
- •Foreword I
- •Foreword II
- •Preface
- •Contents
- •1 Abscesses – Pyogenic Type
- •3 Cyst I – Typical Small
- •4 Cyst II – Typical Large with MR-CT Correlation
- •5 Cyst III – Multiple Small Lesions with MR-CT-US Comparison
- •6 Cyst IV – Adult Polycystic Liver Disease
- •7 Cystadenoma / Cystadenocarcinoma
- •8 Hemangioma I – Typical Small
- •10 Hemangioma III – Typical Giant
- •11 Hemangioma IV – Giant Type with a Large Central Scar
- •13 Hemangioma VI – Multiple with Perilesional Enhancement
- •14 Hemorrhage
- •16 Mucinous Metastasis – Mimicking an Hemangioma
- •17 Colorectal Metastases I – Typical Lesion
- •18 Colorectal Metastases II – Typical Multiple Lesions
- •19 Colorectal Metastases III – Metastasis Versus Cyst
- •20 Colorectal Metastases IV – Metastasis Versus Hemangiomas
- •21 Liver Metastases V – Large, Mucinous, Mimicking a Primary Liver Lesion
- •24 Breast Carcinoma Liver Metastases
- •25 Kahler’s Disease (Multiple Myeloma) Liver Metastases
- •26 Melanoma Liver Metastases I – Focal Type
- •27 Melanoma Liver Metastases II – Diffuse Type
- •28 Neuroendocrine Tumor I – Typical Liver Metastases
- •29 Neuroendocrine Tumor II – Pancreas Tumor Metastases
- •30 Neuroendocrine Tumor III – Gastrinoma Liver Metastases
- •31 Neuroendocrine Tumor IV – Carcinoid Tumor Liver Metastases
- •32 Neuroendocrine Tumor V – Peritoneal Spread
- •34 Renal Cell Carcinoma Liver Metastasis
- •35 Cirrhosis I – Liver Morphology
- •36 Cirrhosis II – Regenerative Nodules and Confluent Fibrosis
- •37 Cirrhosis III – Dysplastic Nodules
- •38 Cirrhosis IV – Dysplastic Nodules – HCC Transition
- •39 Cirrhosis V – Cyst in a Cirrhotic Liver
- •40 Cirrhosis VI – Multiple Cysts in a Cirrhotic Liver
- •41 Cirrhosis VII – Hemangioma in a Cirrhotic Liver
- •42 HCC in Cirrhosis I – Typical Small with Pathologic Correlation
- •43 HCC in Cirrhosis II – Small With and Without a Tumor Capsule
- •44 HCC in Cirrhosis III – Nodule-in-Nodule Appearance
- •45 HCC in Cirrhosis IV – Mosaic Pattern with Pathologic Correlation
- •47 HCC in Cirrhosis VI – Mosaic Pattern with Fatty Infiltration
- •48 HCC in Cirrhosis VII – Large Growing Lesion with Portal Invasion
- •49 HCC in Cirrhosis VIII – Segmental Diffuse with Portal Vein Thrombosis
- •50 HCC in Cirrhosis IX – Multiple Lesions Growing on Follow-up
- •51 HCC in Cirrhosis X – Capsular Retraction and Suspected Diaphragm Invasion
- •52 HCC in Cirrhosis XI – Diffuse Within the Entire Liver with Portal Vein Thrombosis
- •53 HCC in Cirrhosis XII – With Intrahepatic Bile Duct Dilatation
- •54 Focal Nodular Hyperplasia I – Typical with Large Central Scar and Septa
- •55 Focal Nodular Hyperplasia II – Typical with Pathologic Correlation
- •57 Focal Nodular Hyperplasia IV – Multiple FNH Syndrome
- •58 Focal Nodular Hyperplasia V – Fatty FNH with Concurrent Fatty Adenoma
- •59 Focal Nodular Hyperplasia VI – Atypical with T2 Dark Central Scar
- •60 Hepatic Angiomyolipoma – MR-CT Comparison
- •61 Hepatic Lipoma – MR-CT-US Comparison
- •62 Hepatocellular Adenoma I – Typical with Pathologic Correlation
- •63 Hepatocellular Adenoma II – Large Exophytic with Pathologic Correlation
- •64 Hepatocellular Adenoma III – Typical Fat-Containing
- •65 Hepatocellular Adenoma IV – With Large Hemorrhage
- •77 Intrahepatic Cholangiocarcinoma – With Pathologic Correlation
- •78 Telangiectatic Hepatocellular Lesion
- •79 Focal Fatty Infiltration Mimicking Metastases
- •80 Focal Fatty Sparing Mimicking Liver Lesions
- •81 Hemosiderosis – Iron Deposition, Acquired Type
- •82 Hemochromatosis – Severe Type
- •83 Hemochromatosis with Solitary HCC
- •84 Hemochromatosis with Multiple HCC
- •85 Thalassemia with Iron Deposition
- •86 Arterioportal Shunt I – Early Enhancing Lesion in a Cirrhotic Liver
- •89 Budd-Chiari Syndrome II – Gradual Deformation of the Liver
- •90 Budd-Chiari Syndrome III – Nodules Mimicking Malignancy
- •92 Caroli’s Disease I – Intrahepatic with Segmental Changes
- •93 Caroli’s Disease II – Involvement of the Liver and Kidneys
- •95 Choledocholithiasis (Bile Duct Stones)
- •96 Gallbladder Carcinoma I – Versus Gallbladder Wall Edema
- •97 Gallbladder Carcinoma II – Hepatoid Type of Adenocarcinoma
- •98 Hilar Cholangiocarcinoma I – Typical
- •99 Hilar Cholangiocarcinoma II – Intrahepatic Mass
- •100 Hilar Cholangiocarcinoma III – Partially Extrahepatic Tumor
- •101 Hilar Cholangiocarcinoma IV – Metal Stent with Interval Growth
- •102 Hilar Cholangiocarcinoma V – Biliary Dilatation Mimicking Klatskin Tumor at CT
- •103 Primary Sclerosing Cholangitis I – Cholangitis and Segmental Atrophy
- •104 Primary Sclerosing Cholangitis II – With Intrahepatic Cholestasis
- •105 Primary Sclerosing Cholangitis III – With Intrahepatic Stones
- •106 Primary Sclerosing Cholangitis IV – With Biliary Cirrhosis
- •107 Primary Sclerosing Cholangitis V – With Intrahepatic Cholangiocarcinoma
- •108 Primary Sclerosing Cholangitis VI – With Hilar Cholangiocarcinoma
- •109 T2 Bright Liver Lesions
- •110 T1 Bright Liver Lesions
- •111 T2 Bright Central Scar
- •112 Lesions in Fatty Liver
- •113 Appendix I: MR Imaging Technique and Protocol
- •114 Appendix II: Liver Segmental and Vascular Anatomy
- •Subject Index

234 Part VI – Differential Diagnosis
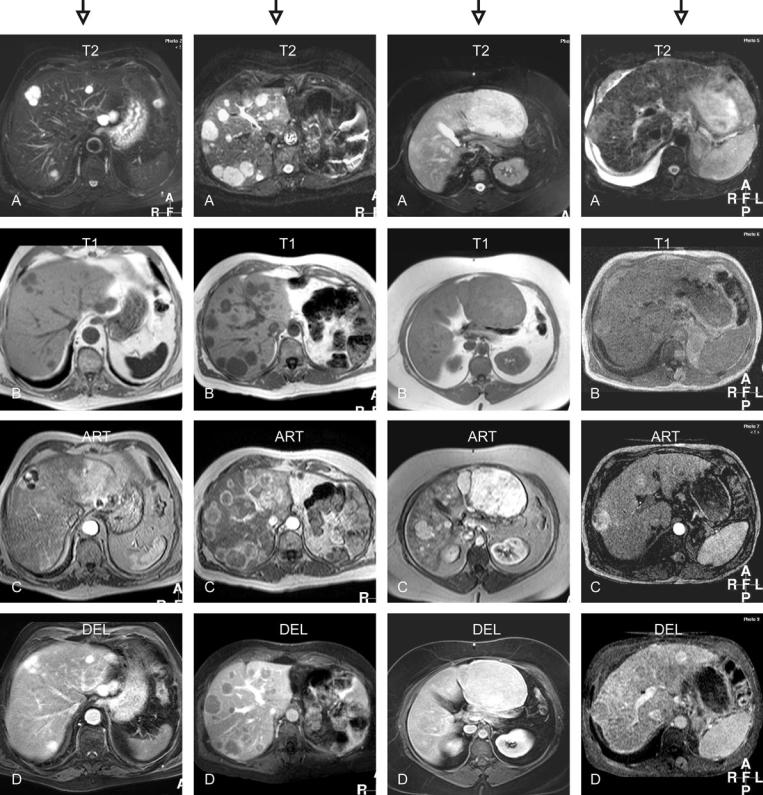
109 T2 Bright Liver Lesions
Evaluation of the T2-weighted sequences (Figs. 109.1A–109.4A):
–Lesions and the liver differ in appearance in all four examples. The first two types of lesions are however very bright, and multiple, in a non-cirrhotic liver. The third example shows a large moderately bright lesion with a non-cirrhotic liver, whereas in the final example a faintly bright nodule,
cirrhotic liver, and ascites constitute the image.
Evaluation of the T1-weighted sequences (Figs. 109.1B–109.4B):
–The first two types of lesions are similar in appearance. The third example shows isointense lesions, whereas in the final example a faintly T1 bright nodule is visible.
Evaluation of the arterial enhancement pattern (Figs. 109.1C – 109.4C):
–The lesions in the four examples show peripheral nodular, ring-shaped, almost homogeneous, and heterogeneous enhancement patterns, respectively.
Evaluation of the delayed enhancement pattern (Figs. 109.1D – 109.4D):
–The lesions in the four examples show persistent, washout without a capsule, homogeneous without a capsule, and washout with a capsular enhancement within a cirrhotic liver, respectively.
Based on the following pertinent combination of findings the lesions can be characterized as:
1.Multiple hemangiomas (T2 bright with peripheral nodular enhancement)
2.Multiple metastases (ring-shaped enhancement and washout without a capsule)
3.Multiple hepatocellular adenomas (T1 isointense, almost homogeneous enhancement without washout or capsule)
4.Multiple hepatocellular carcinomas (cirrhotic liver, slightly T2 bright lesion, heterogeneous enhancement, and washout with capsular enhancement)
|
|
|
109 T2 Bright Liver Lesions 235 |
|
|
|
|
T2 very bright lesions |
T2 very bright lesions |
T2 bright-isointense lesions |
T2 slightly bright-isointense |
T1 dark lesions |
T1 dark lesions |
T1 isointense lesions |
lesions |
Peripheral nodular |
Ring-shaped enhancement |
Homogeneous enhancement |
T1 slightly bright-isointense |
enhancement |
Washout |
Fade to isointensity |
Heterogeneous enhancement |
Persistent enhancement |
|
|
Washout with capsular |
|
|
|
enhancement |
Fig. 109.1. Multiple hemangiomas |
Fig. 109.2. Multiple metastases |
Fig. 109.3. Hepatocellular adenomas |
Fig. 109.4. Hepatocellular carcinomas |

236 Part VI – Differential Diagnosis
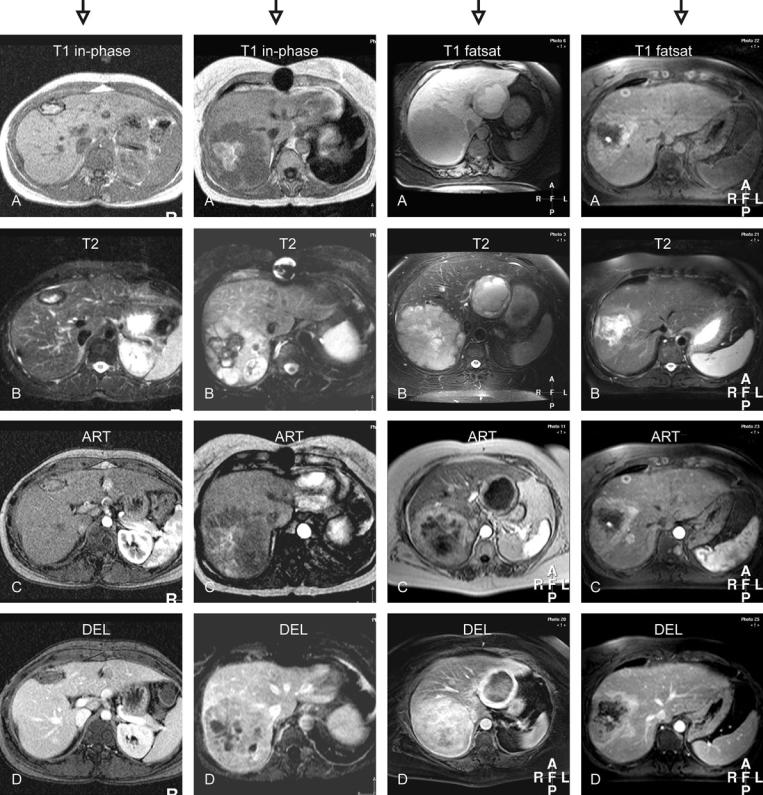
110 T1 Bright Liver Lesions
Evaluation of the T1-weighted sequence (Figs. 110.1A – 110.4A):
–All lesions have components with bright signal within a non-cirrhotic liver. In the first example, the lesion is surrounded by a dark rim. The second example shows a large
lesion with a central bright area. The third example shows a cystic lesion with bright contents in the left liver. The fourth example shows multiple, predominantly bright lesions, including one with a ring-shaped appearance.
Evaluation of the T2-weighted sequence (Figs. 110.1B – 110.4B):
–In the first example, the lesion is surrounded by a dark rim with increased thickness. The second example shows a large lesion with a central dark area. The third example shows two bright lesions with cystic and solid components. The fourth
example shows one large and small bright lesions. Evaluation of the arterial enhancement pattern (Figs. 110.1C – 110.4C):
–In the first example, the lesion does not show any enhancement (bright signal was present prior to contrast injection). The second lesion shows some heterogeneous enhancement. The third example shows lesions with a thick rim of en-
hancement. In the fourth example, the lesions show intense enhancement.
Evaluation of the delayed enhancement pattern (Figs. 110.1D – 110.4D):
–In the first example, the lesion shows lack of enhancement (mimics washout). The second lesion shows washout with some persistent heterogeneous enhancement. The third example shows lesions with a persistent rim of enhancement. In the fourth example, the lesions show washout and become less intense.
Based on the following pertinent combination of findings the lesions can be characterized as:
1.Hematoma (T1 bright due to methemoglobin with a rim of hemosiderin)
2.Hemorrhagic carcinoid metastasis (suggests metastases; non-specific findings; recommend clinical and somatostatinscintigraphy correlation)
3.Protein-producing carcinoid metastases (suggests metastases; non-specific findings; recommend clinical and somatostatinscintigraphy correlation)
4.Melanoma metastasis (T1 bright lesions in a patient with a history of uveal melanoma; intense enhancement and washout are typical for melanin-containing liver metastases)
|
|
|
110 T1 Bright Liver Lesions 237 |
|
|
|
|
T1 bright with a dark rim |
T1 very bright within a dark |
T1 bright and dark lesions |
T1 (predominantly) bright |
T2 bright with a dark rim |
lesion |
T2 mixed signal intensity |
lesions |
No enhancement |
T2 dark with a bright lesion |
Irregular ring-shaped |
T2 isointense to very bright |
No enhancement |
Heterogeneous enhancement |
enhancement |
Enhancement of the T1-bright |
|
within the lesion |
Heterogeneous and persistent |
parts |
|
Washout within the solid lesion |
enhancement |
Heterogeneous and persistent |
|
|
|
enhancement |
Fig. 110.1. Hematoma after surgery |
Fig. 110.2. Hemorrhagic carcinoid |
Fig. 110.3. Protein-producing |
Fig. 110.4. Melanoma metastases |
|
metastasis |
carcinoid metastasis |
|
