPLEX
- ••The skin lesions appear between days 2 and 20.
- ••During an intrauterine infection, vesicles appear within 1 day of life.
- •Neonatal herpes simplex showing congenital ulceration and scarring at 10 days.
- •DIAGNOSIS
- •FETAL VARICELLA SYNDROME
- •Pregnant women who are not immune (on the basis of history, and, preferably,
- •FUNGAL INFECTIONS
- •NEONATAL CANDIDIASIS
- ••White, “flaky,” creamy patches are seen on the tongue and mucous membranes of
- ••In the surrounding normal skin there may be punctate erythematous lesions, sometimes pustular
- •CONGENITAL CANDIDIASIS
- ••Palmar and plantar pustules are regarded as a hallmark of congenital cutaneous candidiasis
- •Congenital candidiasis in a neonate born at 24 weeks’ gestation. Note the “burn-like”
- •DISORDERS CAUSED BY TRANSPLACENTAL
- •NEONATAL PEMPHIGUS VULGARIS
- ••No treatment is required as the lesions have resolved spontaneously within about 3
- •NEONATAL LUPUS ERYTHEMATOSUS
- ••It occurs in neonates up to 3 months old.
- ••A ‘spectacle like’ distribution of lesions around the eyes is especially characteristic.
- •Pathology
- ••Infants generally show little sign of residual disease after the age of 1
- •GENODERMATOSIS
- •SOURCE-IADVL
- •MISCELLANEOUS DISORDERS
- •COLLODION BABY
- ••Almost 90% of collodion babies will go on to develop a severe form
- ••Within hours, this membrane
- •MANAGEMENT
- •REFERENCES
•Infants generally show little sign of residual disease after the age of 1 year.
Management
•The skin lesions of neonatal LE require no treatment, but sun protection is essential.
•Up to 50% of infants with cardiac involvement will require a pacemaker.
•Treatment with high dose systemic steroids may be indicated for fetal bradycardia where there are signs of heart failure.
104
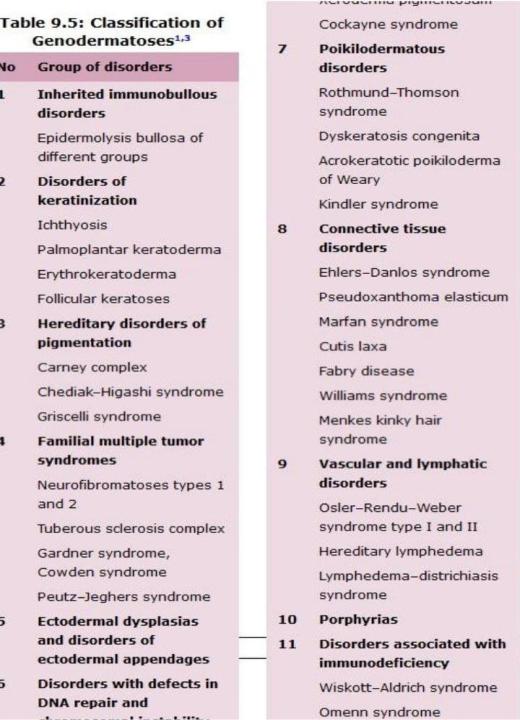
GENODERMATOSIS
•They are inherited skin conditions,majority are lifelong
•A/W- high morbidity due to incurable nature
•Patterns of inheritance-AD,AR,XLD,XLR
•Management- symptomatic
105
SOURCE-IADVL |
106 |
MISCELLANEOUS DISORDERS
• Colloidion baby
107
COLLODION BABY
•Highly characteristic clinical entity present at birth where a child is born with an ‘extra’ skin resembling a shiny membrane or collodion.
•The severely affected infant is bright red and encased in a taut, glistening, yellowish, translucent covering resembling collodion.
108
•Almost 90% of collodion babies will go on to develop a severe form of autosomal recessive ichthyosis in the first few weeks of life:
-lamellar ichthyosis
-non bullous ichthyosiform erythroderma (syn. congenital ichthyosiform erythroderma)
109

•Within hours, this membrane
dries and cracks, and bleeding may occur Within 1 or 2 days, it starts to peel off
The shedding will more or less complete within 4 weeks Subsequently, the typical features of one of several varieties of ichthyosis gradually emerge over a period of weeks or months.
110
MANAGEMENT
•Incubation in a high humidity atmosphere, with careful monitoring of body temperature.
•Fluid and electrolyte balance.
•Fluid loss is significantly reduced by frequent applications of lipid, a mixture of white soft paraffin and liquid paraffin is ideal.
•Frequent oiling.
111
REFERENCES
•ROOK’S TEXTBOOK OF DERMATOLOGY
•HARPER’S TEXTBOOK OF PAEDIATRIC DEMATOLOGY
•IADVL TEXTBOOK OF DERMATOLOGY 4th edition
•Neonatal Dermatoses and knowledge, attitude, practice of postnatal mothers from South India(Neha Sharma, Jayadev Betkerur, LSS Manickam)
112
