
- •Pineal Parenchymal Tumors
- •Germ Cell Tumors
- •Selected References
- •Medulloblastoma
- •Selected References
- •Anatomy of the Cranial Meninges
- •Meningomas
- •Primary Melanocytic Lesions
- •Other Related Neoplasms
- •Selected References
- •Cranial Nerve Anatomy
- •Schwannomas
- •Neurofibromas
- •Selected References
- •Histiocytic Tumors
- •Selected References
- •Sellar Region Anatomy
- •Normal Imaging Variants
- •Congenital Lesions
- •Neoplasms
- •Miscellaneous Lesions
- •Selected References
- •Intracranial Pseudotumors
- •Selected References
- •Metastatic Lesions
- •Paraneoplastic Syndromes
- •Selected References
- •Scalp Cysts
- •Extraaxial Cysts
- •Parenchymal Cysts
- •Intraventricular Cysts
- •Selected References
- •Anatomy and Physiology of the Basal Ganglia and Thalami
- •Selected References
- •Alcohol and Related Disorders
- •Opioids and Derivatives
- •Inhaled Gases and Toxins
- •Selected References
- •Selected References
- •Hypertensive Encephalopathies
- •Glucose Disorders
- •Thyroid Disorders
- •Seizures and Related Disorders
- •Miscellaneous Disorders
- •Selected References
- •The Normal Aging Brain
- •Dementias
- •Degenerative Disorders
- •Selected References
- •Normal Variants
- •Hydrocephalus
- •CSF Leaks and Sequelae
- •Selected References
- •Cerebral Hemisphere Formation
- •Imaging Approach to Brain Malformations
- •Posterior Fossa Anatomy
- •Chiari Malformations
- •Hindbrain Malformations
- •Selected References
- •Commissural Anomalies
- •Malformations Secondary to Abnormal Postmigrational Development
- •Selected References
- •Anencephaly
- •Holoprosencephaly
- •Holoprosencephaly Variants
- •Related Midline Disorders
- •Holoprosencephaly Mimics
- •Selected References
- •Selected References
- •Selected References
- •Cephaloceles
- •Craniosynostoses
- •Meningeal Anomalies
- •Selected References
- •Index
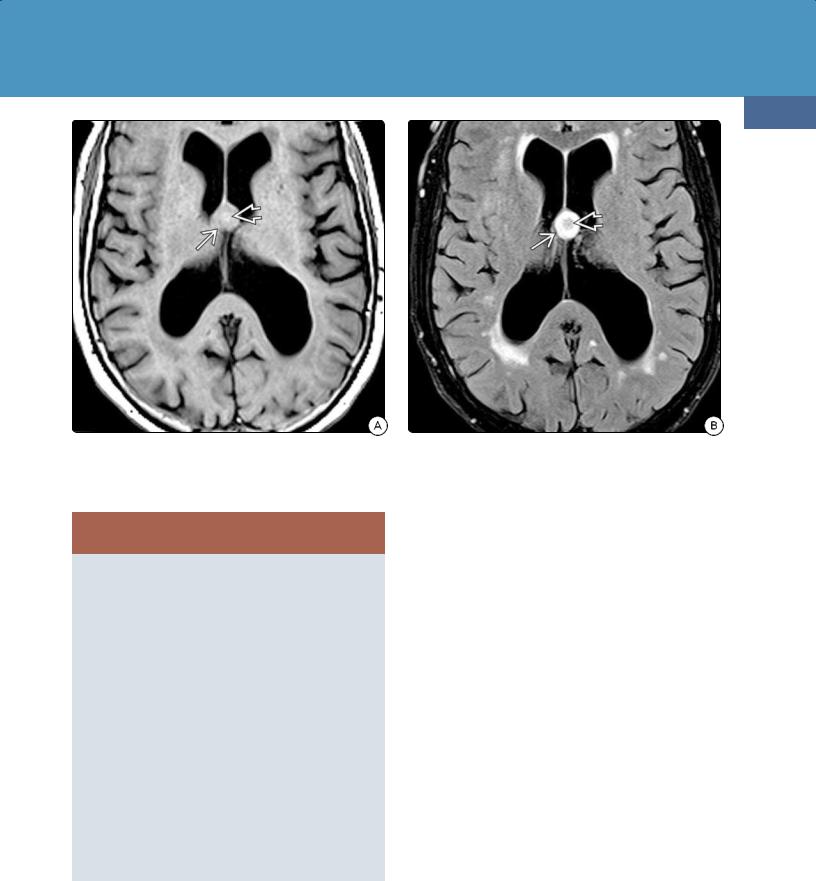
Imaging
CT Findings. Porencephalic cysts are sharply marginated, smooth-walled, CSF-filled cavities that usually communicate directly with an adjacent ventricle (28-46). The ipsilateral ventricle is often enlarged secondary to volume loss in the adjacent parenchyma.
Calcification is rare. Bone CT may show skull thinning and remodeling caused by chronic CSF pulsations.
A porencephalic cyst does not enhance.
MR Findings. Porencephalic cysts follow CSF signal intensity on all sequences (28-46). Large cysts may show internal inhomogeneities secondary to spin dephasing. These cysts suppress completely on FLAIR although there is often a rim of hyperintense gliotic or spongiotic white matter around the cyst. No restriction on DWI is present.
Differential Diagnosis
The major differential diagnosis is cystic encephalomalacia. An encephalomalacic cavity is often more irregular and does not communicate with the adjacent ventricle.
Porencephalic cysts are lined by reactive gliosis (glial "scar"), which occurs when histologically benign astrocytes proliferate in and around damaged brain parenchyma. A porencephalic cyst with surrounding reactive gliosis must be distinguished from spongiosis, a process that represents tissue loss (not astrocytic proliferation) with formation of empty (spongiform) areas ("holes") in the brain. Gliosis is a low to medium cellularity lesion that is hyperintense on T2WI and does not suppress on FLAIR. Spongiosis is T2 hyperintense but suppresses on FLAIR.
An arachnoid cyst is extraaxial and does not communicate with the ventricle. Schizencephaly (literally "split brain") is a congenital lesion that can be either "open" or "closed lip." An "open lip" schizencephalic cleft can look very much like a porencephalic cyst but is lined with dysplastic gray matter, not gliotic white matter.
Hydranencephaly ("water on the brain") is a congenital lesion in which most of the supratentorial developing brain has been destroyed by arterial occlusion. Here the brain looks like a bag of water with little or no remnant cortex. Hydranencephaly is bilateral and symmetric, whereas most porencephalic cysts are unilateral or bilateral but asymmetric.
Intraventricular Cysts
Intraventricular cysts include choroid plexus cysts, colloid cysts, and ependymal cysts.
Choroid Plexus Cysts
Choroid plexus cysts (CPCs) are one of the most common types of intracranial cyst. Most are small and unremarkable. Occasionally, large cysts may appear somewhat atypical and cause diagnostic concern.
Terminology
Nonneoplastic Cysts
893
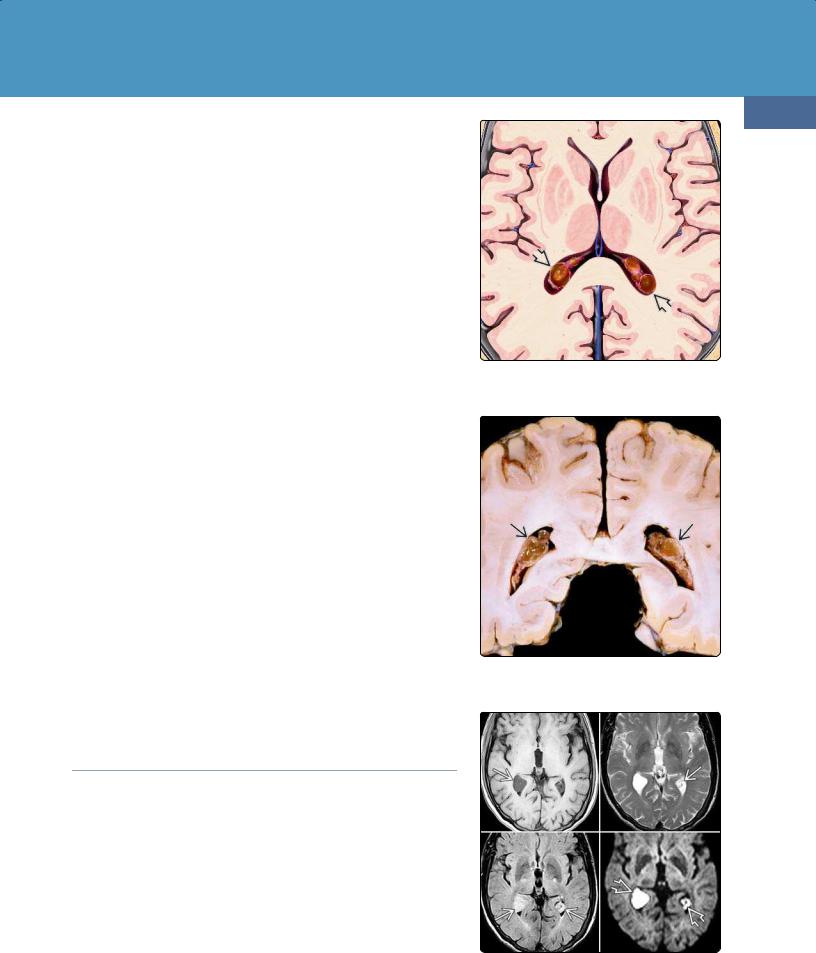
(28-47) Multiple cystic masses are in choroid plexus glomi ; in adults, it increases with age. Most are degenerative xanthogranulomas.
(28-48) Autopsy specimen shows multiple cysts in the choroid plexus glomi of both lateral ventricles. (Courtesy N. Nakase, MD.)
A CPC is also often called a choroid plexus xanthogranuloma. CPCs are nonneoplastic noninflammatory cysts of the choroid plexus.
(28-49) Choroid plexus cysts are usually bilateral and hyperintense compared with CSF and are often very bright on DWI .
Neoplasms, Cysts, and Tumor-Like Lesions
894
(28-50A) Variant choroid plexus cysts are in the body of the lateral ventricle. Cyst contents are slightly hyperintense compared with CSF.
(28-50B) The cysts are so hyperintense on T2WI that the thin cyst walls are barely visible .
Etiology
General Concepts. CPCs can be either congenital or acquired. Acquired lesions are much more common; lipid that accumulates from desquamating, degenerating choroid plexus epithelium coalesces into macrocysts and provokes a xanthomatous response.
Genetics. Large (> 10 mm), congenital CPCs can be associated with aneuploidy, particularly trisomy 18. CPCs, together with choroid plexus papillomas, also occur as part of Aicardi syndrome.
Pathology
Location. Most CPCs are found in the atrium of the lateral ventricle, within the choroid plexus glomus (28-47).
Size and Number. CPCs are mostly small, ranging from a few millimeters up to 1 cm although occasionally larger cysts exceed 2 cm in diameter. Multiple bilateral lesions are significantly more common than solitary unilateral CPCs.
Gross Pathology. CPCs are nodular, partly cystic, yellowish-gray masses that are most often found in the choroid plexus glomus (28-48). They are highly proteinaceous and often gelatinous. Gross hemorrhage is rare.
CHOROID PLEXUS CYSTS: ETIOLOGY, PATHOLOGY, AND CLINICAL ISSUES
Etiology
•Congenital
○Aicardi syndrome
○Trisomy 18
•Acquired
○Desquamated, degenerated epithelium
○Xanthomatous response
Pathology
•Bilateral, usually multiloculated
•Most common in glomi of choroid plexus
•Proteinaceous, gelatinous contents
Clinical Issues
•Most common intracranial cyst
•Most found incidentally
•Most common in fetus/infants, older adults
Clinical Issues
Demographics. CPCs are the most common of all intracranial cysts, occurring in up to 50% of autopsies. CPCs are found at both ends of the age spectrum. In adults, their prevalence increases with age, whereas fetal CPCs decrease with gestational age. There is no sex predilection.
Presentation and Natural History. Most adult CPCs are found incidentally and are asymptomatic, remaining stable for many years. Congenital CPCs are detected on prenatal ultrasound in 1% of fetuses during the second trimester and generally resolve during the third trimester. When detected postnatally, CPCs are of no clinical significance in otherwise normal neonates.
Imaging
(28-50C) T1 C+ FS shows that the thin walls of these multiloculated choroid plexus cysts enhance moderately .
CT Findings. CPCs are isoto slightly hyperdense compared with intraventricular CSF. Irregular clumps of calcification around the margins are
Nonneoplastic Cysts
895
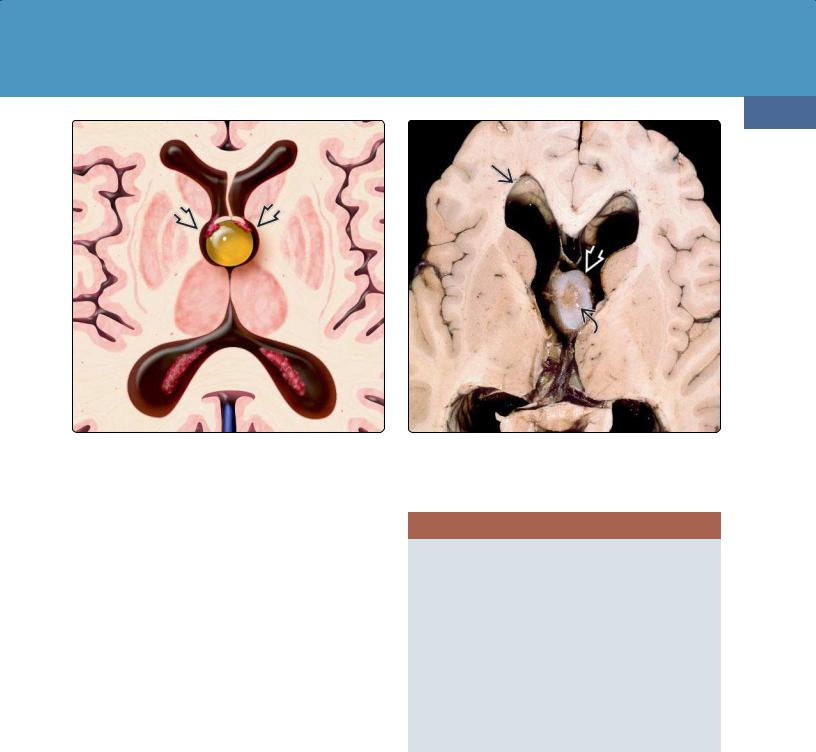
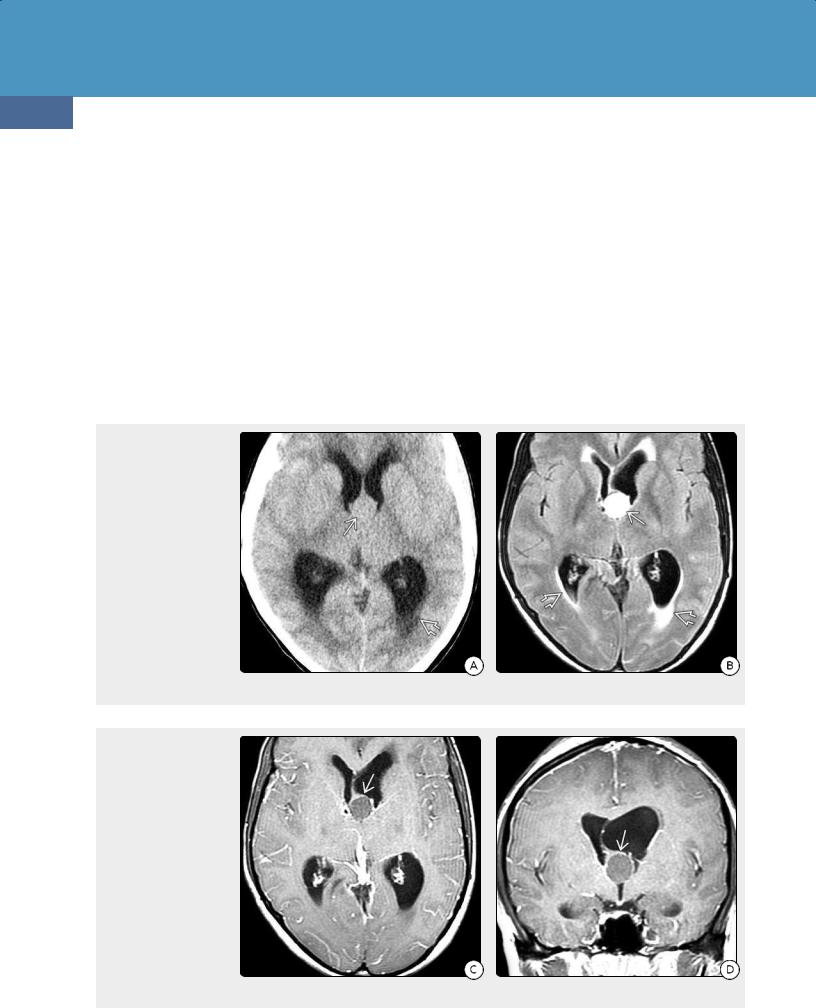
(28-51) Axial graphic shows a classic colloid cyst at the foramen of Monro causing mild/moderate obstructive hydrocephalus. Note that the fornices and choroid plexus are elevated and stretched over the cyst .
common findings. Enhancement varies from none to a complete rim surrounding each cyst.
MR Findings. CPCs do not precisely follow CSF signal intensity. They are isoto slightly hyperintense compared with CSF on T1WI and are hyperintense on PD and T2WI. FLAIR signal is variable (28-49).
Enhancement following contrast administration varies from none to striking. Solid, ring, and nodular patterns occur (2850).
Between 60-80% of CPCs appear quite bright on DWI but often remain isointense with parenchyma on ADC. This may therefore represent pseudorestriction rather than true restricted diffusion.
Ultrasound. Fetal ultrasound may show multiple cysts of variable sizes.
Differential Diagnosis
The major differential diagnosis of a CPC is an ependymal cyst. Ependymal cysts generally displace and compress the choroid plexus rather than arise from it. Ependymal cysts usually behave much more like CSF than CPCs do. Intraventricular parasitic cysts, specifically those of neurocysticercosis, are relatively uncommon. They are not associated with the choroid plexus. A scolex is often present. Intraventricular epidermoid cysts occur but are rare in the lateral ventricles.
(28-52) Autopsy specimen demonstrates obstructive hydrocephalus and a large gelatinous-appearing colloid cystwith a densely fibrotic inspissated center . Lesion is located within the foramen of Monro. (Courtesy R. Hewlett, MD.)
CHOROID PLEXUS CYST: IMAGING AND DDx
CT
•Iso-/mildly hyperdense
•Ca++ common
MR
•Iso-/mildly hyperintense to CSF on T1WI
•Hyperintense on PD/T2WI, FLAIR variable
•Variable enhancement (usually thin rim)
•Bright on DWI but isointense on ADC
Differential Diagnosis
•Most common = ependymal cyst
•Uncommon/rare
○Epidermoid cyst (rarely intraventricular)
○Cystic metastasis
Choroid plexus papilloma of the lateral ventricle is a tumor of children younger than 5 years old and enhances intensely. An enhancing, enlarged choroid plexus without frank cyst formation can also be seen with Sturge-Weber malformation, collateral venous drainage, and diffuse villous hyperplasia. Sturge-Weber and collateral venous drainage usually cause unilateral choroid plexus enlargement. The entire choroid plexus is enlarged in diffuse villous hyperplasia.
Colloid Cyst
Terminology
Colloid cysts (CCs) are also called paraphyseal cysts. They are unilocular, mucin-containing cysts that are almost always
Neoplasms, Cysts, and Tumor-Like Lesions
896
(28-53) NECT scan reveals a classic colloid cyst as a wellcircumscribed hyperdense mass in the foramen of Monro.
found wedged into the top of the third ventricle at the foramen of Monro (28-51).
Etiology
General Concepts. CCs are endodermal—rather than neuroectodermal—cysts. They are similar to the other intracranial foregut-derived cysts, i.e., Rathke cleft and neurenteric cysts. Although their precise etiology is unknown, they are presumed to arise from ectopic endodermal elements that migrate into the embryonic diencephalic roof.
Genetics. No specific gene mutations have been identified. A few rare familial CCs have been described that appear to have an autosomal-recessive pattern of inheritance with variable penetrance.
Pathology
Location. More than 99% of CCs are wedged into the foramen of Monro, attached to the anterosuperior roof of the third ventricle. The posterior aspects of the frontal horns of the lateral ventricle are splayed laterally around the cyst, and the pillars of the fornix "straddle" the CC.
Size and Number. CCs are virtually always solitary lesions. Size varies from tiny (a few millimeters) up to 3 cm. Mean diameter is 1.5 cm.
Gross Pathology. CCs are smooth-walled, well-demarcated, spherical or ovoid cysts that have a gelatinous center of variable viscosity (28-52). Gross hemorrhage is very rare.
Microscopic Features. The wall of a CC consists of a thin fibrous capsule that is lined with simple or pseudostratified columnar epithelium. Some ciliated and mucin-secreting
(28-54) NECT scan shows hyperdense colloid cyst that is hyperintense on T1WI , hypointense on T2WI , with mixed signal intensity on FLAIR .
goblet cells are interspersed throughout the cyst lining. Like other endodermal cysts, CCs are cytokeratin and EMA positive on immunohistochemistry.
Clinical Issues
Epidemiology. CCs account for about 1% of all intracranial tumors but cause 15-20% of all intraventricular tumors.
Demographics. Most symptomatic CCs present between the third and fifth decades. The peak age is 40 years. Pediatric CCs are rare; less than 8% of all patients are younger than 15 years at the time of initial diagnosis. There is no sex predilection.
Presentation. The clinical presentation of CCs is diverse, ranging from asymptomatic, incidentally discovered cysts (nearly half of all patients) to acute deterioration, coma, and death. CCs cause symptoms when they obstruct CSF flow at the foramina of Monro. Headache is the presenting symptom in 50-60% of symptomatic patients.
Natural History. Over 90% of CCs—especially small cysts found in older patients—are stable and do not enlarge. The roughly 10% that do enlarge tend to be larger lesions, often causing hydrocephalus, and found in younger patients. Incidental lesions rarely cause acute obstructive hydrocephalus or sudden neurological deterioration.
Cyst "apoplexy" with intracystic hemorrhage and sudden enlargement occurs but is rare.
Nonneoplastic Cysts
897
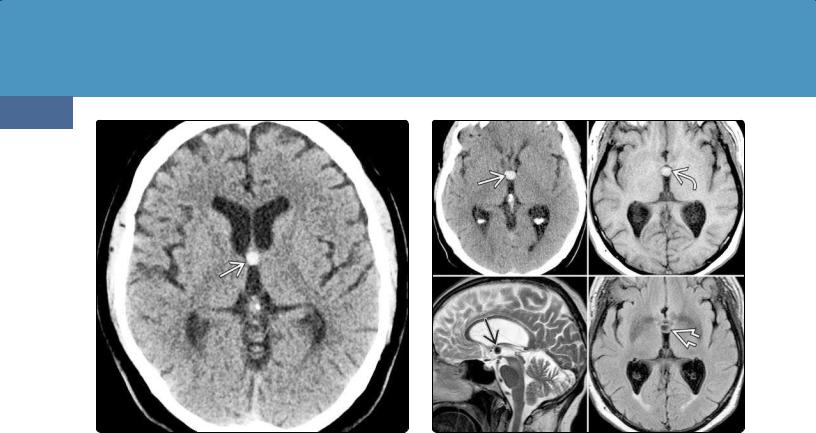
(28-55A) Axial T1WI in a 78y woman with headaches shows moderately enlarged lateral ventricles and isointense mass at the foramen of Monro . Faint hyperintensity in the middle of the mass suggests inspissated mucous in a colloid cyst.
COLLOID CYST: PATHOETIOLOGY AND CLINICAL ISSUES
Etiology
•Endodermal cyst
•Probably derived from ectopic elements in diencephalic roof
Pathology
•Foramen of Monro (> 99%)
•Size varies from a few millimeters up to 3 cm
•Fibrous capsule
•Cyst lining
○Columnar epithelium
○Mucin-secreting goblet cells
•Gelatinous center (variable viscosity)
Clinical Issues
•Epidemiology
○1% of all intracranial tumors
○15-20% of intraventricular masses
•Peak age = 40 years (rare in children)
•Asymptomatic, found incidentally (50%)
•Headache most common symptom
•Sudden obstruction can cause coma, death
•Stable, do not enlarge (90%)
Treatment Options. Small asymptomatic CCs that are discovered incidentally and followed with serial imaging rarely grow or cause obstructive hydrocephalus. However, their treatment is debated. Neuroendoscopic management has emerged as a safe, effective alternative to microsurgery with either a transcortical-transventricular or a transcallosal approach.
(28-55B) FLAIR in the same case shows that most of the cyst is hyperintense . The center of the cyst appears isointense with brain . Colloid cyst with inspissated mucous was removed at surgery.
Imaging
General Features. CCs are well-delineated round or ovoid masses. Imaging appearance depends on their viscosity and/or cholesterol content. The relative amounts of mucous material, cholesterol, protein, and water content all affect density/signal intensity. Desiccated, inspissated cysts appear very different from water-rich lesions.
CT Findings. Density on NECT correlates directly with the hydration state of the cyst contents. Nearly two-thirds of all CCs are hyperdense compared with brain (28-53), whereas one-third are isoto hypodense (28-56A). Hydrocephalus is variable. Intracystic hemorrhage and calcification are very rare.
Most CCs show no enhancement. Occasionally, a thin enhancing rim surrounds the cyst. Solid or nodular enhancement almost never occurs.
CTA/CTV demonstrates that the internal cerebral veins are displaced posterolaterally around the CC.
MR Findings. Signal intensity varies with cyst content.
Signal intensity on T1WI reflects cholesterol concentration. Most CCs are hyperintense compared with brain (28-54), but one-third are isointense. Small isointense CCs may be very difficult to identify on T1WI.
Signal on PD and T2WI is more variable, as it is more reflective of water content. Most CCs are minimally hyperintense to brain on PD and usually isointense on T2WI (28-54). A few CCs with inspissated contents are hypointense. Approximately 25% demonstrate mixed hypoand hyperintensity (the "black hole" effect). Fluid-fluid levels are rare.
Neoplasms, Cysts, and Tumor-Like Lesions
898
CCs do not suppress on FLAIR (28-55), nor do they restrict on DWI.
CCs generally do not enhance. A thin peripheral rim of enhancement can be seen in some cases (28-56).
Differential Diagnosis
A well-delineated focal hyperdense lesion at the foramen of Monro on NECT scan is virtually pathognomonic of a CC. Occasionally, extreme ectasia of an artery—usually the basilar artery—can mimic a CC although serial sections easily demonstrate the tubular nature of the ectatic vessel.
On MR, the most common "lesion" that mimics a CC is artifact caused by pulsatile CSF flow. Phase artifact propagated across the image is helpful in establishing the etiology. Multiplanar imaging and other pulse sequences are also helpful.
(28-56A) Patient had sudden-onset severe headache before he became comatose. Emergency NECT scan shows an isodense mass at the foramen of Monrowith enlarged ventricles. Note the "blurred" ventricular margins . (28-56B) FLAIR shows that the cyst is hyperintense . The "halo" of fluid around the lateral ventricles is secondary to obstructed drainage of interstitial fluid in the deep cerebral WM.
(28-56C) T1 C+ FS demonstrates a rim of enhancement around the cyst . (28-56D) Coronal T1 C+ also shows the enhancing rim . This is a variant colloid cyst.
Neoplasms such as metastasis and subependymoma (usually in the frontal horn or foramen of Monro, not anterosuperior third ventricle) can be hyperdense on NECT scans. Large craniopharyngiomas and pituitary macroadenomas occasionally extend superiorly almost to the foramen of Monro. Multiplanar MR shows that the origin of these tumors is inferior to the third ventricle.
Rarely, an astrocytoma or lymphoma can infiltrate and thicken the fornices and thus mimic a CC. Most all of these neoplasms are diffusely infiltrating, nonfocal lesions that often show moderate to marked enhancement following contrast administration.
Other third ventricle/foramen of Monro choroid plexus masses such as papilloma, xanthogranuloma, and choroid plexus cysts are rare.
COLLOID CYST: IMAGING AND DDx
Imaging
•CT
○2/3 hyperdense
○1/3 isoto hypodense
○Usually do not enhance
•MR
○Signal intensity varies with sequence, cyst contents
○Typical: T1 hyper-, T2 hypointense
○Inspissated: T2 hypointense
○"Black hole" effect (25%)
○Do not suppress on FLAIR
○Generally do not enhance
○Thin peripheral rim enhancement may occur
○No restriction on DWI
Differential Diagnosis
•Most common
○Ectatic basilar artery (NECT)
○CSF flow artifact (MR)
•Less common
○Metastasis
○Subependymoma
○Pituitary macroadenoma
○Craniopharyngioma
•Rare but important
○Low-grade astrocytoma
○Lymphoma
○Choroid plexus papilloma
○Choroid plexus cyst
○Xanthogranuloma
Ependymal Cyst
Terminology
Ependymal cysts are also called glioependymal cysts. Some authors consider ependymal cysts a subtype of neuroepithelial cyst.
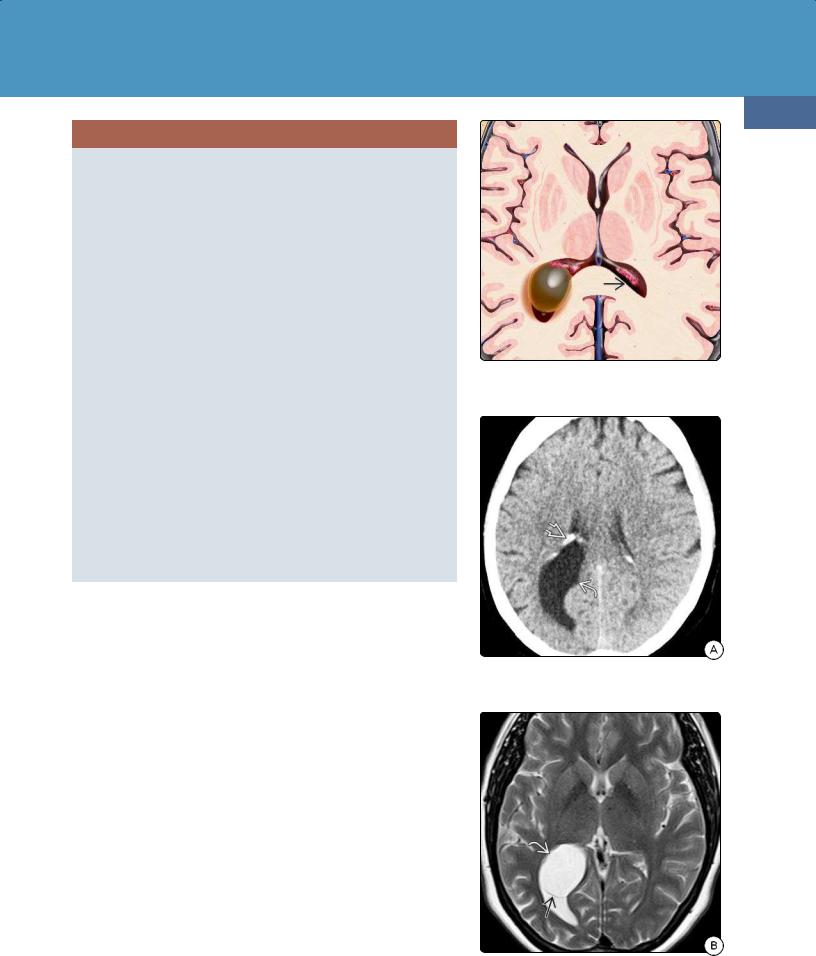
Pathology
Ependymal cysts are solitary lesions that are most often found in the atrium of the lateral ventricles, where they may cause significant ventricular asymmetry (28-57). Less commonly they occur in the brain parenchyma.
Ependymal cysts are rare lesions, accounting for less than 1% of all nonneoplastic intracranial cysts. Their precise pathogenesis is unknown.
Ependymal cysts are usually unilocular, thin walled, and filled with clear CSFlike liquid. They are lined by a layer of simple columnar or cuboidal cells that are similar to the normal endoventricular lining.
Clinical Issues
Ependymal cysts are typically asymptomatic and discovered incidentally at imaging or autopsy. Most patients present as young adults (under 40 years of age). Nonspecific symptoms such as headache and cognitive dysfunction are common. Large ependymal cysts occasionally cause obstructive hydrocephalus and increased intracranial pressure.
Nonneoplastic Cysts
899
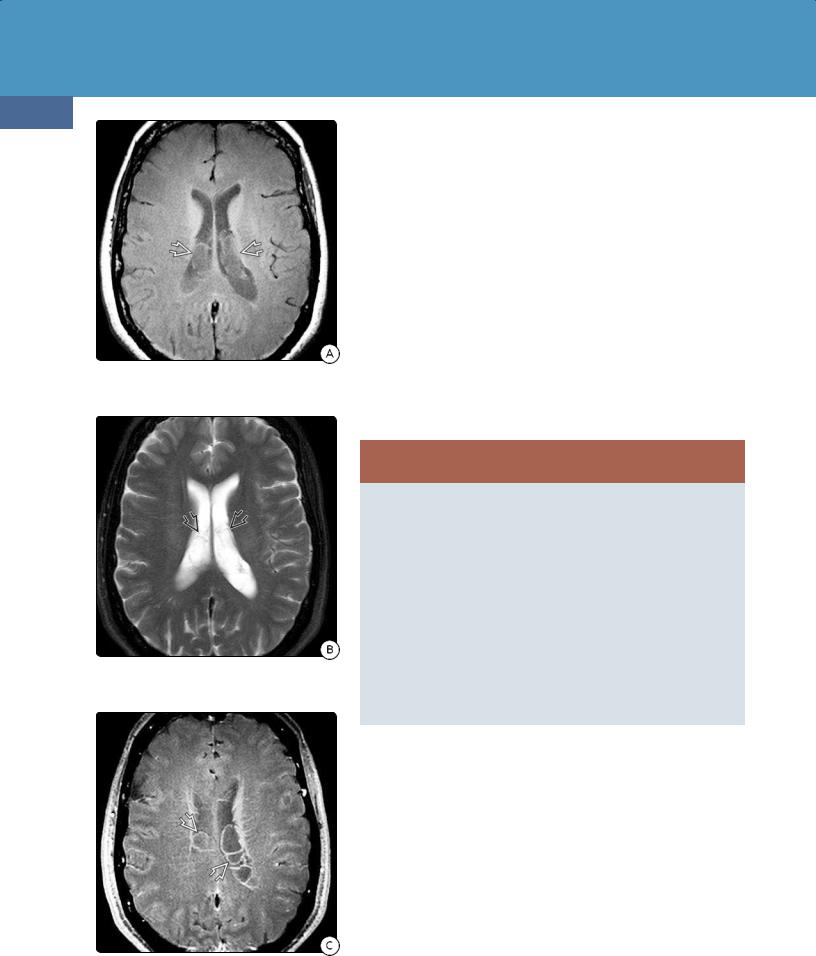
(28-57) Graphic depicts ependymal cyst of the lateral ventricle as a CSF-containing simple cyst that displaces the choroid plexus around it.
(28-58A) Axial NECT of ependymal cyst shows a CSF-containing mass displacing the calcified choroid plexus around it .
(28-58B) T2WI in the same case shows that the unilocular ependymal cyst is exactly like CSF. Note distinct cyst wall .
Neoplasms, Cysts, and Tumor-Like Lesions
900
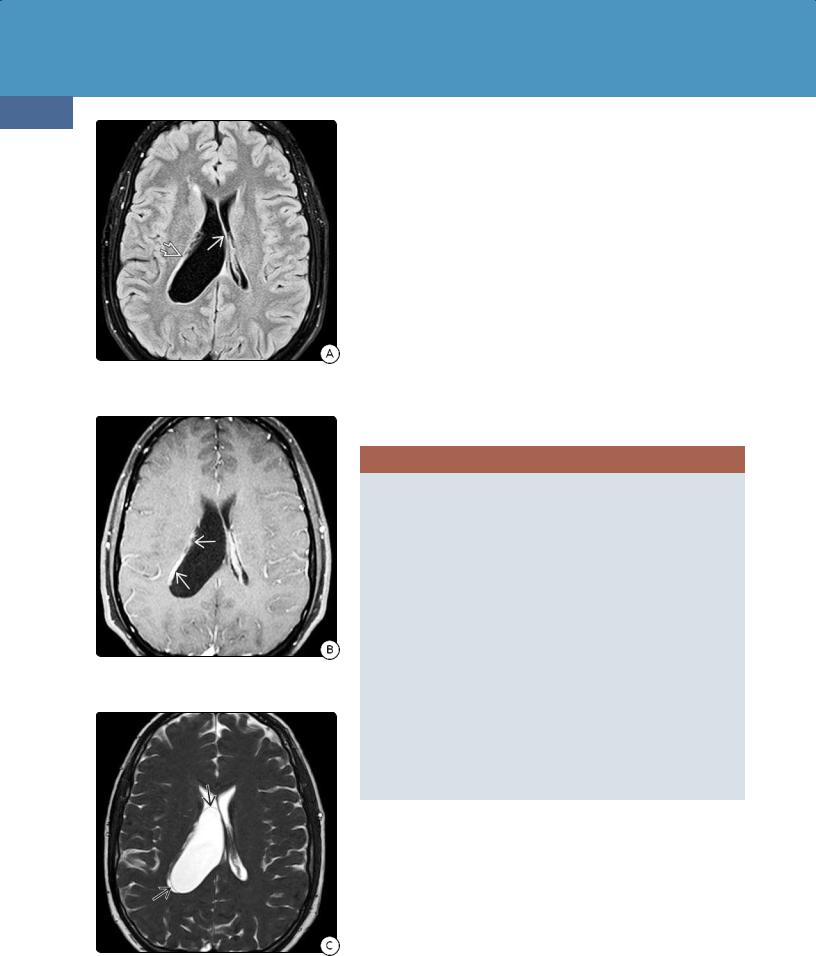
(28-59A) FLAIR, 27y man with severe headaches, shows enlarged body of right lateral ventricle , displaced septum pellucidum, fornices .
(28-59B) T1 C+ FS shows that the choroid plexus is displaced laterally , but no intraventricular mass can be identified.
Imaging
Ependymal cysts parallel CSF in density/signal intensity (28-58). They suppress completely on FLAIR, do not enhance, and do not demonstrate diffusion restriction. Thin-section heavily T2-weighted sequences such as constructive interference in a steady state (CISS) may be necessary to delineate the cyst wall (28-59).
Differential Diagnosis
Except for location, ependymal cysts may be indistinguishable on imaging from other benign intracranial cysts such as neuroglial cysts.
The major intraventricular mass that can mimic ependymal cyst is a choroid plexus cyst. Choroid plexus cysts are typically bilateral, often multilocular, and located within the choroid plexus glomi. Ependymal cysts arise outside the choroid plexus and usually displace it superolaterally.
Epidermoid cysts are rare in the lateral ventricle. They do not suppress completely on FLAIR and demonstrate diffusion restriction on DWI. Arachnoid cysts are identical to ependymal cysts in density and signal intensity but are rarely intraventricular. Cystic metastases to the choroid plexus are rare; nodular or irregular rim enhancement is typical.
EPENDYMAL CYST
Terminology
• Also called glioependymal or neuroepithelial cyst
Pathology
•1% of intracranial cysts
•Solitary, usually unilocular
•Lined by columnar epithelium
•Contain CSF
Clinical Issues
•Most asymptomatic, discovered incidentally
•All ages, but usually < 40 years
Imaging
•Density, signal intensity = CSF
•No enhancement, no restriction
Differential Diagnosis
•Most common
○Choroid plexus cyst
•Uncommon/rare
○Epidermoid cyst
○Arachnoid cyst
○Cystic metastasis
(28-59C) Constructive interference in steady state (CISS) clearly shows wall of an ependymal cyst causing the ventricular dilatation.
