
Lesson topic №21 Синдром артериальной гипертензии (Arterial hypertension in the outpatient setting) (1)
.pdf
Comprehensive physical examination for hypertension
Body habitus
Weight and height measured on a calibrated scale, with calculation of BMI
Waist circumference

Comprehensive physical examination for hypertension
Signs of hypertension-mediated organ damage
Neurological examination and cognitive status
Fundoscopic examination for hypertensive retinopathy in emergencies
Auscultation of heart and carotid arteries
Palpation of carotid and peripheral arteries
Ankle–brachial index

Comprehensive physical examination for hypertension
Signs of secondary hypertension
Skin inspection: cafe-au-lait patches of neurofibromatosis (pheochromocytoma)
Kidney palpation for signs of renal enlargement in polycystic kidney disease
Auscultation of heart and renal arteries for murmurs or bruits indicative of aortic coarctation, or renovascular hypertension
Signs of Cushing's disease or acromegaly
Signs of thyroid disease

Selected standard laboratory tests for work-up of hypertensive patients
Hemoglobin and/or hematocrit
Fasting blood glucose/HbA1c
Blood lipids: total cholesterol, LDL cholesterol, HDL cholesterol, triglycerides
Blood creatinine (and/or cystatin C) for estimating glomerular filtration rate (GFR)
Blood uric acid
Blood potassium and sodium
Urine analysis (first voided urine in the morning), multicomponent dipstick test in all patients, urinary albumin/creatinine ratio, microscopic examination in selected patients

Other investigations in hypertension
Screening tests |
Aim |
|
|
12 lead ECG |
Measure HR and AV conduction, detect |
|
cardiac arrhythmias, myocardial |
|
ischemia and infarction, screen for LVH |
|
|
Echocardiography |
Evaluate structure and function of the |
|
ventricles and left atrium, detect |
|
valvular disease, aortic root diameter |
|
and ascending aortic aneurysm |
|
|
Carotid artery ultrasound |
Determine carotid intima-media |
|
thickness, plaque and stenosis |
|
|
Kidney ultrasound |
Evaluate size and structure of kidney, |
|
detect renovascular disease, determine |
|
renal resistive index (RRI) (by spectral |
|
doppler ultrasonography) |
|
|
Retina microvasculature |
Detect microvascular changes |
|
|

SECONDARY HYPERTENSION
Secondary forms of hypertension account for only a small fraction of the overall hypertension prevalence
Despite their limited prevalence, detection and management of secondary forms of hypertension is of utmost importance, because these forms often carry a high or very-high risk of morbidity and mortality and can possibly be cured by timely treatment of their cause
Secondary forms of hypertension are a frequent cause of severe or trueresistant hypertension, worsening of previously controlled hypertension or increased severity of HMOD, which may appear as disproportionate to the duration of hypertension
SECONDARY HYPERTENSION
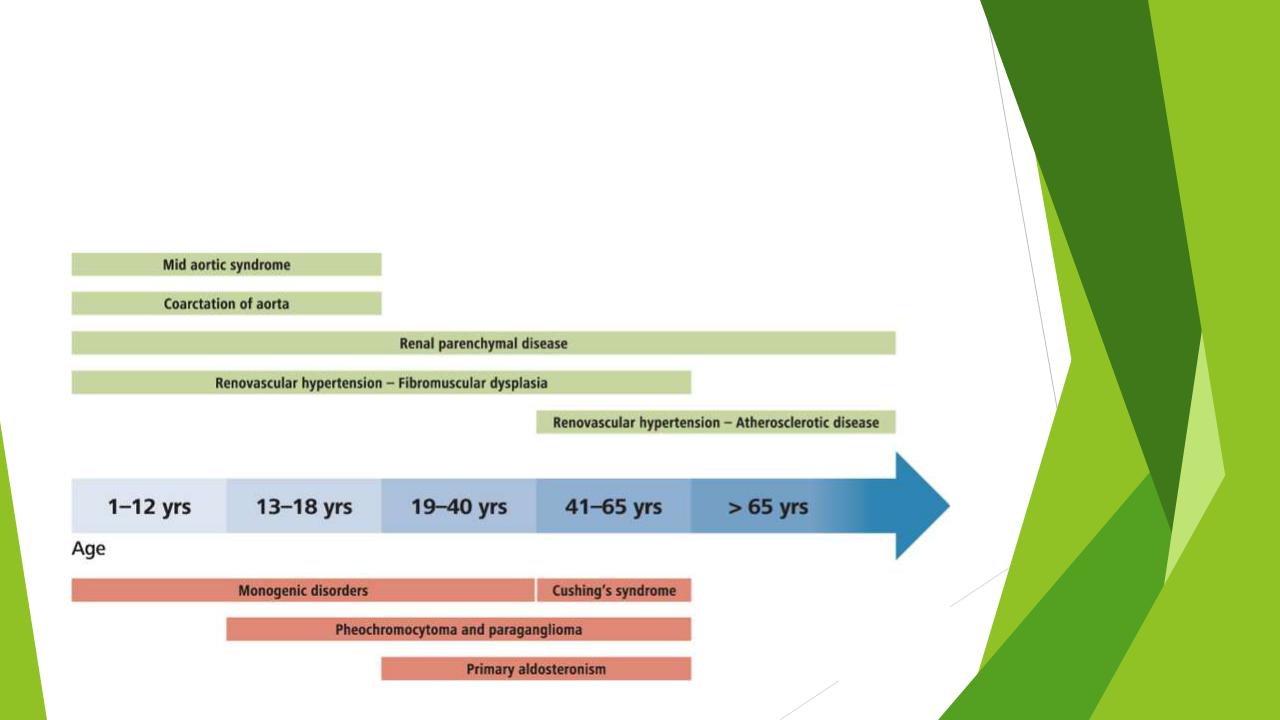
Incidence of selected forms of secondary hypertension according to age

Patient characteristics that should raise the suspicion of secondary hypertension
Younger patients (<40 years) with grade 2 or 3 hypertension or hypertension of any grade in childhood
Sudden onset of hypertension in individuals with previously documented normotension
Acute worsening of BP control in patients with previously well controlled by treatment
True resistant hypertension hypertension
Hypertensive emergency
Severe (grade 3) or malignant hypertension
Severe and/or extensive HMOD, particularly if disproportionate for the duration and severity of the BP elevation
Clinical or biochemical features suggestive of endocrine causes of hypertension
Clinical features suggestive of renovascular hypertension or fibromuscular dysplasia
Clinical features suggestive of obstructive sleep apnea
Severe hypertension in pregnancy (>160/110 mmHg) or acute worsening of BP control in pregnant women with preexisting hypertension

LIFESTYLE INTERVENTIONS
Smoking cessation
Weight reduction
should ideally be achieved through a combination of a low-caloric diet and exercise Increase levels of daily physical activity and regular exercise
The acute pressor effect of dynamic and isometric exercise does not contraindicate regular exercise on a chronic basis. Recommended minimum physical activity level of 150 min per week. Moderate-intensity aerobic exercise (40–60% heart rate reserve) is recommended to prevent and treat hypertension
Restriction of sodium intake
Augmentation of dietary potassium intake
Moderation of alcohol intake

Smoking cessation
Tobacco smoking is the single largest preventable cause of death and is known to significantly increase the risk of CVD.
Attention should also be given to passive exposure to smoking, which has been associated with the risk of CVD and a 24 h BP elevation.
In recent decades, water pipe smoking has developed into a major and rapidly growing alternative to traditional tobacco smoking within the global tobacco epidemic. The few available studies showed no clear difference in the CV disease incidence between waterpipe smoking and traditional tobacco smokers.
E-cigarettes originally marketed as potential aids in smoking cessation, have attracted a lot of consumers. Recent meta-analyses now highlight that these
‘so-called safer’ alternatives acutely increase BP, heart rate and may also be associated with increased risk of CV disease.
