
- •Foreword I
- •Foreword II
- •Preface
- •Contents
- •1 Abscesses – Pyogenic Type
- •3 Cyst I – Typical Small
- •4 Cyst II – Typical Large with MR-CT Correlation
- •5 Cyst III – Multiple Small Lesions with MR-CT-US Comparison
- •6 Cyst IV – Adult Polycystic Liver Disease
- •7 Cystadenoma / Cystadenocarcinoma
- •8 Hemangioma I – Typical Small
- •10 Hemangioma III – Typical Giant
- •11 Hemangioma IV – Giant Type with a Large Central Scar
- •13 Hemangioma VI – Multiple with Perilesional Enhancement
- •14 Hemorrhage
- •16 Mucinous Metastasis – Mimicking an Hemangioma
- •17 Colorectal Metastases I – Typical Lesion
- •18 Colorectal Metastases II – Typical Multiple Lesions
- •19 Colorectal Metastases III – Metastasis Versus Cyst
- •20 Colorectal Metastases IV – Metastasis Versus Hemangiomas
- •21 Liver Metastases V – Large, Mucinous, Mimicking a Primary Liver Lesion
- •24 Breast Carcinoma Liver Metastases
- •25 Kahler’s Disease (Multiple Myeloma) Liver Metastases
- •26 Melanoma Liver Metastases I – Focal Type
- •27 Melanoma Liver Metastases II – Diffuse Type
- •28 Neuroendocrine Tumor I – Typical Liver Metastases
- •29 Neuroendocrine Tumor II – Pancreas Tumor Metastases
- •30 Neuroendocrine Tumor III – Gastrinoma Liver Metastases
- •31 Neuroendocrine Tumor IV – Carcinoid Tumor Liver Metastases
- •32 Neuroendocrine Tumor V – Peritoneal Spread
- •34 Renal Cell Carcinoma Liver Metastasis
- •35 Cirrhosis I – Liver Morphology
- •36 Cirrhosis II – Regenerative Nodules and Confluent Fibrosis
- •37 Cirrhosis III – Dysplastic Nodules
- •38 Cirrhosis IV – Dysplastic Nodules – HCC Transition
- •39 Cirrhosis V – Cyst in a Cirrhotic Liver
- •40 Cirrhosis VI – Multiple Cysts in a Cirrhotic Liver
- •41 Cirrhosis VII – Hemangioma in a Cirrhotic Liver
- •42 HCC in Cirrhosis I – Typical Small with Pathologic Correlation
- •43 HCC in Cirrhosis II – Small With and Without a Tumor Capsule
- •44 HCC in Cirrhosis III – Nodule-in-Nodule Appearance
- •45 HCC in Cirrhosis IV – Mosaic Pattern with Pathologic Correlation
- •47 HCC in Cirrhosis VI – Mosaic Pattern with Fatty Infiltration
- •48 HCC in Cirrhosis VII – Large Growing Lesion with Portal Invasion
- •49 HCC in Cirrhosis VIII – Segmental Diffuse with Portal Vein Thrombosis
- •50 HCC in Cirrhosis IX – Multiple Lesions Growing on Follow-up
- •51 HCC in Cirrhosis X – Capsular Retraction and Suspected Diaphragm Invasion
- •52 HCC in Cirrhosis XI – Diffuse Within the Entire Liver with Portal Vein Thrombosis
- •53 HCC in Cirrhosis XII – With Intrahepatic Bile Duct Dilatation
- •54 Focal Nodular Hyperplasia I – Typical with Large Central Scar and Septa
- •55 Focal Nodular Hyperplasia II – Typical with Pathologic Correlation
- •57 Focal Nodular Hyperplasia IV – Multiple FNH Syndrome
- •58 Focal Nodular Hyperplasia V – Fatty FNH with Concurrent Fatty Adenoma
- •59 Focal Nodular Hyperplasia VI – Atypical with T2 Dark Central Scar
- •60 Hepatic Angiomyolipoma – MR-CT Comparison
- •61 Hepatic Lipoma – MR-CT-US Comparison
- •62 Hepatocellular Adenoma I – Typical with Pathologic Correlation
- •63 Hepatocellular Adenoma II – Large Exophytic with Pathologic Correlation
- •64 Hepatocellular Adenoma III – Typical Fat-Containing
- •65 Hepatocellular Adenoma IV – With Large Hemorrhage
- •77 Intrahepatic Cholangiocarcinoma – With Pathologic Correlation
- •78 Telangiectatic Hepatocellular Lesion
- •79 Focal Fatty Infiltration Mimicking Metastases
- •80 Focal Fatty Sparing Mimicking Liver Lesions
- •81 Hemosiderosis – Iron Deposition, Acquired Type
- •82 Hemochromatosis – Severe Type
- •83 Hemochromatosis with Solitary HCC
- •84 Hemochromatosis with Multiple HCC
- •85 Thalassemia with Iron Deposition
- •86 Arterioportal Shunt I – Early Enhancing Lesion in a Cirrhotic Liver
- •89 Budd-Chiari Syndrome II – Gradual Deformation of the Liver
- •90 Budd-Chiari Syndrome III – Nodules Mimicking Malignancy
- •92 Caroli’s Disease I – Intrahepatic with Segmental Changes
- •93 Caroli’s Disease II – Involvement of the Liver and Kidneys
- •95 Choledocholithiasis (Bile Duct Stones)
- •96 Gallbladder Carcinoma I – Versus Gallbladder Wall Edema
- •97 Gallbladder Carcinoma II – Hepatoid Type of Adenocarcinoma
- •98 Hilar Cholangiocarcinoma I – Typical
- •99 Hilar Cholangiocarcinoma II – Intrahepatic Mass
- •100 Hilar Cholangiocarcinoma III – Partially Extrahepatic Tumor
- •101 Hilar Cholangiocarcinoma IV – Metal Stent with Interval Growth
- •102 Hilar Cholangiocarcinoma V – Biliary Dilatation Mimicking Klatskin Tumor at CT
- •103 Primary Sclerosing Cholangitis I – Cholangitis and Segmental Atrophy
- •104 Primary Sclerosing Cholangitis II – With Intrahepatic Cholestasis
- •105 Primary Sclerosing Cholangitis III – With Intrahepatic Stones
- •106 Primary Sclerosing Cholangitis IV – With Biliary Cirrhosis
- •107 Primary Sclerosing Cholangitis V – With Intrahepatic Cholangiocarcinoma
- •108 Primary Sclerosing Cholangitis VI – With Hilar Cholangiocarcinoma
- •109 T2 Bright Liver Lesions
- •110 T1 Bright Liver Lesions
- •111 T2 Bright Central Scar
- •112 Lesions in Fatty Liver
- •113 Appendix I: MR Imaging Technique and Protocol
- •114 Appendix II: Liver Segmental and Vascular Anatomy
- •Subject Index

32 Part I – High-Fluid Content Liver Lesions
16 Mucinous Metastasis – Mimicking an Hemangioma
Colorectal mucinous carcinoma is a histopathologic subtype of rectal adenocarcinoma, which is characterized by the production of an abundant amount of extracellular mucin. The incidence of the mucinous carcinomas varies between 10 % and 20 % of the total number of colorectal carcinomas. Mucinous carcinomas are known to be highly infiltrative lesions, which lead to a lower resection rate and a higher postoperative dissemination rate. These factors lead to a poorer prognosis in patients with the mucinous as compared with non-mucinous colorectal carcinomas. Because of higher fluid than solid content with concomitant less vascularity, the liver metastases of colorectal adenocarcinomas may mimic non-solid liver lesions such as cysts and hemangiomas at imaging. Particularly, MR imaging may facilitate the distinction of mucinous liver metastases from benign non-solid liver lesions.
Literature
1.Wu CS, Tung SY, Chen PC, Kuo YC (1996) Clinicopathologic study of colorectal mucinous carcinoma in Taiwan: a multivariate analysis. J Gastroenterol Hepatol 11:77 – 81
2.Ueda K, Matsui O, Nobata K, Takashima T (1996) Mucinous carcinoma of the liver mimicking cavernous hemangioma on preand postcontrast MR imaging [letter]. Am J Roentgenol 166:468 – 469
3.Outwater EK, Tomaszewski JE, Daly JM, Kressel HY (1991) Hepatic colorectal metastases; correlation of MR imaging and pathology. Radiology 180:327 – 332
MR Imaging Findings
Because of the abundant extracellular mucin, liver metastases of mucinous colorectal adenocarcinomas typically show predominantly high to very high signal on T2-weighted MR images. On T1-weighted images, the lesions often have unremarkable low signal intensity. After injection of gadolinium, mucinous liver metastases show enhancement of the intratumoral structures, including septa and vessels, in the arterial as well as delayed phases (Figs. 16.1, 16.2). Particularly at CT the enhancement of intratumoral structures may mimic the peripheral nodular enhancement and, in combination with signs such as a traversing vessel, may suggest a benign lesion such as hemangioma (Fig. 16.3A). In our experience, positron emission tomography (PET) may show no abnormal activity and may wrongfully suggest that CT findings are correct (Fig. 16.3B). In such cases, after MR imaging an US-guided biopsy or a resection of the liver lesion may show conclusive evidence of metastasis.
Pathology
At gross pathology, the lesions appear as solid pink lesions with sharp demarcation to the surrounding liver. At histology, the lesions show large spaces filled with abundant mucin. These spaces are interspersed with large septa containing vessels (Fig. 16.3C, D).
16 Mucinous Metastasis – Mimicking an Hemangioma 33
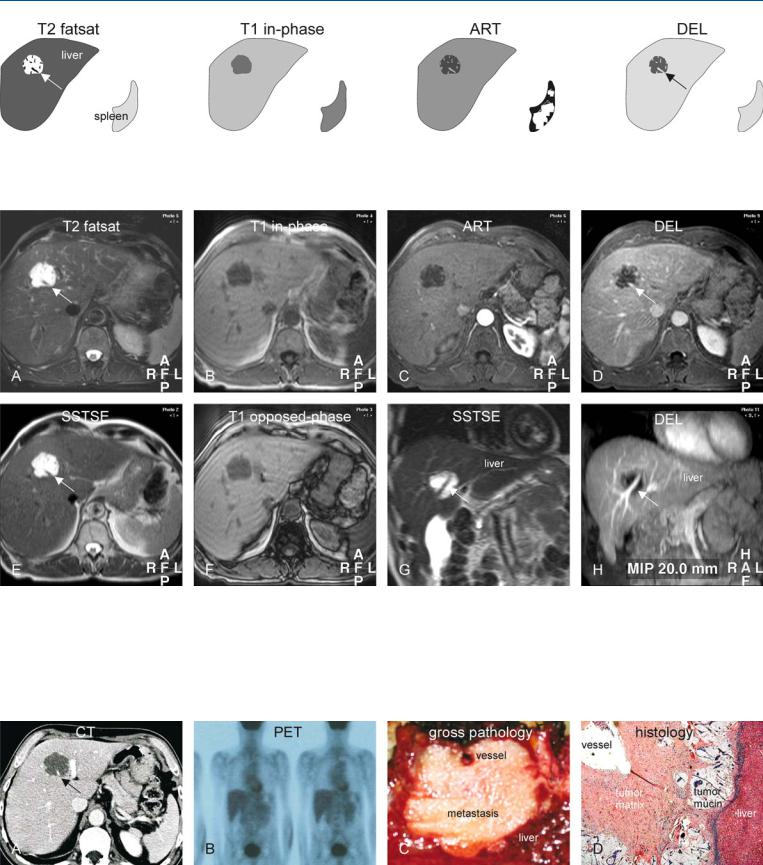
Fig. 16.1. Mucinous colorectal metastasis mimicking hemangioma, drawings.
T2 fatsat: metastasis is very bright containing low intensity structures, including a traversing vessel (arrow); T1 in-phase: metastasis is hypointense
Fig. 16.2. Mucinous colorectal metastasis mimicking hemangioma at CT: MRI findings. A Axial TSE image (T2 fatsat): Lesion is very bright and contains low intensity structures and a traversing vessel (arrow). B Axial in-phase image (T1 in-phase): Metastasis is hypointense to the liver. C Axial arterial phase image (ART): Intratumoral structures, including the vessel, show some enhancement; transversing vessel is often considered a sign of benign lesions. D Axial delayed phase image (DEL): Intratumoral structures and the
to the liver; ART: metastasis shows enhancement of low intensity structures and vessel; DEL: metastasis shows increased enhancement of the intratumoral structures and the vessel (arrow)
traversing vessel (arrow) are more enhanced. E Axial SSTSE image with a TE of 120 ms: metastasis retains its signal, which is a common finding of hemangioma and cysts. F Axial opposed-phase image (T1 opposed-phase) shows no change in the aspect of the liver, nor of the lesion. G Coronal SSTSE (SSTSE) shows metastasis with the traversing vessel (arrow). H Maximum intensity projection (MIP) of the delayed phase (DEL) provides an overview of the traversing liver vein (arrow)
Fig. 16.3. Mucinous colorectal metastasis with inconclusive CT and PET; MR-pa- thology correlation. A CT shows little enhancement, and in combination with the traversing vessel (arrow), the lesion was considered benign. B Positron emission tomography (PET) showed normal uptake in the liver. C Based on
MR imaging, the lesion was biopsied and then resected. Pathology confirmed a metastasis with a traversing vessel. D Photomicrograph shows the metastasis composed of tumor matrix, pools of mucin, and a traversing vessel. H&E stain, × 100

Part II
Solid Liver Lesions II

Part II/IIA
Solid Liver Lesions |
II |
Metastases: Colorectal |
IIA |
