
- •Pineal Parenchymal Tumors
- •Germ Cell Tumors
- •Selected References
- •Medulloblastoma
- •Selected References
- •Anatomy of the Cranial Meninges
- •Meningomas
- •Primary Melanocytic Lesions
- •Other Related Neoplasms
- •Selected References
- •Cranial Nerve Anatomy
- •Schwannomas
- •Neurofibromas
- •Selected References
- •Histiocytic Tumors
- •Selected References
- •Sellar Region Anatomy
- •Normal Imaging Variants
- •Congenital Lesions
- •Neoplasms
- •Miscellaneous Lesions
- •Selected References
- •Intracranial Pseudotumors
- •Selected References
- •Metastatic Lesions
- •Paraneoplastic Syndromes
- •Selected References
- •Scalp Cysts
- •Extraaxial Cysts
- •Parenchymal Cysts
- •Intraventricular Cysts
- •Selected References
- •Anatomy and Physiology of the Basal Ganglia and Thalami
- •Selected References
- •Alcohol and Related Disorders
- •Opioids and Derivatives
- •Inhaled Gases and Toxins
- •Selected References
- •Selected References
- •Hypertensive Encephalopathies
- •Glucose Disorders
- •Thyroid Disorders
- •Seizures and Related Disorders
- •Miscellaneous Disorders
- •Selected References
- •The Normal Aging Brain
- •Dementias
- •Degenerative Disorders
- •Selected References
- •Normal Variants
- •Hydrocephalus
- •CSF Leaks and Sequelae
- •Selected References
- •Cerebral Hemisphere Formation
- •Imaging Approach to Brain Malformations
- •Posterior Fossa Anatomy
- •Chiari Malformations
- •Hindbrain Malformations
- •Selected References
- •Commissural Anomalies
- •Malformations Secondary to Abnormal Postmigrational Development
- •Selected References
- •Anencephaly
- •Holoprosencephaly
- •Holoprosencephaly Variants
- •Related Midline Disorders
- •Holoprosencephaly Mimics
- •Selected References
- •Selected References
- •Selected References
- •Cephaloceles
- •Craniosynostoses
- •Meningeal Anomalies
- •Selected References
- •Index

Chapter 20
607
Pineal and Germ Cell Tumors
The pineal region is located in the middle of the brain. Because there are so many critical structures that surround this small gland, operating on pineal region lesions poses a challenge to neurosurgeons, and accurate preoperative assessment is essential. The posterior third ventricle, midbrain, thalamus, vein of Galen, internal cerebral vein, quadrigeminal plate, and tentorial apex are all critical structures in the adjacent "neighborhood."
The pineal gland consists of pineal parenchymal cells, astrocytes, and sympathetic neurons. A number of other cells can also be found adjacent to the pineal gland. These include ependymal cells (lining the third ventricle), choroid plexus cells, arachnoid cells that form the velum interpositum, and astrocytes in the brainstem, thalamus, and corpus callosum splenium.
Lesions of the pineal region include a broad spectrum of both neoplasms and nonneoplastic entities. This histologic diversity reflects the broad range of normal cell types that reside within the gland and its adjacent structures.
The pineal region may also be the site of neoplasms that are more commonly found elsewhere. Metastases, neuronal tumors, endothelial tumors, and lymphomas are all occasionally seen. Congenital lesions such as epidermoid and dermoid cysts as well as lipomas can also occur.
Overall, pineal region tumors are rare, accounting for 1-3% of all intracranial neoplasms. Despite their histologic complexity, neoplasms in this region can be grouped into three simple overarching categories. The two most important groups arise from cells within the pineal gland itself: (1) tumors of pineal parenchymal cells and (2) germ cell tumors (GCTs).
The third group of pineal region lesions is composed of tumors of "other cell" origin. These include metastases and rare tumors that arise from pineal astrocytes or ependyma-like cells. Tumors and nonneoplastic masses may also arise from adjacent structures in close proximity. They include entities such as tentorial apex meningioma, aneurysmal dilatation of the vein of Galen, and nonneoplastic cysts (including cysts of the pineal gland itself).
We begin our discussion with a brief review of normal gross and imaging anatomy of the pineal region. Understanding normal pineal region anatomy is critical for correct imaging diagnosis. The differential diagnoses are very different for a mass inside the pineal gland versus a mass that lies in the same general region but is outside the gland.
We then turn our attention to the two major groups of neoplasms, pineal parenchymal tumors and GCTs. GCTs occupy a separate category in the WHO classification. However, because the pineal gland is by far the most common site for GCTs and because the differential diagnosis of an intrinsic pineal
Pineal Region Anatomy and |
|
Histology |
608 |
Gross Anatomy |
608 |
Normal Imaging |
610 |
Histology |
611 |
Pineal Parenchymal Tumors |
611 |
Pineocytoma |
612 |
Pineal Parenchymal Tumor of |
614 |
Intermediate Differentiation |
|
Pineoblastoma |
616 |
Papillary Tumor of the Pineal |
618 |
Region |
|
Germ Cell Tumors |
619 |
Overview of Germ Cell Tumors |
619 |
Germinoma |
621 |
Teratoma |
625 |
Other Germ Cell Neoplasms |
628 |
"Other Cell" Pineal and Pineal |
|
Region Neoplasms |
630 |
Miscellaneous Pineal Neoplasms |
630 |
Miscellaneous Pineal Region |
630 |
Masses |
|
|
|

Neoplasms, Cysts, and Tumor-Like Lesions
608
(20-1) Sagittal midline section demonstrates the anatomic complexity of the pineal region. The pineal gland is adjacent to the tentorial apex and vein of Galen , lying behind the third ventricle below the velum interpositum (VI) . The VI lies below the fornix, contains the internal cerebral veins, and helps form the roof of the third ventricle. (Courtesy M. Nielsen, MS.)
gland tumor includes both pineal parenchymal tumors and pineal GCTs, we consider them together in this chapter.
We close our discussion with a brief discussion of "other cell" tumors in the pineal gland and a differential diagnosis of pineal region masses.
Pineal Region Anatomy
and Histology
The pineal region is located under the falx cerebri, near its confluence with the tentorium cerebelli. This anatomically complex region encompasses the pineal gland itself, adjacent CSF spaces (the third ventricle and subarachnoid cisterns), brain parenchyma (corpus callosum splenium, quadrigeminal plate, upper vermis), arteries (medial and lateral posterior choroidal), veins (internal cerebral veins, vein of Galen), dural sinuses (inferior sagittal sinus, straight sinus), and meninges (dura and arachnoid) (20-1).
Gross Anatomy
We begin our discussion of the pineal region with the pineal gland itself, then consider its relationship to the normal structures that surround it.
Pineal Gland
The pineal gland, also called the hypophysis cerebri, is a small round or triangular endocrine organ that nestles between the superior colliculi. It is attached to the diencephalon and posterior wall of the third ventricle by the pineal stalk. It has other connections to the habenular and posterior commissures. The pineal gland also connects with other important structures, including the hypothalamus, hippocampi, amygdala, and brainstem.
The main vascular supply to the pineal gland is derived from branches of the medial posterior choroidal artery. The gland lacks a capillary blood-brain barrier.
Microscopically, 95% of the pineal gland consists of specialized neurons called pinealocytes that are arranged in cords or lobules separated by a fibrovascular stroma. Pinealocytes have both photosensory and neuroendocrine functions. The pinealocytes are interspersed with astrocytes and numerous

Pineal and Germ Cell Tumors
609
(20-2) Sagittal graphic depicts the normal anatomy of the pineal region. The pineal gland abuts the posterior third ventricle and lies below the fornix , velum interpositum , and internal cerebral vein .
blood vessels. Fine sand-like calcifications are commonly deposited within the pineal parenchyma.
The major hormone produced by the pineal gland is melatonin. Melatonin plays an important role in the synchronization of seasonal reproductive rhythms and entrainment of circadian cycles. Influenced by the dark/light cycle, the protein-coupled metabotropic melatonin receptors MT1 and MT2 are the primary mediators of its physiologic actions.
Third Ventricle and Commissures
The pineal gland abuts the posterior third ventricle. The third ventricle has two small posterior CSF outpouchings that abut the pineal gland. The more prominent supra-pineal recess lies above the pineal gland and below the corpus callosum splenium. The smaller pineal recess points posteriorly, directly into the gland.
Two commissural fiber tracts relate to the pineal gland. The habenular commissure lies just above the pineal gland, immediately below the suprapineal recess. The posterior commissure lies below the gland.
Fornix
The fornices are part of the limbic system. The two fornices, together with the fimbria, are the smallest and innermost of three nested C-shaped arches that surround the diencephalon and basal ganglia. The fornices provide the primary efferent outputs from the hippocampus.
Each fornix has four parts. The crura arch under the corpus callosum splenium forms part of the medial wall of the lateral ventricles. The commissure connects the two crura, which
(20-3) Axial graphic shows the velum interpositum opened into the roof of the third ventricle, paired internal cerebral veins, and vein of Galen .
then converge to form the body. The body is attached to the inferior surface of the corpus callosum. The bodies of the fornices curve inferiorly, forming the columns or "pillars" of the fornices. The fornices terminate in the mammillary bodies.
The commissure and bodies of the fornices lie above the velum interpositum (VI), internal cerebral veins, and pineal gland (20-2).
Velum Interpositum
The tela choroidea is a thin translucent bilaminar membrane that forms the VI (20-1). The VI stretches (and thus is "interposed") between the bodies of the two fornices. The VI forms the roof of the third ventricle and is closed anteriorly at the foramen of Monro. If it is open posteriorly, it forms a CSFfilled space that communicates directly with the quadrigeminal cistern. This normal variant is called a cavum of the velum interpositum or cistern of the velum interpositum.
The VI extends laterally over the thalami, where it becomes "tacked down" at the choroid fissures and continuous with the choroid plexus of the lateral ventricles. The VI covers the pineal gland and habenular commissure but is not directly attached to these structures.
Quadrigeminal Cistern
The quadrigeminal cistern is a rhomboid-shaped CSF space that lies dorsal to the tectal (quadrigeminal) plate and pineal gland. It is continuous inferiorly with the superior vermian cistern and laterally with the two ambient cisterns. Anteriorly it connects directly with the cistern of the VI.
Neoplasms, Cysts, and Tumor-Like Lesions
610
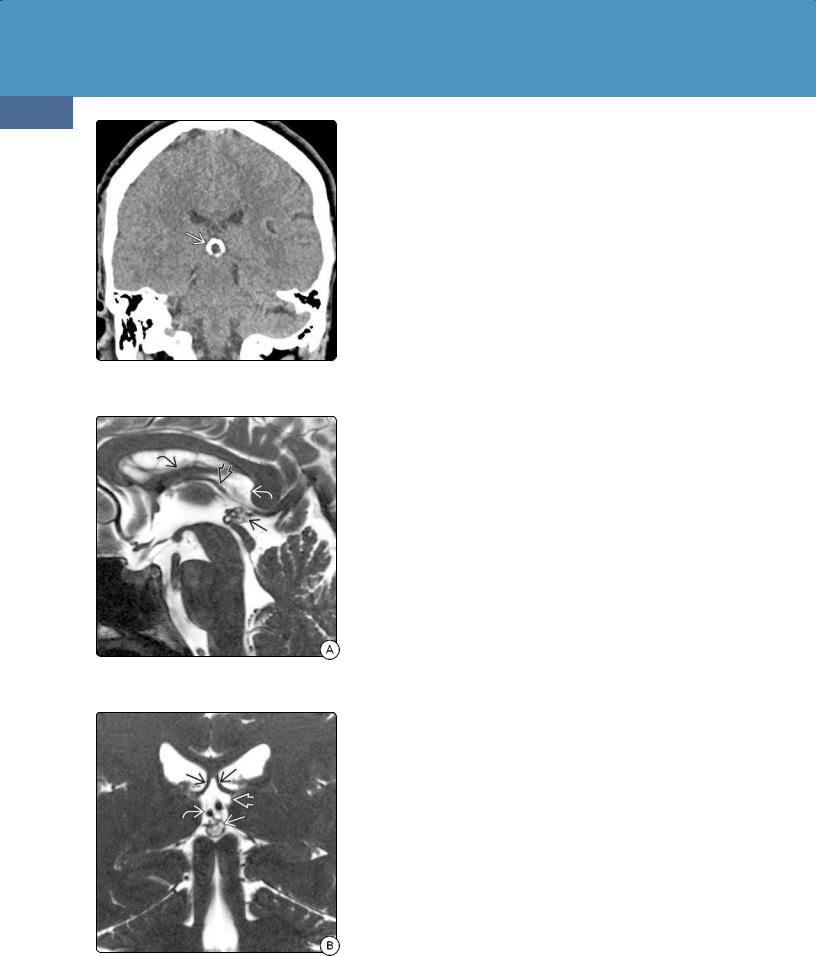
(20-4) Coronal NECT in a patient with minor head injury shows a 14-mm Ca++ cystic pineal gland. This is a normal variant.
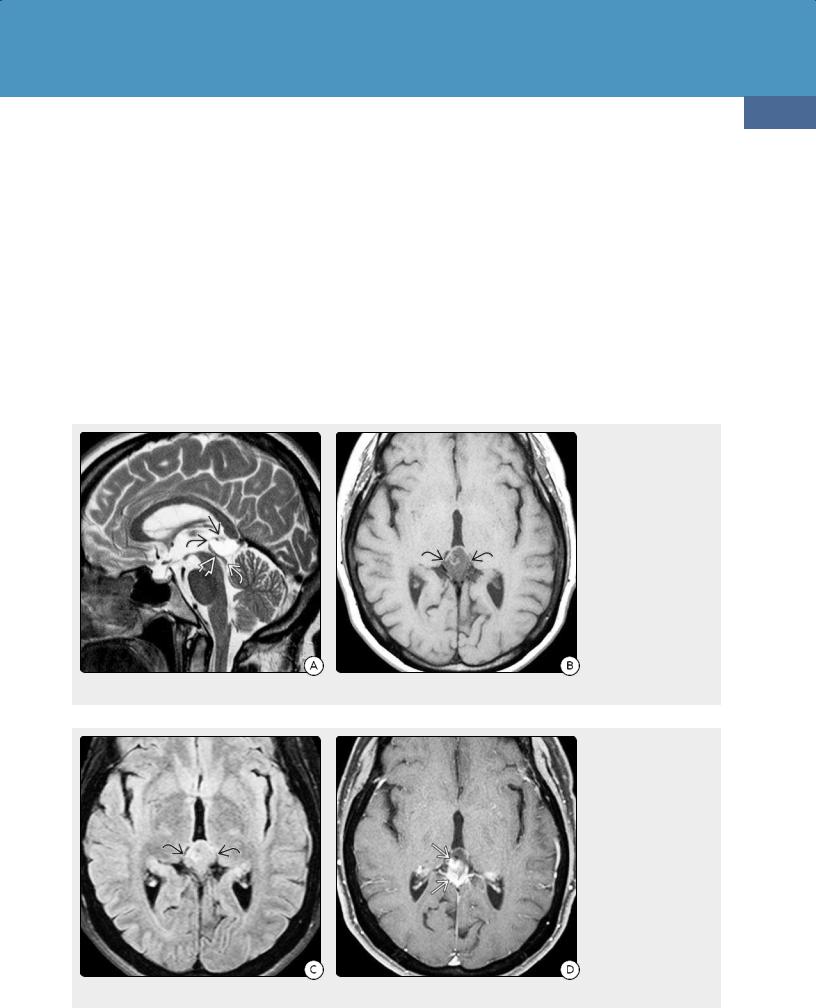
(20-5A) Sagittal T2WI shows multicystic pineal gland behind third ventricle, below ICV , velum interpositum , and fornix .
(20-5B) Coronal T2WI shows pineal gland below internal cerebral veins , velum interpositum , and fornices .
Meninges
Infoldings of the inner (meningeal) layer of the dura form the falx cerebri and tentorium cerebelli. These two dural leaves unite just behind the corpus callosum splenium to form the falcotentorial junction.
A loosely adherent, thin, almost transparent layer of arachnoid closely follows the dura and forms the outer border of the subarachnoid spaces. The arachnoid does not invaginate into the sulci or CSF cisterns.
Veins and Venous Sinuses
The internal cerebral veins (ICVs) are paired, paramedian veins that course posteriorly between the dorsal and ventral membranous layers of the VI. The ICVs terminate in the quadrigeminal cisterns by uniting with each other and the basal veins of Rosenthal to form the great cerebral vein of Galen (20-3). The ICVs lie above the pineal gland, which lies anteroinferior to the vein of Galen (20-2).
The inferior sagittal sinus (ISS) courses posteriorly along the inferior (free) margin of the falx cerebri. The ISS and vein of Galen unite at the falcotentorial junction to form the straight sinus. The falcotentorial junction, together with the leaves of the tentorium cerebelli, forms the "roof" of the quadrigeminal cistern.
Arteries
The medial posterior choroidal arteries arise from the P2 segments of the posterior cerebral arteries. They curve laterally around the brainstem, enter the tela choroidea, and run anteromedially along the roof of the third ventricle. Branches of the medial posterior choroidal arteries provide the main arterial supply to the pineal gland.
Parenchyma
The corpus callosum splenium lies above and behind the pineal gland. The tectal (quadrigeminal) plate lies below it. The thalami lie inferolateral to the pineal gland.
Normal Imaging
Pineal Calcification on NECT
Physiologic pineal gland calcification ("concretions") is common (20-4). Primary mineralization occurs in an organic matrix formed by pinealocytes. Pineal calcification increases with age. Reported prevalence is 1% in children under age 6 years, 8% in patients under age 10, and 40% in patients under 30. More than half of all adults have calcified pineal glands.
The diameter of normal pineal glands is usually ≤ 10 mm, but glands measuring 14-15 mm are not uncommon.
MR of the Pineal Region
Thin-section, small field-of-view sagittal T2WI is the ideal sequence for imaging the pineal gland and adjacent structures. The contrast between CSF in the posterior third ventricle in front, the velum interpositum above, and the quadrigeminal cistern posteriorly allows maximum delineation of the gland (20-5).
An easy way to recall the relationship of the pineal gland to its adjacent structures can be identified using sagittal T2WI. From top down, the mnemonic "famous V.I.P." identifies the fornix, velum interpositum, internal

Pineal and Germ Cell Tumors
cerebral veins, and pineal gland. Lesions in the fornix, VI, and ICVs will all displace the pineal gland inferiorly.
Lesions that arise from the tectal plate displace the pineal gland anterosuperiorly, whereas third ventricle masses displace it posteriorly. Knowing the normal gross anatomy helps make it simple!
Histology
The pineal gland has a unique morphology that differs considerably from the rest of the CNS. The gland is encased in a pial capsule and exhibits a loosely lobulated arrangement with a prominent intralobular fibrovascular and glia stroma.
The normal pineal gland is densely cellular and is composed mainly of pinocytes surrounded by connective tissue septa. Pinocytes are a specialized type of neuroepithelial cell, closely related to neurons, that have photosensory and neuroendocrine functions. Pinocytes stain avidly with neuronal immunohistochemical markers (e.g., synaptophysin and neurofilament protein).
At least four other cell types have been identified in the pineal gland, including interstitial cells and small numbers of fibrillary astrocytes.
Germ cells are not normal pineal gland constituents, and primitive germ cell elements are not found in fetal pineal glands. The theory that germ cell neoplasms arise from primordial germ cells that failed to migrate properly during the first few weeks of embryonic development is probably incorrect. More recent hypotheses implicate native stem cells of pluripotent or neural type as the source of neoplastically transformed germ cell elements.
Pineal Parenchymal Tumors
In North America and Europe, pineal region tumors represent less than 1% of all primary intracranial neoplasms but 3-8% of pediatric tumors. In Asia, they account for 3-3.5% of brain tumors. Despite their rarity, a broad spectrum of neoplasms can arise from the pineal gland itself or structures that are in its vicinity.
Most tumors of the pineal gland are germ cell neoplasms, which account for approximately 40% of all pineal tumors and are discussed separately. Pineal parenchymal tumors (PPTs) are intrinsic primary neuronal tumors that arise from pinealocytes or their precursors. PPTs account for less than 0.2% of all brain tumors but cause approximately 15-30% of pineal gland tumors.
PPT grading is based on the presence or absence of mitoses and neurofilament staining. Three grades are recognized: (1) pineocytoma, (2) pineal parenchymal tumor of intermediate differentiation (PPTID), and
(3) pineoblastoma, the most malignant parenchymal cell tumors.
In the most recent epidemiologic studies, pineocytomas account for 13-15% of pineal parenchymal neoplasms (probably an underrepresentation, as many presumed cases are not resected or biopsied). PPTIDs represent nearly two-thirds of cases, and pineoblastomas account for approximately 20%.
The very rare papillary tumor of the pineal region (PTPR), with which we conclude our discussion of PPTs, resembles pineocytoma but actually arises from the subcommissural organ.
611
(20-6) Graphic depicts pineocytoma. The cystic center is lined by a rim of solid, partially calcified tumor . Hemorrhage is not uncommon.
(20-7) Autopsy case shows pineocytoma as a welldemarcated lobulated mass behind the third ventricle . (Courtesy B. Horten, MD.)
(20-8) Resected pineocytoma shows multiple cysts , solid nodules , and intratumoral hemorrhage . (Courtesy R. Hewlett, MD.)

Neoplasms, Cysts, and Tumor-Like Lesions
612
Pineocytoma
Terminology
Pineocytoma is a slow-growing and well-differentiated PPT composed of mature cells that resemble normal pinealocytes.
Etiology
The ontogeny of the human pineal gland recapitulates the phylogeny of the retina and the pineal organ. PPTs mimic the developmental stages of the pineal gland, with immunoexpression profiles that indicate that they are biologically linked to pinealocytes.
No consistent genetic mutations have been described to date, and no definite relationship of pineocytoma with the RB1 gene has been established. No syndromic associations have been demonstrated.
(20-9A) NECT scan shows the typical findings of pineocytoma. The cysticappearing pineal mass "explodes" calcifications toward the periphery of the lesion . (20-9B) T2WI in the same patient shows a cyst surrounded by a thin rim of solid tissue .
(20-9C) FLAIR scan shows that the cyst wall is mildly hyperintense and that the cyst fluid does not suppress. (20-9D) T1 C+ FS demonstrates that the cyst wall enhances . This is pathologically proven pineocytoma, WHO grade I.
Pathology
Location and Size. Pineocytomas are located behind the third ventricle and rarely invade it or adjacent structures (20-6) (20-7). Pineocytomas vary in size. Although "giant" tumors have been reported, most are smaller than 3 cm in diameter.
Gross Pathology. Pineocytomas are well-circumscribed, round or lobular, gray-tan masses that may display intratumoral cysts or hemorrhagic foci (20-8).
Microscopic Features. Pineocytomas are composed of small uniform cells that closely resemble pinealocytes. Large "pineocytomatous rosettes" are the most characteristic feature.
Immunopositivity for neuronal markers such as synaptophysin, neuron-specific enolase, and neurofilament protein (NFP) is typical.
Pineocytoma and the normal pineal gland may appear very similar, and histologic differentiation between the two may be difficult, especially in small tissue samples.
Staging, Grading, and Classification. Pineocytoma is positive for both synaptophysin and neurofilament and shows no mitoses. Pineocytomas are WHO grade I neoplasms.
Clinical Issues
Epidemiology. Pineocytoma is the most common PPT, accounting for 15-60% of all primary PPTs.
Demographics. Pineocytomas occur at all ages but are mostly tumors of adults. Mean age at diagnosis is 43 years. There is a slight female predominance (M:F = 0.6:1).
Presentation. Many small pineocytomas are discovered incidentally on imaging studies. Larger lesions may compress adjacent structures or cause hydrocephalus. Headache and
Pineal and Germ Cell Tumors
613
Parinaud syndrome (paralysis of upward gaze) are common in symptomatic patients.
Natural History. Pineocytomas grow very slowly and often remain stable in size over many years. Gross total resection is the major prognostic factor with reported 5-year survival rates between 90 and 100%.
Treatment Options. "Watchful waiting" is common with small lesions. Imaging is usually obtained only if the patient's symptoms change. Complete surgical resection is generally curative, without recurrence or metastatic tumor spread.
Imaging
CT Findings. Pineocytomas are globular, well-delineated masses that are mixed isoto hypodense on NECT scans. Calcifications typically appear "exploded" toward the periphery of the pineal gland (20-9A).
(20-10A) Sagittal T2WI in a 58y woman with headaches and a normal neurologic examination shows a mixed cystic and solid pineal mass that compresses the tectal plate . The cerebral aqueduct is patent. (20-10B) Axial T1WI in the same case shows that the cystic portion of the massis hyperintense compared with CSF in the adjacent third ventricle.
(20-10C) Axial FLAIR MR in the same case shows that fluid in the cyst does not suppress. There is no evidence for obstructive hydrocephalus. (20-10D) Axial T1 C+ FS MR shows strong but heterogeneous enhancement in the solid portions of the mass . The lesion has remained stable for several years. This is presumed (not proven) pineocytoma.

Neoplasms, Cysts, and Tumor-Like Lesions
614
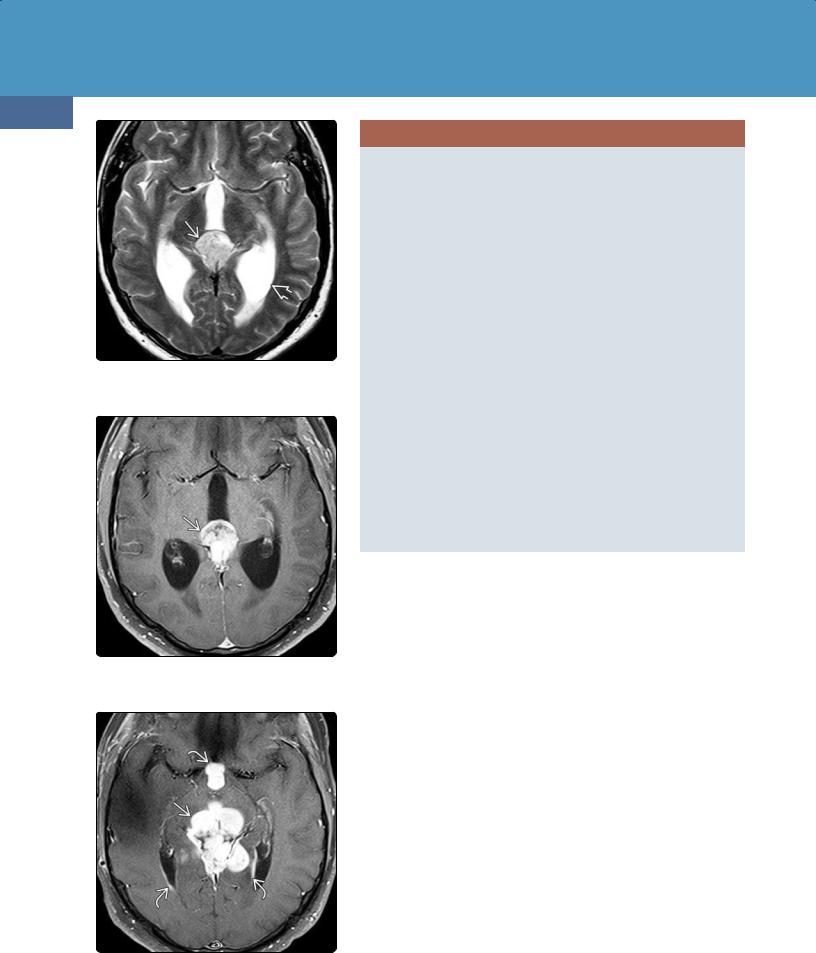
(20-11A) Axial T1WI in a 57y man with headaches shows a lobulated mixed iso-/hypointense pineal mass causing obstructive hydrocephalus.
(20-11B) An axial T2WI scan in the same case shows both solid and cystic portions of the mass.
(20-11C) Axial T1 C+ FS scan shows the solid portions of the mass and cyst enhance strongly. This is PPTID, WHO grade II.
MR Findings. Pineocytomas are well-demarcated round or lobular masses that are isoto hypointense on T1WI and hyperintense on T2WI and FLAIR (20-9B) (20-9C). T2* GRE may show "blooming" foci secondary to calcification or hemorrhage. Pineocytomas typically enhance avidly with solid, rim, or even nodular patterns (20-9D) (20-10).
Differential Diagnosis
The major differential diagnosis of pineocytoma is a benign, nonneoplastic pineal cyst. Pineal cysts may be indistinguishable from pineocytomas on imaging studies. Germinoma typically "engulfs" rather than "explodes" the pineal calcifications, is most common in male adolescents, and enhances intensely and uniformly. Pineal parenchymal tumor of intermediate differentiation (PPTID) is a tumor of middle-aged and older patients. The imaging appearance of PPTIDs is more "aggressive" than that of pineocytoma (see below).
PINEOCYTOMA
Pathology
•Most 1-3 cm
•Well-demarcated, round/lobulated
•WHO grade I
Clinical Issues
•Adults (mean = 40 years)
•Grows very slowly, often stable for years
Imaging
•CT
○Mixed iso-/hypodense
○Pineal Ca++ "exploded"
•MR
○Iso-/hypointense on T1, hyperintense on T2
○Cysts common, may hemorrhage
○Variable enhancement (solid, rim, nodular)
Differential Diagnosis
•Benign pineal cyst (may be indistinguishable)
•Germinoma ("engulfs" Ca++, male adolescents)
•PPTID (more "aggressive looking")
Pineal Parenchymal Tumor of Intermediate
Differentiation
Some pineal lesions both look worse and behave more aggressively than pineocytomas but are still less malignant than pineoblastomas. In 2007, the WHO formally recognized a new tumor, pineal parenchymal tumor of intermediate differentiation (PPTID), which is intermediate in malignancy between pineocytoma and pineoblastoma.
Terminology
PPTID supersedes the terms "atypical" or "aggressive" pineocytoma.
Pathology
Grossly, PPTID is a large, heterogeneous mass with peripheral calcification and variable cystic changes. Microscopically, PPTIDs are moderate to highly cellular tumors that exhibit dense lobular architecture. Two morphologic subtypes, small cell and large cell, have been recently described.

Pineal and Germ Cell Tumors
PPTIDs can be either WHO grade II or III although definite histologic grading criteria remain to be defined.
Clinical Issues
Epidemiology and Demographics. PPTIDs are the most common pineal parenchymal tumor, representing between half and two-thirds of all cases. PPTIDs can occur at any age but are typically tumors of middle-aged adults.
Natural History. Diplopia, Parinaud syndrome, and headache are the most common presenting symptoms. Biologic behavior is variable, and long-term survival—even with subtotal resection—is common. Tumors tend to enlarge slowly over many years and recur locally although CSF dissemination may occur.
Treatment Options. Treatment of PPTID is controversial. Stereotactic biopsy followed by surgical resection is the most common treatment. The role of adjuvant chemotherapy or radiotherapy is undetermined.
Imaging
General Features. PPTIDs have a more "aggressive" imaging appearance than pineocytoma (20-11). Extension into adjacent structures (e.g., the ventricles and thalami) is common. Size varies from less than 1 cm to large masses that are 4-6 cm in diameter. CSF dissemination is uncommon but does occur, so imaging evaluation of the entire neuraxis should be performed prior to surgical intervention.
CT Findings. NECT scans show a hyperdense mass that "engulfs" pineal gland calcifications. PPTIDs generally enhance strongly and uniformly.
MR Findings. PPTIDs are mixed isoand hypointense on T1WI, isointense with gray matter on T2WI, and hyperintense on FLAIR. T2* (GRE, SWI) scans may show hypointense "blooming" foci. Enhancement is generally strong but heterogeneous on T1 C+ (20-12). MRS shows elevated Cho and decreased NAA. A lactate peak may be present.
Differential Diagnosis
The major differential diagnosis of PPTID is pineocytoma. A more aggressive-appearing pineal mass in a middle-aged or older adult is most consistent with PPTID. Pineoblastoma is typically a tumor of younger patients. Germinoma is more common in male adolescents. Papillary tumor of the pineal region can appear identical on imaging studies but is very rare.
PINEAL PARENCHYMAL TUMOR OF INTERMEDIATE
DIFFERENTIATION
Pathology
•50-68% of pineal parenchymal tumors
•WHO grade II or III
Clinical Issues
• Middle-aged adults
Imaging
•Appears more "aggressive" than pineocytoma
•Usually larger, more heterogeneous
•May disseminate via CSF
Differential Diagnosis
•Pineocytoma > > pineoblastoma
•Germinoma
615
(20-12A) Axial T1WI in a 21y man with Parinaud syndrome shows a large heterogeneous mass causing moderate obstructive hydrocephalus.
(20-12B) T2WI shows numerous hyperintense cysts and solid isointense nodules comprising the mass .
(20-12C) T1 C+ FS shows strong enhancement of the solid portions of the mass and cyst walls. Pathology was PPTID, WHO grade III.

Neoplasms, Cysts, and Tumor-Like Lesions
616
(20-13) Sagittal graphic depicts pineoblastomawith CSF dissemination into ventricles , subarachnoid spaces .
(20-14) Autopsied pineoblastoma shows dissemination with metastases coating lateral, third ventricles . (Courtesy B. Horten, MD.)
(20-15) Pineoblastoma is composed of sheets of small blue undifferentiated cells with occasional rosettes . (Courtesy B. K. DeMasters, MD.)
Pineoblastoma
Terminology
Pineoblastoma (PB) is a poorly differentiated, highly embryonal neoplasm of the pineal gland.
Etiology
Along with the less malignant pineal parenchymal tumors, PBs share morphologic and immunohistochemical features with embryonic cells of the developing human pineal gland and retina.
PBs are known to occur in patients with RB1 gene abnormalities. PBs also occur in patients with familial (bilateral) retinoblastoma (the so-called "trilateral retinoblastoma syndrome"), and cases have been reported in familial adenomatous polyposis. Patients with DICER1 syndrome are at increased risk for developing PBs.
Pathology
Gross Pathology. A soft, friable, diffusely infiltrating tumor that invades adjacent brain and obstructs the cerebral aqueduct is typical (20-13). Necrosis and intratumoral hemorrhage are common, as is CSF dissemination with sheet-like coating of the brain and spinal cord (20-14).
Microscopic Features. PBs are highly cellular neoplasms that resemble other embryonic neoplasms. Undifferentiated small round blue cells with hyperchromatic nuclei and a high nuclear-to-cytoplasmic ratio are the dominant histologic feature of PB. Occasional Homer-Wright rosettes (neuroblastic differentiation) or Flexner-Wintersteiner rosettes (retinoblastic differentiation) can be identified (20-15). Mitotic activity varies but is generally high.
Staging, Grading, and Classification. PB are WHO grade IV neoplasms.
Clinical Issues
Epidemiology. PBs comprise 0.5-1.0% of primary brain tumors, 15% of pineal region neoplasms, and 20-35% of pineal parenchymal tumors.
Demographics. Although they can occur at any age, PBs are decidedly more prevalent in children. Most present in the first two decades.
Presentation. Symptoms of elevated intracranial pressure such as headache, nausea, and vomiting are typical. Parinaud syndrome is common.
Natural History. PBs are the most primitive and biologically aggressive of all the pineal parenchymal tumors. Prognosis is poor with a median survival of 16-25 months. CSF dissemination is frequent at the time of initial diagnosis and the most common cause of death.
Treatment Options. Surgical debulking with adjuvant chemotherapy and craniospinal radiation comprise the typical regimen.
Imaging
General Features. PBs are large, bulky, aggressive-looking pineal region masses that invade adjacent brain and usually cause obstructive hydrocephalus. CSF dissemination is common, so the entire neuraxis should be imaged prior to surgical intervention.
CT Findings. A large, hyperdense, inhomogeneously enhancing mass with obstructive hydrocephalus is typical. If pineal calcifications are present, they appear "exploded" toward the periphery of the tumor (20-16A).

MR Findings. PBs are heterogeneous tumors that frequently demonstrate necrosis and intratumoral hemorrhage. They are usually mixed isoto hypointense compared with brain on T1WI and mixed isoto hyperintense on T2WI (20-17). They enhance strongly but heterogeneously. Because they are densely cellular tumors, restriction on DWI is common (2016B).
Differential Diagnosis
The major differential diagnosis of PB is PPTID. PBs tend to occur in children. CSF dissemination at diagnosis is more common. Germinoma may mimic PB on imaging studies, as it also frequently demonstrates CSF spread. Germinomas are more common in adolescent and young adult male patients. They tend to "engulf" rather than "explode" pineal calcifications.
Nongerminomatous malignant germ cell tumors are a heterogeneous group of tumors that may be indistinguishable
Pineal and Germ Cell Tumors
617
on imaging studies from PBs. Elevated tumor markers such as α-fetoprotein and β-human chorionic gonadotropin—all usually negative in germinoma and PB—are helpful in establishing the diagnosis.
Pineal anlage tumors are a peculiar, very rare malignant pineal tumor of infants and young children. Pineal anlage tumors exhibit both PB-like neuroectodermal and ectomesenchymal elements (striated muscle, fibrous and adipose tissue, and cartilaginous islands). No endodermal components are present, distinguishing these unusual tumors from teratomas.
Imaging shows a mixed solid and cystic pineal region mass that typically causes obstructive hydrocephalus. Imaging findings are indistinguishable from other pineal parenchymal tumors such as pineocytoma and PPTID. Age is the only characteristic suggesting this rare neoplasm.
(20-16A) NECT of pineoblastoma shows an ill-defined, slightly hyperdense pineal region mass causing obstructive hydrocephalus. Some calcifications are seen toward the periphery of the mass. (20-16B) DWI in the same patient shows moderate diffusion restriction, consistent with high cellularity.
(20-17A) T2WI in another patient with pineoblastoma shows a large pineal mass that causes severe obstructive hydrocephalus. (20-17B) T1 C+ scan in the same patient shows that the lesion enhances intensely, uniformly. (Courtesy R. Hewlett, MD.)
Neoplasms, Cysts, and Tumor-Like Lesions
618
(20-18) T2WI in 43y man w/ headache, nausea, vomiting for 11 days shows hyperintense pineal mass , acute obstructive hydrocephalus .
(20-19) T1 C+ FS shows mass enhances intensely, heterogeneously, no evidence for CSF spread. This is pineoblastoma, WHO grade IV.
(20-20) The patient deteriorated 5 weeks later. Repeat T1 C+ FS shows mass has increased significantly, and there is CSF dissemination .
PINEOBLASTOMA
Etiology
•Cells of embryonic pineal gland/retina
•Genetic susceptibility
○RB1 mutation
○Familial adenomatous polyposis
○DICER1 germline mutation
Pathology
•Most primitive, malignant of all PPTs
•Diffusely infiltrates adjacent structures
•Early, widespread CSF dissemination common
•WHO grade IV
Clinical Issues
•15% of pineal region tumors
•20-35% of PPTs
•All ages but primarily children (< 20 years old)
•Prognosis generally poor
Imaging
•CT
○Inhomogeneously hyperdense
○Ca++ "exploded"
•MR
○Large, bulky, aggressive-looking
○Necrosis, intratumoral hemorrhage common
○Enhances strongly, heterogeneously
○Restricts on DWI (densely cellular)
○Look for CSF spread (image entire neuraxis)
Papillary Tumor of the Pineal Region
Papillary tumor of the pineal region (PTPR) is a rare neuroepithelial tumor that arises from the subcommissural organ in the posteroinferior wall of the third ventricle (20-21). PTPRs are adult tumors; mean age at diagnosis is 32 years.
Typical chromosomal alterations as well as specific DNA methylation and mRNA expression profiles have been recently delineated that allow differentiation of PTPR from close histopathologic mimics such as ependymoma and PPTID. Chromosome 10 losses are the most common genetic alteration. Several subcommissural organ-related genes such as transcription factor SPDEF are overexpressed in PTPRs.
Macroscopically, PTPRs are indistinguishable from pineocytoma although they are easily differentiated microscopically. PTPRs show distinct papillary architecture with pseudostratified columnar epithelium. Grading of PTPRs has yet to be defined, but, in the 2016 WHO, PTPRs correspond to grade II or III neoplasms.
Outcome is complicated by local recurrence. Two subgroups with differential methylation profiles have been identified. Progression-free survival in patients with a low frequency of hypermethylated genes is nearly three times longer than those with higher methylation levels (125 months vs. 43 months, respectively).
Only a few PTPRs with imaging findings have been reported. PTPRs tend to be large, relatively well circumscribed, and often partially cystic. Strong but heterogeneous enhancement is typical (20-22). No features that would distinguish these tumors from pineal parenchymal tumors of intermediate
