
Lesson topic №21 Синдром артериальной гипертензии (Arterial hypertension in the outpatient setting) (1)
.pdf
ANTIHYPERTENSIVE TREATMENT
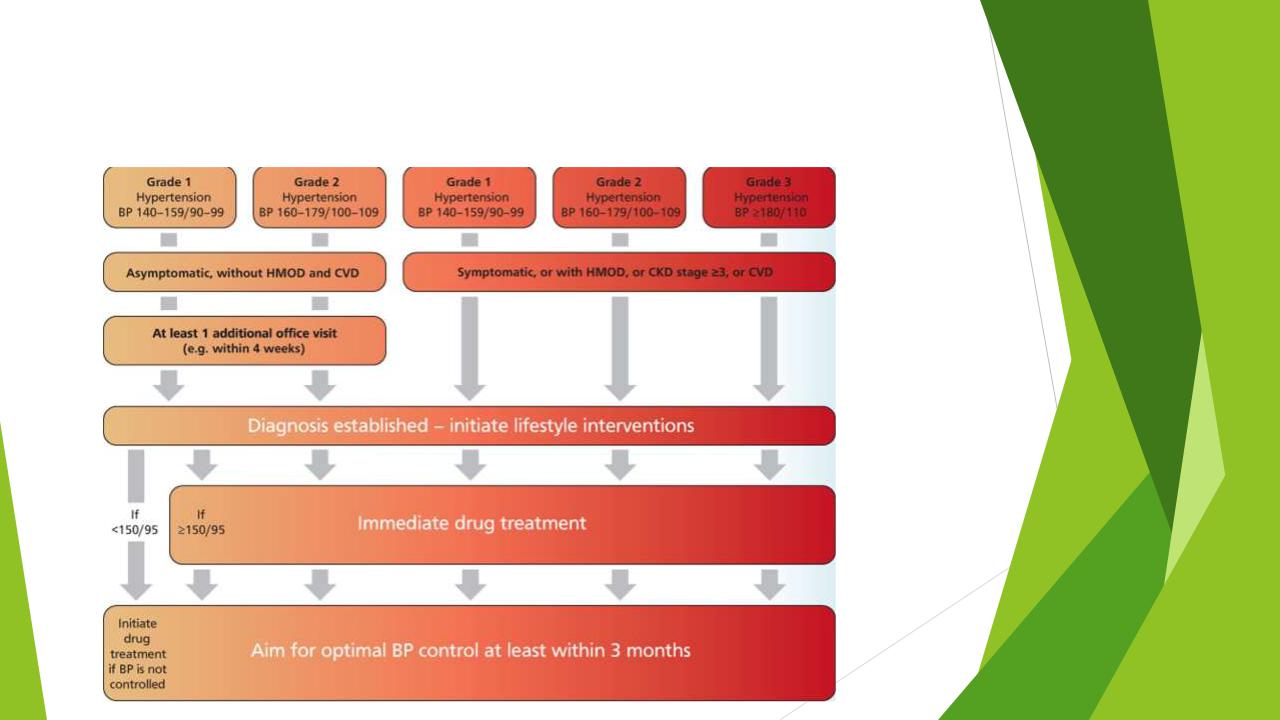
All guidelines agree that patients with grade 2 or 3 hypertension should be offered antihypertensive drug treatment alongside lifestyle interventions.
Patients with grade 1 hypertension and a high CV risk should also be treated both via lifestyle modifications and BP-lowering drugs.
In patients with grade 1 hypertension in its lower BP range, no HMOD and a low CV risk, the possibility may be considered to start treatment with lifestyle changes only. If BP control is not achieved within a few months of a lifestyle-based approach, drug treatment will be necessary.
ANTIHYPERTENSIVE TREATMENT
ANTIHYPERTENSIVE TREATMENT

ANTIHYPERTENSIVE TREATMENT
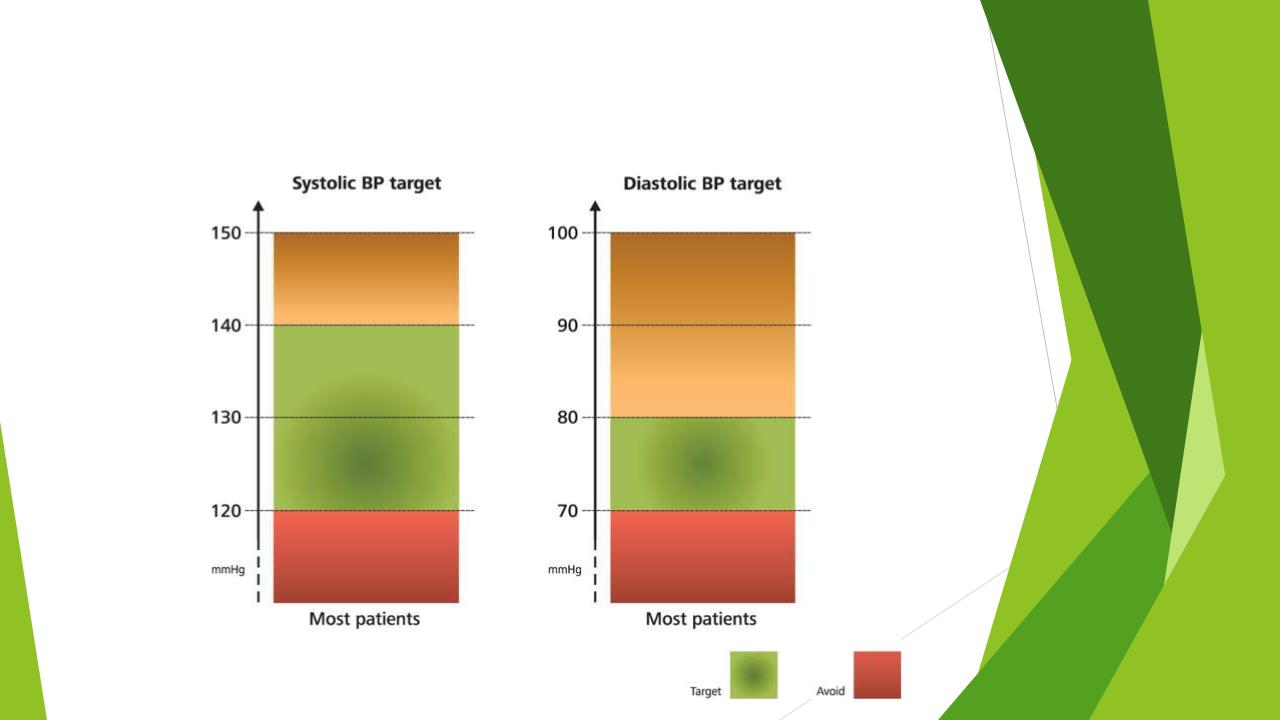
The first objective of antihypertensive treatment should be to lower BP to <140/80 mmHg in most patients.
If drug treatment is well tolerated, treated SBP values should be targeted to 130 mmHg or lower in most patients up to 79 years old.
Despite the smaller incremental benefit, an effort should be made to reach a BP range of 120–129/70–79 mmHg in patients up to 79 years old, but only if treatment is well tolerated.
In patients at least 80 years old who are not frail, the first objective of antihypertensive treatment is to lower BP below 150/80 mmHg. However, a SBP target range between 130-139 mmHg may be considered, if well tolerated.

ANTIHYPERTENSIVE TREATMENT
Five major drug classes are recommended as first-line agents for the treatment of hypertension i.e. angiotensin-converting-enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), calcium channel blockers (CCB), Thiazide/Thiazide-like diuretics and beta blockers (BBs).
The use of an RAS inhibitor (ACEi or ARB), if not contraindicated, is considered as a common component of the general combination treatment strategy.
The use of BBs is restricted to special clinical conditions or situations.

Compelling contraindications and conditions requiring cautious use of BP-lowering drugs
Drug class |
Contraindications |
Cautious use |
|
|
|
ACEi |
Pregnancy |
Women of child-bearing potential |
|
|
without reliable contraception |
|
|
|
|
Women planning pregnancy |
|
|
|
|
|
Previous angioneurotic edema |
|
|
|
|
|
Severe hyperkalemia (e.g. potassium >5.5 |
|
|
mmol/l) |
|
|
|
|
|
Bilateral renal artery stenosis or stenosis in |
|
|
solitary (functional) kidney |
|
|
|
|
ARB |
Pregnancy |
Women of child-bearing potential |
|
|
without reliable contraception |
|
|
|
|
Women planning pregnancy |
|
|
|
|
|
Severe hyperkalemia (e.g. potassium >5.5 |
|
|
mmol/l) |
|
|
|
|
|
Bilateral renal artery stenosis or stenosis in |
|
|
solitary (functional) kidney |
|
|
|
|

Compelling contraindications and conditions requiring cautious use of BP-lowering drugs
Drug class |
Contraindications |
Cautious use |
|
|
|
Beta-blocker |
Asthma |
Glucose intolerance |
|
|
|
|
Any high-grade sino-atrial or atrioventricular |
Athletes and physically active patients |
|
block |
|
|
|
|
|
Bradycardia (e.g. heart rate <60 bpm) |
|
|
|
|
DHP-CCB |
|
Tachyarrhythmia |
|
|
|
|
|
Heart failure (HFrEF, class III or IV) |
|
|
|
|
|
Preexisting severe leg edema |
|
|
|
Non-DHP- |
Any high-grade sino-atrial or AV block |
Constipation |
CCB (verapamil, |
|
|
diltiazem) |
|
|
|
|
|
|
Severe LV dysfunction (LV EF <40%), HFrEF |
|
|
|
|
|
Bradycardia (e.g. heart rate <60 bpm) |
|
|
|
|
|
Co-medications susceptible to significant drug |
|
|
interactions mediated by P-gp or CYP3A4 |
|
|
|
|

Compelling contraindications and conditions requiring cautious use of BP-lowering drugs
Drug class |
Contraindications |
Cautious use |
|
|
|
Thiazide/T |
Hyponatremia |
Glucose intolerance |
hiazide-like |
|
|
diuretics |
|
|
|
|
|
|
CKD due to obstructive uropathy |
Pregnancy |
|
|
|
|
Sulfonamide allergies |
Hypercalcemia |
|
|
|
|
Gout |
Hypokalemia |
|
|
|
|
|
Cancer patients with bone |
|
|
metastasis |
|
|
|
Mineralocor |
Severe hyperkalemia (e.g. potassium |
Co-medications susceptible to |
ticoid |
>5.5 mmol/l) |
significant drug interactions |
receptor |
|
mediated by P-gp or CYP3A4 |
antagonist |
|
for eplerenone |
|
|
|
|
eGFR <30 ml/min/1.73 m2 |
|

Angiotensin-converting-enzyme inhibitors
ACEis are among the most widely used classes of antihypertensive drugs. Because of their earlier availability and, thus, their earlier evaluation against placebo in outcome-based randomized controlled
trials (RCT), knowledge about ACEis is based on a large amount
of RCT data, particularly in patients with HF, CAD and at high CV risk.
ACEis are associated with an increased risk of a very rare event such as angioneurotic edema, especially in people of Black African origin.
They are associated with a cough that affects about 5–10% of treated patients with a greater frequency in women and patients of Asian origin.

Angiotensin receptor blockers
ARBs have a similar antihypertensive efficacy and protective effect as ACEis, albeit with a somewhat different mechanism for RAS inhibition.
A difference between ACEis and ARBs is their tolerability profile, with ARBs having a rate of side effects similar to placebo.
