
Книги по МРТ КТ на английском языке / Advanced Imaging of the Abdomen - Jovitas Skucas
.pdf
679
KIDNEYS AND URETERS
10.Neri E, Boraschi P, Caramella D, et al. Magnetic resonance virtual endoscopy of the upper urinary tract. AJR 2000;175:1697–1702.
11.Rybicki FJ, Shu KM, Cibas ES, Fielding JR, vanSonnenberg E, Silverman SG. Percutaneous biopsy of renal masses: sensitivity and negative predictive value stratified by clinical setting and size of masses. AJR 2003;180:1281–1287.
12.Preda A,Van Dijk LC,Van Oostaijen JA, Pattynama PM. Complication rate and diagnostic yield of 515 consecutive ultrasound-guided biopsies of renal allografts and native kidneys using a 14-gauge Biopty gun. Eur Radiol 2003;13:527–530.
13.Cluzel P, Martinez F, Bellin MF, et al. Transjugular versus percutaneous renal biopsy for the diagnosis of parenchymal disease: comparison of sampling effectiveness and complications. Radiology 2000;215: 689–693.
14.Hogan MJ, Coley BD, Jayanthi VR, Shiels WE, Koff SA. Percutaneous nephrostomy in children and adolescents: outpatient management. Radiology 2001;218: 207–210.
15.Patel U, Hussain FF. Percutaneous nephrostomy of nondilated renal collecting systems with fluoroscopic guidance: technique and results. Radiology 2004;233: 226–233.
16.Caire JT, Ramus RM, Magee KP, Fullington BK, Ewalt DH, Twickler DM. MRI of fetal genitourinary anomalies. AJR 2003;181:1381–1385.
17.Choi JY, Kim SH, Kim SH. Double-blind ureteral duplication: report of two cases. Eur Radiol 2002;12 Suppl 3:S136–139.
18.Wikstrom M, Hauger W, Sinagowitz E. [A triple ureter with an ectopic opening into the vagina.] [Review] [German] Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 1999;171:497–498.
19.Zerin JM, Leiser J. The impact of vesicoureteral reflux on contralateral renal length in infants with multicystic dysplastic kidney. Pediatr Radiol 1998;28:683– 686.
20.Feather SA, Winyard PJ, Dodd S, Woolf AS. Oral- facial-digital syndrome type 1 is another dominant polycystic kidney disease: clinical, radiological and histopathological features of a new kindred. Nephrol Dial Transplant 1997;12:1354–1361.
21.Hateboer N, v Dijk MA, Bogdanova N, et al. Comparison of phenotypes of polycystic kidney disease types 1 and 2. European PKD1–PKD2 Study Group. Lancet 1999;353:103–107.
22.Nicolau C, Torra R, Badenas C, et al. Autosomal dominant polycystic kidney disease types 1 and 2: assessment of US sensitivity for diagnosis. Radiology 1999; 213:273–276.
23.Neumann HP, Bender BU, Berger DP, et al. Prevalence, morphology and biology of renal cell carcinoma in von Hippel-Lindau disease compared to sporadic renal cell carcinoma. J Urol 1998;160:1248–1254.
24.Dondi M, Fanti S, Monetti N. Bartter’s syndrome: renal scintigraphic appearance after captopril administration. J Nucl Med 1996;37:1688–1690.
25.Forget S, Patriquin HB, Dubois J, et al. The kidney in children with tyrosinemia: sonographic, CT and biochemical findings. Pediatr Radiol 1999;29:104– 108.
26.Moore EE, Cogbill TH, Malangoni MA, et al. Organ injury scaling. [Review] Surg Clin North Am 1995; 75:293–303.
27.Dacher JN, Avni F, Francois A, et al. Renal sinus hyperechogenicity in acute pyelonephritis: description and pathological correlation. Pediatr Radiol 1999;29:179– 182.
28.Laguna R, Silva F, Orduna E, Conway JJ, Weiss S, Calderon C. Technetium-99m-MAG3 in early identification of pyelonephritis in children. J Nucl Med 1998; 39:1254–1257.
29.Lonergan GJ, Pennington DJ, Morrison JC, Haws RM, Grimley MS, Kao TC. Childhood pyelonephritis: comparison of gadolinium-enhanced MR imaging and renal cortical scintigraphy for diagnosis. Radiology 1998;207:377–384.
30.Kuo YT, Chen MT, Liu GC, Huang CN, Huang CL, Huang CH. Emphysematous pyelonephritis: imaging diagnosis and follow-up. Kao-Hsiung I Chih 1999;15: 159–170.
31.el Fakir Y, Kabbaj N, Dafiri R, Imani F. [Imaging of urinary Candida bezoars.] [French] Prog Urol 1999;9:513–517.
32.el Khader K, Lrhorfi MH, el Fassi J, Tazi K, Hachimi M, Lakrissa A. [Urogenital tuberculosis. Experience in 10 years.] [French] Prog Urol 2001;11:62–67.
33.Kirchner TH, Kirchner J, Jacobi V. [Renal parenchymal defects as signs of renal tuberculosis.] [German] Rontgenpraxis 2000;52:332–234.
34.Yagi S, Goto T, Kawamoto K, et al. Endoscopic treatment of refractory filarial chyluria: a preliminary report. J Urol 1998;159:1615–1618.
35.Weber MA, Wasser K, Schwenger V, Hallscheidt P, Nahm AM, Delorme S. [Palpable resistance in the right renal area. Xanthogranulomatous pyelonephritis with fistulization in the colon ascendens and M. psoas major.] [German] Radiologe 2002;42:46–50.
36.Leluc O, Andre M, Marciano S, Lafforgue P, Rossi D, Bartoli J. [Retroperitoneal complications of ErdheimChester disease.] [French] J Radiol 2001;82:580–582.
37.Schmidt T, Hohl C, Haage P, et al. Diagnostic accuracy of phase-inversion tissue harmonic imaging versus fundamental B-mode sonography in the evaluation of focal lesions of the kidney. AJR 2003;180:1639–1647.
38.Tello R, Davison BD, O’Malley M, et al. Magnetic resonance imaging of renal masses interpreted on CT to be suspicious. AJR 2000;174:1017–1022.
39.Bain ES, Kinney TB, Gooding JM, Casola G,Ysrael MZ. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): a rare cause of bilateral renal masses. AJR 1999;172:995–996.
40.Townsend MF 3rd, Gal AA, Thoms WW, Newman JL, Eble JN, Graham SD Jr. Ureteral rhabdomyosarcoma. Urology 1999(online);54:561.
41. Johraku A, Miyanaga N, Sekido N, et al. A case of intravascular papillary endothelial hyperplasia (Masson’s tumor) arising from renal sinus. Jpn J Clin Oncol 1997;27:433–436.
42.Bosniak MA. The use of the Bosniak classification system for renal cysts and cystic tumors. J Urol 1997;157:1852–1853.
43.Curry NS, Cochran ST, Bissada NK. Cystic renal masses: accurate Bosniak classification requires adequate renal CT. AJR 2000;175:339–342.
680
ADVANCED IMAGING OF THE ABDOMEN
44.Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology 2004;231:365–371.
45.Chung EP, Herts BR, Linnell G, et al. Analysis of changes in attenuation of proven renal cysts on different scanning phases of triphasic MDCT. AJR 2004;182:405–410.
46.Bae KT, Heiken JP, Siegel CL, Bennett HF. Renal cysts: is attenuation artifactually increased on con- trast-enhanced CT images? Radiology 2000;216:792– 796.
47.Macari M, Bosniak MA. Delayed CT to evaluate renal masses incidentally discovered at contrastenhanced CT: demonstration of vascularity with deenhancement. Radiology 1999;213:674–680.
48.Slywotzky CM, Bosniak MA. Localized cystic disease of the kidney. AJR 2001;176:843–849.
49.Storkel S, van den Berg E. Morphological classification of renal cancer. World J Urol 1995;13:153–158.
50.Kovacs G,Akhtar M, Beckwith BJ, et al. The Heidelberg classification of renal cell tumours. [Review] J Pathol 1997;83:131–133.
51.Kim JK, Kim TK, Ahn HJ, Kim CS, Kim KR, Cho KS. Differentiation of subtypes of renal cell carcinoma on helical CT scans. AJR 2002;178:1499–1506.
52.Toro JR, Glenn G, Duray P, et al. Birt-Hogg-Dube syndrome: a novel marker of kidney neoplasia. Arch Dermatol 1999;135:1195–1202.
53.Brauch H, Weirich G, Hornauer MA, Storkel S, Wohl T, Bruning T. Trichloroethylene exposure and specific somatic mutations in patients with renal cell carcinoma. J Nat Cancer Inst 1999;91:854–661.
54.Ligato S, Ro JY, Tamboli P, Amin MB, Ayala AG. Benign tumors and tumor-like lesions of the adult kidney. Part I: Benign renal epithelial neoplasms. Adv Anat Pathol 1999;6:1–11.
55.Ascenti G, Gaeta M, Magno C, et al. Contrast-enhanced second-harmonic sonography in the detection of pseudocapsule in renal cell carcinoma. AJR 2004;182: 1525–1530.
56.Scialpi M, Di Maggio A, Midiri M, Loperfido A, Angelelli G,Rotondo A. Small renal masses: assessment of lesion characterization and vascularity on dynamic contrast-enhanced MR imaging with fat suppression. AJR 2000;175:751–757.
57.Yoshimitsu K, Honda H, Kuroiwa T, et al. Magnetic resonance detection of cytoplasmic fat in clear cell renal cell carcinoma utilizing chemical shift gradientecho imaging. J Magn Reson Imaging 1999;9:579– 585.
58.Schubert RA, Schleicher C, Mentzel HJ, Wunderlich H, Schubert J, Kaiser WA. [The observed and chancecorrected agreement of the computed tomographic and histological staging results in renal-cell carcinoma.] [German] Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 1999;170:358–364.
59.Ergen FB, Hussain HK, Caoili EM, et al. MRI for
preoperative staging of renal cell carcinoma using the 1997 TNM classification: comparison with surgical and pathologic staging. AJR 2004;182:217– 225.
60.Lebret T, Becette V, Colau A, et al. [Study of the Ki-67 antibody immunolabeling of renal adenocarcinomas
with or without renal vein thrombosis.] [French] Prog Urol 1999;9:649–654.
61.Remer EM, Weinberg EJ, Oto A, O’Malley CM, Gill IS. Magnetic resonance imaging of the kidneys after laparoscopic cryoablation. AJR 2000;174:635–640.
62.Mayo-Smith WW, Dupuy DE, Parikh PM, Pezzullo JA, Cronan JJ. Imaging-guided percutaneous radiofrequency ablation of solid renal masses: techniques and outcomes of 38 treatment sessions in 32 consecutive patients. AJR 2003;180:1503–1508.
63.Lewin JS, Nour SG, Connell CF, et al. Phase II clinical trial of interactive MR imaging-guided interstitial radiofrequency thermal ablation of primary kidney tumors: initial experience. Radiology 2004;232:835– 845.
64.McLaughlin CA, Chen MY, Torti FM, Hall MC, Zagoria RJ. Radiofrequency ablation of isolated local recurrence of renal cell carcinoma after radical nephrectomy. AJR 2003;181:93–94.
65.Hafez KS, Novick AC, Campbell SC. Patterns of tumor recurrence and guidelines for followup after nephron
sparing surgery for sporadic renal cell carcinoma. J Urol 1997;157:2067–2070.
66.Quaia E, Siracusano S, Bertolotto M, Monduzzi M, Mucelli RP. Characterization of renal tumours with pulse inversion harmonic imaging by intermittent high mechanical index technique: initial results. Eur Radiol 2003;13:1402–1412.
67.Shishikura Y, Furusato M, Aizawa S. Cystic renal cell carcinoma: arose as a simple cyst, recurred repeatedly as a multicystic mass and finally presented as a solid mass. Pathol Int 1998;48:623–628.
68.Mahnken AH, Wildberger JE, Bergmann F, Fuzesi L, Adam G, Gunther R. [Papillary renal cell carcinoma: comparison of CT and gross morphology.] [German] Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 2000;172:1011–1015.
69.Lesavre A, Correas JM, Merran S, Grenier N,Vieillefond A, Helenon O. CT of papillary renal cell carcinomas with cholesterol necrosis mimicking angiomyolipomas. AJR 2003;181:143–145.
70.Sijmons RH, Kiemeney LA, Witjes JA, Vasen HF. Urinary tract cancer and hereditary nonpolyposis colorectal cancer: risks and screening options. J Urol 1998;160:466–470.
71.Kitamura Y, Watanabe M, Komatsubara S, Sakata Y, Miyajima N. [Regional lymph node metastasis in renal pelvic or ureteral cancer.] [Japanese] Nippon Hinyokika Gakkai Zasshi 1998;89:522–528.
72.Van Glabeke E, Chartier-Kastler E, Delcourt A, Cluzel P, Bruel S, Richard F. [Epidermoid cancer of the kidney pelvis.] [French] Prog Urol 2000;10:1200– 1203.
73.Rohrschneider WK, Weirich A, Rieden K, Darge K, Troger J, Graf N. US, CT and MR imaging characteristics of nephroblastomatosis. Pediatr Radiol 1998;28: 435–443.
74.Kumar R, Fitzgerald R, Breatnach F. Conservative surgical management of bilateral Wilms tumor: results of the United Kingdom Children’s Cancer Study Group. J Urol 1998;160:1450–1453.
75.Jeanes AC, Beese RC, McHugh K, Ramsay AD. Fatty degeneration in a Wilms’ tumour after chemotherapy. Eur Radiol 2002;12 Suppl 3:S149–151.

681
KIDNEYS AND URETERS
76.Isaac MA, Vijayalakshmi S, Madhu CS, Bosincu L, Nogales FF. Pure cystic nephroblastoma of the ovary with a review of extrarenal Wilms’ tumors. [Review] Hum Pathol 2000;31:761–764.
77.Eble JN, Bonsib SM. Extensively cystic renal neoplasms: cystic nephroma, cystic partially differentiated nephroblastoma, multilocular cystic renal cell carcinoma, and cystic hamartoma of renal pelvis. [Review] Semin Diagn Pathol 1998;15:2–20.
78.Nagao T, Sugano I, Ishida Y, et al. Cystic partially differentiated nephroblastoma in an adult: an immunohistochemical, lectin histochemical and ultrastructural study. Histopathology 1999;35:65–73.
79.Pages A, Granier M. [Nephronogenic nephroma (author’s transl).] [French] Arch Anat Cytol Pathol 1980;28:99–103.
80.Renshaw AA, Freyer DR, Hammers YA. Metastatic metanephric adenoma in a child. Am J Surg Pathol 2000;24:570–574.
81.Keshani de Silva V, Tobias V, Kainer G, Beckwith B. Metanephric adenoma with embryonal hyperplasia of Bowman’s capsular epithelium: previously unreported association. Pediatr Dev Pathol 2000;3:472–478.
82.Argani P, Beckwith JB. Metanephric stromal tumor: report of 31 cases of a distinctive pediatric renal neoplasm. Am J Surg Pathol 2000;24:917–926.
83.Sakhuja V, Jha V, Varma S, et al. Renal involvement in multiple myeloma: a 10–year study. Ren Fail 2000;22: 465–477.
84.Burdeny DA, Semelka RC, Kelekis NL, Reinhold C, Ascher SM. Small (<1.5cm) angiomyolipomas of the kidney: characterization by the combined use of inphase and fat-attenuated MR techniques. Magn Reson Imaging 1997;15:141–145.
85.Lee W, Kim TS, Chung JW, Han JK, Kim SH, Park JH. Renal angiomyolipoma: embolotherapy with a mixture of alcohol and iodized oil. J Vasc Interv Radiol 1998;9: 255–261.
86.Haddad FS, de la Vega DJ, DuBose Dent E Jr, Shippel RM. Renal fibrohistiocytic sarcoma. Three cases and a review of the literature. [Review] J Med Liban 1998;46: 335–342.
87.Tsurukawa H, Iuchi H, Osanai H, et al. [Renomedullary interstitial cell tumor: a case report.] [Review] [Japanese] Nippon Hinyokika Gakkai Zasshi 2000;91: 37–40.
88.Tajima K, Saito K, Umeda Y, Murata T, Satani H. Malignant melanoma of the kidney presenting as a primary tumor. Int J Urol 1997;4:94–96.
89.Soulie M, Escourrou G, Vazzoler N, et al. [Primary carcinoid tumor and horseshoe kidney: potential association.] [French] Prog Urol 2001;11:301–303.
90.Georgiades CS, Moore CJ, Smith DP. Differences of renal parenchymal attenuation for acutely obstructed and unobstructed kidneys on unenhanced helical CT: a useful secondary sign? AJR 2001;76:965–968.
91.Garcia-Pena BM, Keller MS, Schwartz DS, Korsvik HE, Weiss RM. The ultrasonographic differentiation of
obstructive versus nonobstructive hydronephrosis in children: a multivariate scoring system. J Urol 1997; 158:560–565.
92.Sudah M, Vanninen R, Partanen K, Heino A, Vainio P, Ala-Opas M. Magnetic resonance urography in evaluation of acute flank pain: T2–weighted sequences and
gadolinium-enhanced three-dimensional FLASH compared with urography AJR 2001;176:105–112.
93.Foda MM, Gatfield CT, Matzinger M, et al. A prospective randomized trial comparing 2 diuresis renography techniques for evaluation of suspected upper urinary tract obstruction in children. J Urol 1998;159:1691– 1693.
94.Harrington TG, Kandel LB. Renal colic following a gunshot wound to the abdomen: the birdshot calculus. J Urol 1997;157:1351–1352.
95.Sheafor DH, Hertzberg BS, Freed KS, et al. Nonenhanced helical CT and US in the emergency evaluation of patients with renal colic: prospective com-parison. Radiology 2000;217:792–797.
96.Assi Z, Platt JF, Francis IR, Cohan RH, Korobkin M. Sensitivity of CT scout radiography and abdominal radiography for revealing ureteral calculi on helical CT: implications for radiologic follow-up. AJR 2000;175:333–337.
97.Zagoria RJ, Khatod EG, Chen MY. Abdominal radiography after CT reveals urinary calculi: a method to predict usefulness of abdominal radiography on the basis of size and CT attenuation of calculi. AJR 2001;176:1117–1122.
98.Chong WK, Wysoki M, Heller LG, Zegel HG. Renal carcinoma presenting with flank pain: a potential drawback of unenhanced CT. AJR 2000;174:667–669.
99.Goldman SM, Faintuch S, Ajzen SA, et al. Diagnostic value of attenuation measurements of the kidney on unenhanced helical CT of obstructive ureterolithiasis. AJR 2004;182:1251–1254.
100.Jones RA, Perez-Brayfield MR, Kirsch AJ, GrattanSmith JD. Renal transit time with MR urography in children. Radiology 2004;233:41–50.
101.Takahashi N, Kawashima A, Ernst RD, et al. Ureterolithiasis: can clinical outcome be predicted with unenhanced helical CT? Radiology 1998;208: 97–102.
102.Frauscher F, Janetschek G, Helweg G, Strasser H, Bartsch G, zur Nedden D. Crossing vessels at the ureteropelvic junction: detection with contrastenhanced color Doppler imaging. Radiology 1999;210: 727–731.
103.Nishie A,Yoshimitsu K, Irie H, et al. Radiologic features of Castleman’s disease occupying the renal sinus. AJR 2003;181:1037–1040.
104.Geavlete P, Georgescu D, Nita G, Cauni V. [Doppler ultrasonography in the function assessment of double J ureteral endoprosthesis in patients with extrinsic ureteral obstruction.] [French] Prog Urol 2001;11: 22–28.
105.Sugamoto T, Yokoyama M, Nishio S, Takeuchi M. Cholesteatoma of the ureter: a case report. [Review] Int J Urol 1997;4:621–622.
106.Weinberg B,Yeung N. Sonographic sign of intermittent dilatation of the renal collecting system in 10 patients with vesicoureteral reflux. J Clin Ultrasound 1998;26: 65–68.
107.Darge K, Troeger J. Vesicoureteral reflux grading in contrast-enhanced voiding urosonography. Eur J Radiol 2002;43:122–128.
108.Bertschy C, Aubert D, Piolat C, Billerey C. [Ureterovesical implantation after failure of endoscopic treatment of reflux: anatomical and histological study of 61

682
ADVANCED IMAGING OF THE ABDOMEN
resection specimens from 40 children.] [French] Prog Urol 2001;11:113–117.
109.Olbing H, Hirche H, Koskimies O, et al. Renal growth in children with severe vesicoureteral reflux: 10-year prospective study of medical and surgical treatment: the International Reflux Study in Children (European branch).] Radiology 2000;216:731–737.
110.Chow WH, Lindblad P, Gridley G, et al. Risk of urinary tract cancers following kidney or ureter stones. J Nat Cancer Inst 1997;89:1453–1457.
111.Daudon M. [Drug-induced urinary calculi in 1999.] [Review] [French] Prog Urol 1999;9:1023–1033.
112.Saw KC, McAteer JA, Monga AG, Chua GT, Lingeman JE, Williams JC Jr. Helical CT of urinary calculi: effect of stone composition, stone size, and scan collimation. AJR 2000;175:329–332.
113.Mostafavi MR, Ernst RD, Saltzman B. Accurate determination of chemical composition of urinary calculi by spiral computerized tomography. J Urol 1998;159: 673–675.
114.Lee JY, Kim SH, Cho JY, Han D. Color and power Doppler twinkling artifacts from urinary stones: clinical observations and phantom studies. AJR 2001;176: 1441–1445.
115.Chelfouh N, Grenier N, Higueret D, et al. Characterization of urinary calculi: in vitro study of “twinkling artifact” revealed by color-flow sonography. AJR 1998;171: 1055–1060.
116.Dore B. [Management of renal calix calculosis.] [Review] [French] Presse Med 1999;28:2181–2188.
117.Soh J. [The maximum volume of urinary calculi to be disintegrated by ESWL.] [Japanese] Nippon Hinyokika Gakkai Zasshi 1998;89:23–28.
118.Traxer O, Lottmann H, Archambaud F, Helal B, Mercier Pageyral B. [Long-term evaluation with DMSA-Tc 99m scintigraphy of renal parenchymal involvement in children after shockwave extracorporeal lithotripsy.] [French] Prog Urol 1998;8:502–506.
119.Chan KF,Vassar GJ, Pfefer TJ, et al. Holmium:YAG laser lithotripsy: a dominant photothermal ablative mechanism with chemical decomposition of urinary calculi. Lasers Surg Med 1999;25:22–37.
120.Havel D, Saussine C, Fath C, Lang H, Faure F, Jacqmin D. Single stones of the lower pole of the kidney. Comparative results of extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy. Eur Urol 1998;33:396–400.
121.Gremmo E, Ballanger P, Dore B, Aubert J. [Hemorrhagic complications during percutaneous nephrolithotomy. Retrospective studies of 772 cases.] [French] Prog Urol 1999;9:460–463.
122.Schillinger F, Delclaux B, Milcent T, et al. [Renal sarcoidosis with a pseudotumoral pyelic localization.] [French] Presse Med 1999;28:683–685.
123.Yassa NA, Peng M, Ralls PW. Perirenal lucency (“kidney sweat”): a new sign of renal failure. AJR 1999;173:1075–1077.
124.Delzell E, Shapiro S. A review of epidemiologic studies of nonnarcotic analgesics and chronic renal disease. [Review] Medicine 1998;77:102–121.
125.Michail S, Stathakis C, Nakopoulou L, et al. Acute renal failure in an adult patient with Henoch-Schoenlein purpura after episode of macroscopic hematuria. Ren Fail 1999;21:107–111.
126.Selcuk NY, Odabas AR, Cetinkaya R, Tonbul HZ, San A. Outcome of pregnancies with HELLP syndrome complicated by acute renal failure (1989–1999). Ren Fail 2000;22:319–327.
127.Angelelli G, Stabile Ianora AA, Scardapane A, Rotondo A. [Computerized tomography in the study of the diabetic kidney.] [Italian] Radiol Med 2000;99:72– 80.
128.Johnston RJ, Alkhunaizi AM. Unilateral focal segmental glomerulosclerosis with contralateral sparing on the side of renal artery stenosis. AJR 1999;172:35– 37.
129.Colli A, Fraquelli M, Pometta R, Cocciolo M, Visentin S, Conte D. Renovascular impedance and esophageal varices in patients with Child-Pugh class A cirrhosis. Radiology 2001;219:712–715.
130.Katagiri K, Okada S, Kumazaki T, Tsuboi N. [Clearance of gadolinium contrast agent by hemodialysis: in vitro and clinical studies.] [Japanese] Nippon Igaku Hoshasen Gakkai Zasshi 1998;58:739–744.
131.Takebayashi S, Hidai H, Chiba T, Takagi H, Koike S, Matsubara S. Using helical CT to evaluate renal cell carcinoma in patients undergoing hemodialysis: value of early enhanced images. AJR 1999;172:429– 433.
132.Vidart A, Pfister C, Bugel H, Savoye-Collet C, Thoumas D, Grise P. [Role of helical tomodensitometry in the early diagnosis of renal infarction.] [French] Prog Urol 2001; 11:217–221.
133.Di Fiori JL, Rodrigue D, Kaptein EM, Ralls PW. Diagnostic sonography of HIV-associated nephropathy: new observations and clinical correlation. AJR 1998;171:713–716.
134.Rankin SC, Jan W, Koffman CG. Noninvasive imaging of living related kidney donors: evaluation with CT angiography and gadolinium-enhanced MR angiography. AJR 2001;177:349–355.
135.Fink C, Hallscheidt PJ, Hosch WP, et al. Preoperative evaluation of living renal donors: value of contrastenhanced 3D magnetic resonance angiography and comparison of three rendering algorithms. Eur Radiol 2003;13:794–801.
136.Jha RC, Korangy SJ, Ascher SM, Takahama J, Kuo PC, Johnson LB. MR angiography and preoperative evaluation for laparoscopic donor nephrectomy. AJR 2002; 178:1489–1495.
137.Moresco KP,Patel NH,Namyslowski Y,Shah H,Johnson MS, Trerotola SO. Carbon dioxide angiography of the transplanted kidney: technical considerations and imaging findings. AJR 1998;171:1271–1276.
138.Hilborn MD, Bude RO, Murphy KJ, Platt JF, Rubin JM. Renal transplant evaluation with power Doppler sonography. Br J Radiol 1997;70:39–42.
139.Amodio F, Rossi E, Carbone M, et al. [Echographic study with high-frequency and high-spatial resolution transducer in the evaluation of renal transplant in pediatric age.] [Italian] Radiol Med 2000;99:68–71.
140.Heindel W, Kugel H, Wenzel F, Stippel D, Schmidt R, Lackner K. Localized 31P MR spectroscopy of the transplanted human kidney in situ shows altered metabolism in rejection and acute tubular necrosis. J Magn Reson Imaging 1997;7:858–864.
141.Capocasale E, Bignardi L, Adorni A, D’Errico G, Viola V, Botta GC. [Neoplasms and kidney transplantation.
|
|
|
683 |
|
|
|
|
KIDNEYS AND URETERS |
|
|
|
|
Case contribution.] [Italian] Minerva Urol Nefrol |
|
adult patients prior to antireflux ureteral implantation. |
|
1998;50:127–131. |
|
Radiology 2004;233:35–39. |
142. |
Lopez-Ben R, Smith JK, Kew CE 2nd, Kenney PJ, Julian |
145. |
Lezaic V, Radivojevic R, Radosavljevic G, et al. Does |
|
BA, Robbin ML. Focal posttransplantation lymphopro- |
|
tuberculosis after kidney transplantation follow the |
|
liferative disorder at the renal allograft hilum. AJR |
|
trend of tuberculosis in general population? Ren Fail |
|
2000;175:1417–1422. |
|
2001;23:97–106. |
143. |
Swindle P, Falk M, Rigby R, Petrie J, Hawley C, Nicol D. |
146. |
Morcos SK, Thomsen HS, Webb JA, et al. Dialysis and |
|
Transitional cell carcinoma in renal transplant recipi- |
|
contrast media. Eur Radiol 2002;12:3026–3030. |
|
ents: the influence of compound analgesics. Br J Urol |
147. |
Tombach B, Bremer C, Reimer P, et al. Renal tolerance |
|
1998;81:229–233. |
|
of a neutral gadolinium chelate (gadobutrol) in |
144. |
Valentini AL, De Gaetano AM, Minordi LM, et al. |
|
patients with chronic renal failure: results of a ran- |
|
Contrast-enhanced voiding US for grading of reflux in |
|
domized study. Radiology 2001;218:651–657. |
11
Bladder
Technique
Conventional Cystography
Cystography is a well-established technique in evaluating the bladder lumen and providing access for biopsies. It is often used as a gold standard when evaluating other imaging procedures. Cystography as used here implies conventional cystography, which consists of lumen distention with a contrast agent introduced via a catheter and appropriate filming. Cystography is also feasible using computed tomography (CT), ultrasonography (US), magnetic resonance (MR), and radionuclide techniques.
Voiding cystourethrography continues to be the gold standard for imaging evaluation children with urinary tract infection, male urethra, functional bladder conditions and in detecting vesicoureteral reflux. Although radionuclide and contrast enhanced US cystography have a role in screening and follow-up of established conditions, most initial evaluation of function and anatomy appears best served by voiding cystourethrography.
Computed Tomography
A typical CT cystography technique consists of contiguous 5-mm axial scans after bladder distention with a 4% iodinated solution as a positive contrast agent. Air or carbon dioxide is
occasionally used for bladder distention, but a potential complication of air is air embolism. Imaging in both the supine and prone positions is necessary when using gas to detect tumors otherwise covered with fluid.
Similar to CT colonoscopy, CT cystoscopy (also called virtual cystoscopy) is feasible with a contrast filled bladder. Computed tomography cystoscopy is an alternate procedure in patients with urethral strictures who cannot undergo conventional cystoscopy or cystography but indications are expanding and some enthusiasts believe it will replace a large part of conventional cystoscopy. Three-dimensional (3D) CT cystography using perspective volume rendering and a shaded-surface 3D outline evaluates tumor size and shape and provides information about its relationship to adjoining mucosa.With current techniques, however, endoscopic cystoscopy has better spatial resolution in detecting small bladder tumors; thus CT cystoscopy detected 90% of bladder tumors, with all undetected tumors being <5mm in diameter (1); transverse and virtual images are complemen- tary—some small tumors are identified only on virtual images but bladder wall thickening is more apparent on transverse images.
Flow of opacified urine into the bladder during contrast-enhanced CT results in intraluminal artifacts due to incomplete mixing. If necessary, delayed bladder images should be obtained to eliminate these artifacts.
685

686
Ultrasonography
Bladder US is performed using a transabdominal, endorectal, endovaginal, or endourethral approach. Color Doppler US detects ureteral jets and with unilateral ureteral obstruction, Doppler US reveals asymmetry to these ureteral jets. The presence of normal ureteral jets excludes significant obstruction.
Intravesical instillation of an US contrast agent aids detection of certain abnormalities, such as vesicoureteral reflux. A galactose-based microbubble contrast agent, Levovist, is typically employed. Contrast duration for this agent varies when mixed with normal saline. A high concentration of dissolved oxygen in normal saline appears to prevent diffusion of gas from the microbubbles into the solution and as a result contrast duration is longer than with use of a low oxygen concentration solution, such as is found in vacuum sealed containers (2).
Magnetic Resonance Imaging
On T1-weighted images urine is homogeneously hypointense and blends into the bladder wall. On T2-weighted images urine is hyperintense while bladder wall muscle layers remain hypointense and the two can be differentiated from each other. Immediate postcontrast images reveal little or no urine enhancement, but with renal excretion urine becomes hyperintense on delayed images.
Bladder instillation of a superparamagnetic iron oxide contrast agent aids in evaluating intraluminal extension of bladder tumors. High-resolution T2-weighted turbo spin echo (TSE) sequences detect tumors as small as 4mm and estimate the depth of infiltration by identifying inner and outer bladder wall margins (3); this technique, however, does not readily identify different bladder wall layers.
Magnetic resonance (MR) cystoscopy is based on principles similar to CT cystoscopy. After filling the bladder with a negative contrast agent and using a heavily T2-weighted sequence such as half-Fourier acquisition single-shot turbo spin echo (HASTE), axial and virtual cystoscopic images achieved a sensitivity of about 90% in detecting tumors <1cm and 100% for tumors 1cm or larger (4), results not differing statistically from CT cystoscopy or conventional cystoscopy.
ADVANCED IMAGING OF THE ABDOMEN
Virtual MR cystoscopy without bladder filling with contrast or use of IV contrast is also feasible; tumors >1cm are readily detected (5). The role of such a contrast-less MR study in screening and diagnosis remains to be established.
Scintigraphy
Radionuclide cystography is less often performed than conventional cystography because of its poorer spatial resolution. Technetium99m (Tc-99m)–sulfur colloid is not absorbed from the bladder and is thus employed. Indirect radionuclide cystography using Tc-99m- mercaptoacetylglycilglycilglycine (MAG3) may be sufficient for some indications.
Congenital Abnormalities
Agenesis
Bladder agenesis is very rare and is usually associated with other major anomalies. Most affected neonates are stillborn.
Duplication
Bladder duplication is rare. With complete duplication each kidney and ureter drains into its separate bladder, which then drains by separate urethras. Some duplications are incomplete and the two bladders communicate through an isthmus. Some bladders only appear duplicated because of an internal septum. An “hourglass” bladder or a large diverticulum arising from the dome of the bladder also mimics an incomplete duplication.
Cystography readily detects a bladder duplication.
A rare bladder duplication is associated with exstrophy, epispadias, and other abnormalities.
Cloacal Exstrophy
Various gradations in failure of fusion of the inferior abdominal wall range from an omphalocele, to cloacal (bladder) exstrophy, to epispadias. This condition is more common in males. In some, the anterior abdominal muscles and anterior bladder wall are absent.
Cloacal exstrophy is associated with an omphalocele, imperforate anus, exstrophy of
687
BLADDER
two hemibladders, and an everted cecum between which lie the hemibladders. Epispadias is part of an exstrophy abnormality. Cryptorchidism and an umbilical hernia are common. Extensive bowel anomalies include a blind-ending hindgut and an omphalocele. The terminal ileum may prolapse out of the cecum. Spinal anomalies are common and the spinal cord is tethered. An association exists between bladder exstrophy and subsequent development of a bladder malignancy.
Conventional radiographs reveal symphysis pubis widening. Such widening is not pathognomonic for cloacal exstrophy but is also found in cloacal malformation, epispadias, and other hindgut malformations. In exstrophy the iliac bones are rotated laterally.
Surgical treatment of these patients is complex and includes closure of an omphalocele, separation of the gastrointestinal tract from hemibladders, and creation of a single bladder. A bladder continence mechanism needs to be created. Lastly, if possible, a colon pull-through is performed.
Previous therapy for cloacal exstrophy was cystectomy and ureterosigmoidostomy. A number of complications develop with this procedure, including urinary infections and renal damage, with the major long-term complication being development of rectosigmoid adenocarcinoma. The risk of carcinoma is much less after creation of a urinary colonic conduit than with a simple ureteral sigmoidostomy.
Serial renal US is worthwhile in these patients to assess renal status and check for development of hydronephrosis. Renal ectopia is common. These patients are prone to reflux.
A cloacal malformation is a different entity, occurs only in girls, and is not related to cloacal exstrophy; it is discussed in Chapter 12.
Ureterocele
Clinical
A ureterocele is a congenital anomaly consisting of a dilated intramural ureteral segment. It is associated with urinary retention and infection. Ureteroceles are mostly a pediatric diagnosis but they occasionally first manifest in adulthood. They are classified into simple and ectopic, depending on the distal orifice. About 10% are bilateral. Some authors suggest that sib-
lings of children with ureteroceles be screened for urogenital abnormalities.
Ectopic ureteroceles are often part of a duplicated renal collecting systems, with most terminating a ureter draining the upper renal pole. They are more common in girls and are a common cause of bladder obstruction in girls. An extreme example consists of bilateral ureteroceles and bilateral duplex systems. An ectopic ureterocele does occur in patients with a single kidney or a horseshoe kidney.
An ectopic ureterocele can distort an adjacent normally located ureterovesical junction to the point of inducing reflux. A rare ureterocele prolapses and even strangulates. Or occasionally a simple ureterocele even prolapses into the urethra and leads to bladder outlet obstruction. Bladder outlet obstruction can also be due to a simple ureterocele if it is large enough.
If necessary, a ureterocele is treated by endoscopic ureterocele incision; the success rate is lower with ectopic ureteroceles. Vesicoureteral reflux develops after such endoscopic incision in about half the patients, with reflux being more common with an ectopic ureterocele.
Imaging
Intravenous urography of a simple ureterocele is usually diagnostic. A ureterocele is seen as a cyst-like dilation of the distal ureter protruding into the bladder lumen; the ureterocele wall appears as a thin radiolucent line, although infection or stasis results in thickening. The typical “cobra-head” appearance is familiar to most radiologists. At times urography simply reveals a large radiolucent tumor in the bladder in association with nonvisualization of the ipsilateral kidney upper pole.
A cystogram detects a ureterocele, provided instilled contrast does not efface or obscure it. Serial visualization during bladder filling and voiding is helpful.
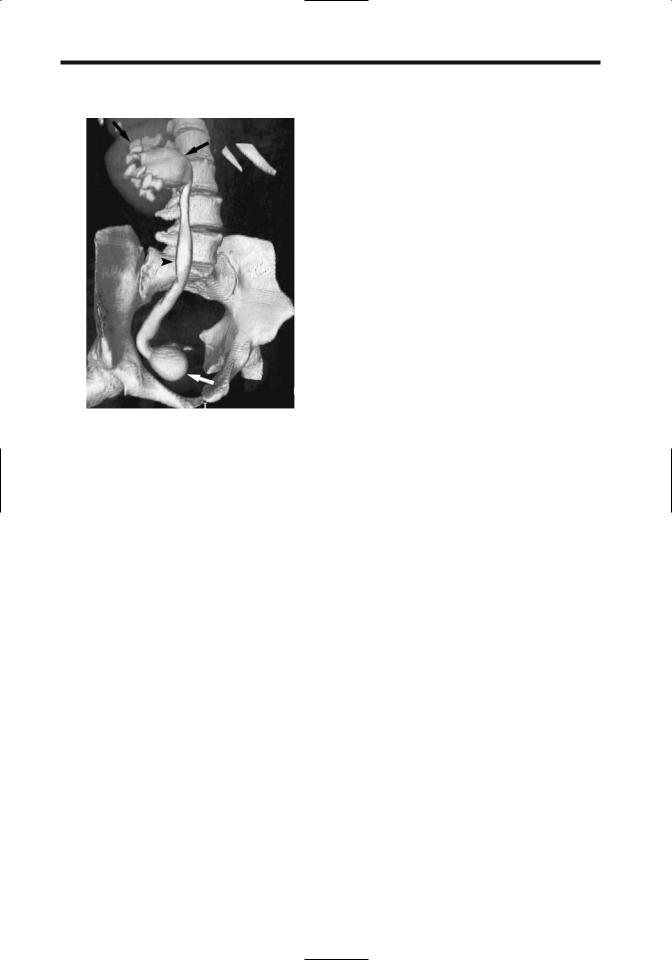
Computed tomography of a ureterocele reveals a well-marginated soft tissue tumor at the ureteral insertion (Fig. 11.1). A simple ureterocele is seen on US as a thin-walled, fluid-filled structure at the trigone.
Occasionally a diminutive renal upper pole is drained by a small duplicated ureter that terminates in a relatively large ureterocele. This condition, called ureterocele disproportion, is
688
Figure 11.1. Ureterocele. Excretory phase three-dimensional (3D) computed tomography (CT) reconstruction identifies hydronephrosis, hydroureter, and a ureterocele (arrow). (Source: Joffe SA, Servaes S, Okon S, Horowitz M. Multi-detector row CT urography in the evaluation of hematuria. RadioGraphics 2003;23(6):1441–1456, with permission from the Radiological Society of North America.)
ADVANCED IMAGING OF THE ABDOMEN
midline extending from the anterior superior bladder wall to the umbilicus. This embryonic communication normally closes before birth, but patency after birth results in luminal communication between the bladder and the umbilicus. Partial obliteration leads to a blind ending sinus at the umbilical end, or, with failure of the bladder end to close, a sinus communicates with the bladder (vesicourachal diverticulum). A urachal cyst (omphalovesical cyst) represents a cavity in the urachus with both the bladder and umbilical ends closed. In children with urachal abnormalities, urachal sinuses and cysts predominate, with a patent urachus and a urachal diverticulum being less common.
Ultrasonography identifies a midline mass between the rectus abdominis muscle and the superior-anterior bladder wall, representing a urachal remnant, in about one third of young adults. A majority of these urachal remnants are nodular, with a minority being tubular in shape. Their prevalence decreases with age, presumably due to involution. In most people a urachal remnant is a normal variant. Occasionally one manifests by hematuria and is resected.
difficult to diagnose with most imaging modalities.
Some ureteral duplications and ectopic ureteroceles are associated with ureteral obstruction, marked hydronephrosis, and dilation of the involved ureter to the point that adjacent nonobstructed collecting systems are displaced inferiorly. The reverse can also occur—occa- sionally an obstructed normal ureter mimics the appearance of a ureterocele.
Stones develop in some ureteroceles.
The term ureterocele eversion describes a ureterocele that everts or intussuscepts retrograde into the ureter during voiding cystourethrography. Radiographically, the outpouching can appear similar to a paraureteral bladder diverticulum. At times fluoroscopy aids in detecting these eversions.
Urachal Abnormalities
The urachus, or median umbilical ligament, is a residual fibromuscular cord located in the
Fistula and Sinus Tract
Urachal anomalies are more common in males. The prevalence of vesicourachal fistulas is increased in the prune belly syndrome. A patent urachus is also associated with urethral obstruction, such as posterior urethral valves or urethral atresia.
The presence of a patent urachus is generally suspected in the neonate and is best established by direct contrast injection into the umbilical opening. A voiding cystourethrogram also detects patency, provided the images are obtained with the infant in a lateral projection. At times an almost patent urachus is initially asymptomatic but manifests later in life when a bladder outlet obstruction develops.
A vesicourachal diverticulum is a midline outpouching extending from the superioranterior bladder wall. Most are discovered incidentally. Occasionally stasis results in recurrent urinary tract infection and stone formation. Cancer originating in a vesicourachal diverticulum is an uncommon occurrence developing in adults.
689
BLADDER
A vesicourachal diverticulum can be suggested by CT, US, or MRI by detecting a bladder outpouching in the appropriate location.
Infection
Infection leads to a pyourachus, located in the midline, deep to the rectus abdominis muscle.
Imaging reveals a fluid-filled midline cavity close to the anterior bladder wall. When infected, the cyst in effect becomes an abscess and the cyst wall gradually thickens. A characteristic CT finding of a pyourachus is a conicalshaped structure extending from the umbilicus to the bladder dome. Inflammatory changes in adjacent subcutaneous tissues, the rectus abdominis muscle, and mesenteric fat surround the infected urachus. Chronic infection results in a thickened cyst wall.
An infected urachal cyst can be drained percutaneously, although this is generally a temporary measure because of an increased reinfection rate. For these reasons most urachal cysts are resected. Also, if an infected urachal cyst is suspected in an adult, a necrotic (or infected) carcinoma should be in the differential diagnosis.
Cyst/Neoplasm
Some urachal cysts remain asymptomatic, and others serve as a nidus for infection, while a neoplasm develops in an occasional one. Some urachal cysts gradually enlarge. In general, if US or other imaging shows a midline cystic structure between the umbilicus and bladder not related to bowel, an urachal cyst should be suspected.
Occasionally dystrophic calcifications or osseous metaplasia develop in an urachal cyst wall. Metaplasia of urachal transitional epithelium can evolve into an adenoma and carcinoma. A majority of these carcinomas are adenocarcinomas, with an occasional transitional cell carcinoma, squamous cell carcinoma, sarcoma, or even a small cell carcinoma. In general, most carcinomas are detected late when the tumor has already spread. A not uncommon presentation is a suprapubic tumor, hematuria, mucusuria, pain, or discharge from the umbilicus. An occasional urachal adenocarcinoma metastasizes (6); a urachal mucinous carcinoma
is a less common cause of pseudomyxoma peritonei.
Imaging reveals a tumor involving the bladder apex, mostly extravesical in location and often growing along the urachus. Primary bladder carcinomas tend not to have these findings. Some mucin-producing urachal adenocarcinomas develop psammomatous calcifications, findings readily detected by CT. These mucinous adenocarcinomas can be solid, cystic, or mixed.
Ultrasonography should readily detect urachal cysts. If needed, CT confirms the diagnosis. Doppler US of an urachus adenocarcinoma revealed neovascularity and a low resistive index in the tumor (7).
Trauma
Spontaneous bladder rupture in the absence of trauma is rare but has occurred in a setting of previous radiation therapy, surgery, infection, or is idiopathic. Contrast extravasation may occur during voiding cystourethrography performed in a patient with an unused bladder. Most of these extravasations are self-limiting.
The risk of bladder rupture increases with bladder distention. Perforation of an empty bladder is generally associated with a penetrating injury, either extrinsic or a bone fragment.
After blunt pelvic trauma or in a setting of pelvic fractures, bladder or urethral injury is suggested by hematuria or inability to urinate. A small minority of patients with bladder rupture have only microscopic hematuria. A direct association exists between gross hematuria and bladder perforation, most being extraperitoneal, less often intraperitoneal, and least common being both intraand extraperitoneal. Pelvic fractures are present in a majority of patients with bladder perforation.
A retrograde urethrogram is generally obtained to exclude urethral injury, followed by a cystogram. At times extraperitoneal contrast extravasation is only seen on postdrainage radiographs. A cystogram should detect not only bladder rupture but also determine whether the rupture is intraor extraperitoneal (Fig. 11.2). During the cystogram an attempt should be made to identify a site of perforation. Subtle intraperitoneal leaks are difficult to
