
- •Contents
- •Contributors
- •1 Introduction
- •2.1 Posterior Compartment
- •2.2 Anterior Compartment
- •2.3 Middle Compartment
- •2.4 Perineal Body
- •3 Compartments
- •3.1 Posterior Compartment
- •3.1.1 Connective Tissue Structures
- •3.1.2 Muscles
- •3.1.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2 Anterior Compartment
- •3.2.1 Connective Tissue Structures
- •3.2.2 Muscles
- •3.2.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2.4 Important Vessels, Nerves, and Lymphatics of the Anterior Compartment
- •3.3 Middle Compartment
- •3.3.1 Connective Tissue Structures
- •3.3.2 Muscles
- •3.3.3 Reinterpreted Anatomy and Clinical Relevance
- •3.3.4 Important Vessels, Nerves, and Lymphatics of the Middle Compartment
- •4 Perineal Body
- •References
- •MR and CT Techniques
- •1 Introduction
- •2.1 Introduction
- •2.2.1 Spasmolytic Medication
- •2.3.2 Diffusion-Weighted Imaging
- •2.3.3 Dynamic Contrast Enhancement
- •3 CT Technique
- •3.1 Introduction
- •3.2 Technical Disadvantages
- •3.4 Oral and Rectal Contrast
- •References
- •Uterus: Normal Findings
- •1 Introduction
- •References
- •1 Clinical Background
- •1.1 Epidemiology
- •1.2 Clinical Presentation
- •1.3 Embryology
- •1.4 Pathology
- •2 Imaging
- •2.1 Technique
- •2.2.1 Class I Anomalies: Dysgenesis
- •2.2.2 Class II Anomalies: Unicornuate Uterus
- •2.2.3 Class III Anomalies: Uterus Didelphys
- •2.2.4 Class IV Anomalies: Bicornuate Uterus
- •2.2.5 Class V Anomalies: Septate Uterus
- •2.2.6 Class VI Anomalies: Arcuate Uterus
- •2.2.7 Class VII Anomalies
- •References
- •Benign Uterine Lesions
- •1 Background
- •1.1 Uterine Leiomyomas
- •1.1.1 Epidemiology
- •1.1.2 Pathogenesis
- •1.1.3 Histopathology
- •1.1.4 Clinical Presentation
- •1.1.5 Therapy
- •1.1.5.1 Indications
- •1.1.5.2 Medical Therapy and Ablation
- •1.1.5.3 Surgical Therapy
- •1.1.5.4 Uterine Artery Embolization (UAE)
- •1.1.5.5 Magnetic Resonance-Guided Focused Ultrasound
- •2 Adenomyosis of the Uterus
- •2.1 Epidemiology
- •2.2 Pathogenesis
- •2.3 Histopathology
- •2.4 Clinical Presentation
- •2.5 Therapy
- •3 Imaging
- •3.2 Magnetic Resonance Imaging
- •3.2.1 Magnetic Resonance Imaging: Technique
- •3.2.2 MR Appearance of Uterine Leiomyomas
- •3.2.3 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.4 Histologic Subtypes and Forms of Degeneration
- •3.2.5 Differential Diagnosis
- •3.2.6 MR Appearance of Uterine Adenomyosis
- •3.2.7 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.8 Differential Diagnosis
- •3.3 Computed Tomography
- •3.3.1 CT Technique
- •3.3.2 CT Appearance of Uterine Leiomyoma and Adenomyosis
- •3.3.3 Atypical Appearances on CT and Differential Diagnosis
- •4.1 Indications
- •4.2 Technique
- •Bibliography
- •Cervical Cancer
- •1 Background
- •1.1 Epidemiology
- •1.2 Pathogenesis
- •1.3 Screening
- •1.4 HPV Vaccination
- •1.5 Clinical Presentation
- •1.6 Histopathology
- •1.7 Staging
- •1.8 Growth Patterns
- •1.9 Treatment
- •1.9.1 Treatment of Microinvasive Cervical Cancer
- •1.9.2 Treatment of Grossly Invasive Cervical Carcinoma (FIGO IB-IVA)
- •1.9.3 Treatment of Recurrent Disease
- •1.9.4 Treatment of Cervical Cancer During Pregnancy
- •1.10 Prognosis
- •2 Imaging
- •2.1 Indications
- •2.1.1 Role of CT and MRI
- •2.2 Imaging Technique
- •2.2.2 Dynamic MRI
- •2.2.3 Coil Technique
- •2.2.4 Vaginal Opacification
- •2.3 Staging
- •2.3.1 General MR Appearance
- •2.3.2 Rare Histologic Types
- •2.3.3 Tumor Size
- •2.3.4 Local Staging
- •2.3.4.1 Stage IA
- •2.3.4.2 Stage IB
- •2.3.4.3 Stage IIA
- •2.3.4.4 Stage IIB
- •2.3.4.5 Stage IIIA
- •2.3.4.6 Stage IIIB
- •2.3.4.7 Stage IVA
- •2.3.4.8 Stage IVB
- •2.3.5 Lymph Node Staging
- •2.3.6 Distant Metastases
- •2.4 Specific Diagnostic Queries
- •2.4.1 Preoperative Imaging
- •2.4.2 Imaging Before Radiotherapy
- •2.5 Follow-Up
- •2.5.1 Findings After Surgery
- •2.5.2 Findings After Chemotherapy
- •2.5.3 Findings After Radiotherapy
- •2.5.4 Recurrent Cervical Cancer
- •2.6.1 Ultrasound
- •2.7.1 Metastasis
- •2.7.2 Malignant Melanoma
- •2.7.3 Lymphoma
- •2.8 Benign Lesions of the Cervix
- •2.8.1 Nabothian Cyst
- •2.8.2 Leiomyoma
- •2.8.3 Polyps
- •2.8.4 Rare Benign Tumors
- •2.8.5 Cervicitis
- •2.8.6 Endometriosis
- •2.8.7 Ectopic Cervical Pregnancy
- •References
- •Endometrial Cancer
- •1.1 Epidemiology
- •1.2 Pathology and Risk Factors
- •1.3 Symptoms and Diagnosis
- •2 Endometrial Cancer Staging
- •2.1 MR Protocol for Staging Endometrial Carcinoma
- •2.2.1 Stage I Disease
- •2.2.2 Stage II Disease
- •2.2.3 Stage III Disease
- •2.2.4 Stage IV Disease
- •4 Therapeutic Approaches
- •4.1 Surgery
- •4.2 Adjuvant Treatment
- •4.3 Fertility-Sparing Treatment
- •5.1 Treatment of Recurrence
- •6 Prognosis
- •References
- •Uterine Sarcomas
- •1 Epidemiology
- •2 Pathology
- •2.1 Smooth Muscle Tumours
- •2.2 Endometrial Stromal Tumours
- •3 Clinical Background
- •4 Staging
- •5 Imaging
- •5.1 Leiomyosarcoma
- •5.2.3 Undifferentiated Uterine Sarcoma
- •5.3 Adenosarcoma
- •6 Prognosis and Treatment
- •References
- •1.1 Anatomical Relationships
- •1.4 Pelvic Fluid
- •2 Developmental Anomalies
- •2.1 Congenital Abnormalities
- •2.2 Ovarian Maldescent
- •3 Ovarian Transposition
- •References
- •1 Introduction
- •4 Benign Adnexal Lesions
- •4.1.1 Physiological Ovarian Cysts: Follicular and Corpus Luteum Cysts
- •4.1.1.1 Imaging Findings in Physiological Ovarian Cysts
- •4.1.1.2 Differential Diagnosis
- •4.1.2 Paraovarian Cysts
- •4.1.2.1 Imaging Findings
- •4.1.2.2 Differential Diagnosis
- •4.1.3 Peritoneal Inclusion Cysts
- •4.1.3.1 Imaging Findings
- •4.1.3.2 Differential Diagnosis
- •4.1.4 Theca Lutein Cysts
- •4.1.4.1 Imaging Findings
- •4.1.4.2 Differential Diagnosis
- •4.1.5 Polycystic Ovary Syndrome
- •4.1.5.1 Imaging Findings
- •4.1.5.2 Differential Diagnosis
- •4.2.1 Cystadenoma
- •4.2.1.1 Imaging Findings
- •4.2.1.2 Differential Diagnosis
- •4.2.2 Cystadenofibroma
- •4.2.2.1 Imaging Features
- •4.2.3 Mature Teratoma
- •4.2.3.1 Mature Cystic Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •4.2.3.2 Monodermal Teratoma
- •Imaging Findings
- •4.2.4 Benign Sex Cord-Stromal Tumors
- •4.2.4.1 Fibroma and Thecoma
- •Imaging Findings
- •4.2.4.2 Sclerosing Stromal Tumor
- •Imaging Findings
- •4.2.5 Brenner Tumors
- •4.2.5.1 Imaging Findings
- •4.2.5.2 Differential Diagnosis
- •5 Functioning Ovarian Tumors
- •References
- •1 Introduction
- •2.1 Context
- •2.2.2 Indications According to Simple Rules
- •References
- •CT and MRI in Ovarian Carcinoma
- •1 Introduction
- •2.1 Familial or Hereditary Ovarian Cancers
- •3 Screening for Ovarian Cancer
- •5 Tumor Markers
- •6 Clinical Presentation
- •7 Imaging of Ovarian Cancer
- •7.1.2 Peritoneal Carcinomatosis
- •7.1.3 Ascites
- •7.3 Staging of Ovarian Cancer
- •7.3.1 Staging by CT and MRI
- •Imaging Findings According to Tumor Stages
- •Value of Imaging
- •7.3.2 Prediction of Resectability
- •7.4 Tumor Types
- •7.4.1 Epithelial Ovarian Cancer
- •High-Grade Serous Ovarian Cancer
- •Low-Grade Serous Ovarian Cancer
- •Mucinous Epithelial Ovarian Cancer
- •Endometrioid Ovarian Carcinomas
- •Clear Cell Carcinomas
- •Imaging Findings of Epithelial Ovarian Cancers
- •Differential Diagnosis
- •Borderline Tumors
- •Imaging Findings
- •Differential Diagnosis
- •Recurrent Ovarian Cancer
- •Imaging Findings
- •Differential Diagnosis
- •Value of Imaging
- •Malignant Germ Cell Tumors
- •Dysgerminomas
- •Imaging Findings
- •Differential Diagnosis
- •Immature Teratomas
- •Imaging Findings
- •Malignant Transformation in Benign Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •Sex-Cord Stromal Tumors
- •Granulosa Cell Tumors
- •Imaging Findings
- •Sertoli-Leydig Cell Tumor
- •Imaging Findings
- •Ovarian Lymphoma
- •Imaging Findings
- •Differential Diagnosis
- •7.4.3 Ovarian Metastases
- •Imaging Findings
- •Differential Diagnosis
- •7.5 Fallopian Tube Cancer
- •7.5.1 Imaging Findings
- •Differential Diagnosis
- •References
- •Endometriosis
- •1 Introduction
- •2.1 Sonography
- •3 MR Imaging Findings
- •References
- •Vagina and Vulva
- •1 Introduction
- •3.1 CT Appearance
- •3.2 MRI Protocol
- •3.3 MRI Appearance
- •4.1 Imperforate Hymen
- •4.2 Congenital Vaginal Septa
- •4.3 Vaginal Agenesis
- •5.1 Vaginal Cysts
- •5.1.1 Gardner Duct Cyst (Mesonephric Cyst)
- •5.1.2 Bartholin Gland Cyst
- •5.2.1 Vaginal Infections
- •5.2.1.1 Vulvar Infections
- •5.2.1.2 Vulvar Thrombophlebitis
- •5.3 Vulvar Trauma
- •5.4 Vaginal Fistula
- •5.5 Post-Radiation Changes
- •5.6 Benign Tumors
- •6.1 Vaginal Malignancies
- •6.1.1 Primary Vaginal Carcinoma
- •6.1.1.1 MRI Findings
- •6.1.1.2 Lymph Node Drainage
- •6.1.1.3 Recurrence and Complications
- •6.1.2 Non-squamous Cell Carcinomas of the Vagina
- •6.1.2.1 Adenocarcinoma
- •6.1.2.2 Melanoma
- •6.1.2.3 Sarcomas
- •6.1.2.4 Lymphoma
- •6.2 Vulvar Malignancies
- •6.2.1 Vulvar Carcinoma
- •6.2.2 Melanoma
- •6.2.3 Lymphoma
- •6.2.4 Aggressive Angiomyxoma of the Vulva
- •7 Vaginal Cuff Disease
- •7.1 MRI Findings
- •8 Foreign Bodies
- •References
- •Imaging of Lymph Nodes
- •1 Background
- •3 Technique
- •3.1.1 Intravenous Unspecific Contrast Agents
- •3.1.2 Intravenous Tissue-Specific Contrast Agents
- •References
- •1 Introduction
- •2.1.1 Imaging Findings
- •2.1.2 Differential Diagnosis
- •2.1.3 Value of Imaging
- •2.2 Pelvic Inflammatory
- •2.2.1 Imaging Findings
- •2.3 Hydropyosalpinx
- •2.3.1 Imaging Findings
- •2.3.2 Differential Diagnosis
- •2.4 Tubo-ovarian Abscess
- •2.4.1 Imaging Findings
- •2.4.2 Differential Diagnosis
- •2.4.3 Value of Imaging
- •2.5 Ovarian Torsion
- •2.5.1 Imaging Findings
- •2.5.2 Differential Diagnosis
- •2.5.3 Diagnostic Value
- •2.6 Ectopic Pregnancy
- •2.6.1 Imaging Findings
- •2.6.2 Differential Diagnosis
- •2.6.3 Value of Imaging
- •3.1 Pelvic Congestion Syndrome
- •3.1.1 Imaging Findings
- •3.1.2 Differential Diagnosis
- •3.1.3 Value of Imaging
- •3.2 Ovarian Vein Thrombosis
- •3.2.1 Imaging Findings
- •3.2.2 Differential Diagnosis
- •3.2.3 Value of Imaging
- •3.3 Appendicitis
- •3.3.1 Imaging Findings
- •3.3.2 Value of Imaging
- •3.4 Diverticulitis
- •3.4.1 Imaging Findings
- •3.4.2 Differential Diagnosis
- •3.4.3 Value of Imaging
- •3.5 Epiploic Appendagitis
- •3.5.1 Imaging Findings
- •3.5.2 Differential Diagnosis
- •3.5.3 Value of Imaging
- •3.6 Crohn’s Disease
- •3.6.1 Imaging Findings
- •3.6.2 Differential Diagnosis
- •3.6.3 Value of Imaging
- •3.7 Rectus Sheath Hematoma
- •3.7.1 Imaging Findings
- •3.7.2 Differential Diagnosis
- •3.7.3 Value of Imaging
- •References
- •MRI of the Pelvic Floor
- •1 Introduction
- •2 Imaging Techniques
- •3.1 Indications
- •3.2 Patient Preparation
- •3.3 Patient Instruction
- •3.4 Patient Positioning
- •3.5 Organ Opacification
- •3.6 Sequence Protocols
- •4 MR Image Analysis
- •4.1 Bony Pelvis
- •5 Typical Findings
- •5.1 Anterior Compartment
- •5.2 Middle Compartment
- •5.3 Posterior Compartment
- •5.4 Levator Ani Muscle
- •References
- •Evaluation of Infertility
- •1 Introduction
- •2 Imaging Techniques
- •2.1 Hysterosalpingography
- •2.1.1 Cycle Considerations
- •2.1.2 Technical Considerations
- •2.1.3 Side Effects and Complications
- •2.1.5 Pathological Findings
- •2.1.6 Limitations of HSG
- •2.2.1 Cycle Considerations
- •2.2.2 Technical Considerations
- •2.2.2.1 Normal and Abnormal Anatomy
- •2.2.3 Accuracy
- •2.2.4 Side Effects and Complications
- •2.2.5 Limitations of Sono-HSG
- •2.3 Magnetic Resonance Imaging
- •2.3.1 Indications
- •2.3.2 Technical Considerations
- •2.3.3 Limitations
- •3 Ovulatory Dysfunction
- •4 Pituitary Adenoma
- •5 Polycystic Ovarian Syndrome
- •7 Uterine Disorders
- •7.1 Müllerian Duct Anomalies
- •7.1.1 Class I: Hypoplasia or Agenesis
- •7.1.2 Class II: Unicornuate
- •7.1.3 Class III: Didelphys
- •7.1.4 Class IV: Bicornuate
- •7.1.5 Class V: Septate
- •7.1.6 Class VI: Arcuate
- •7.1.7 Class VII: Diethylstilbestrol Related
- •7.2 Adenomyosis
- •7.3 Leiomyoma
- •7.4 Endometriosis
- •References
- •MR Pelvimetry
- •1 Clinical Background
- •1.3.1 Diagnosis
- •1.3.2.1 Cephalopelvic Disproportion
- •1.3.4 Inadequate Progression of Labor due to Inefficient Contraction (“the Powers”)
- •2.2 Palpation of the Pelvis
- •3 MR Pelvimetry
- •3.2 MR Imaging Protocol
- •3.3 Image Analysis
- •3.4 Reference Values for MR Pelvimetry
- •5 Indications for Pelvimetry
- •References
- •MR Imaging of the Placenta
- •2 Imaging of the Placenta
- •3 MRI Protocol
- •4 Normal Appearance
- •4.1 Placenta Variants
- •5 Placenta Adhesive Disorders
- •6 Placenta Abruption
- •7 Solid Placental Masses
- •9 Future Directions
- •References
- •Erratum to: Endometrial Cancer

474 |
G. Masselli |
|
|
overlying or near the internal cervical os (Baergren 2005). Normally, the lower placental edge should be at least 2 cm from the margin of the internal cervical os. The relationship of the placenta to the internal os changes throughout the course of pregnancy as the uterus enlarges. The diagnosis of placenta previa should not be made before 15 weeks’ gestation, and low-lying or marginal placental positioning should be revaluated later in gestation to confirm placental position before delivery.
Placenta previa can be subdivided according to the position of the placenta relative to the internal cervical os (To and Leung 1995). Although transvaginal sonography is the imaging standard for making this diagnosis, the position of the placenta is usually demonstrable with transabdominal imaging. In the appropriate clinical setting, the absence of sonographic confirmation of placenta previa does not exclude the diagnosis.
MR imaging allows accurate identification of the position of the placenta; sagittal MR sequence oriented in the plane of the cervix is used to assess the placental margin (Fig. 7).
Given widespread use of endovaginal and translabial ultrasound, this is unlikely to be a common indication for MR examination. However, transvaginal imaging should be undertaken with care in advanced pregnancies, as it can lead to premature rupture of membranes or to infection when the membranes have already ruptured. The placental edge is easily identified with MR Haste and true FISP sequences.
5\ Placenta Adhesive Disorders
Abnormal invasive placenta describes a group of conditions that produce the abnormal infiltration of placental tissue into the uterus or also into the surrounding tissues. This condition usually produces severe complications for the mother, such as massive hemorrhage, organ damage, organ failure, and even death (Bernirschke and Kaufmann 2000).
Placenta accreta, placenta increta, and placenta percreta represent a spectrum of placental adhesive disorders (PADs) and occur when a
defect of the decidua basalis allows the invasion of chorionic villi into the myometrium (Sebire and Sepulveda 2008; Oyelese and Smulian 2006).
PAD is classified on the basis of the depth of myometrial invasion: placenta accreta is the least severe of the three entities with penetration of the decidua by the chorionic villi. Placenta increta is penetration of the myometrium by the chorionic villi. Placenta percreta is the most severe of the implantation anomalies with invasion of both the myometrium and uterine serosa often with extension into neighboring organs (Bernirschke and Kaufmann 2000).
Prior cesarean section and placenta previa are the two most important risk factors for placenta adhesive disorders; these conditions occur in 5% of patients with placenta previa, in up to 10% of patients after four or more cesarean sections, and in 67% of patients who have both placenta previa and four or more cesarean sections (Oyelese and Smulian 2006).
As abnormal placentation becomes more prevalent, in large part due to the steadily rising rates of cesarean deliveries, there is a need for accurate antenatal diagnosis of this condition to prevent maternal morbidity and mortality because timing and site of delivery, availability of blood products, and recruitment of a skilled anesthesia and surgical team can be arranged in advance.
Diagnostic signs using MRI are similar to those described in US (To and Leung 1995), (Masselli et al. 2011c), (Sebire et al. 2002). Interrupted or myometrial thinning is a common sign but not specific of AIP. Previous cesarean scar is prone to produce some degree of dehiscence when the placenta is located in the lower segment. For this reason, this sign itself is not indicative of PAD, although histologically it could agree with a placenta accreta, increta, or percreta. Presence of lagoons, especially multiple, confluent, and intercommunicated, is probably the most reliable sign of PAD (US and pMRI) (Fig. 8). Tenting of bladder was described as a sign of PAD (Huppertz 2008), but this sign is not specific and surgically represents the bladder adhesion to the previous scar. Although uterine bulging was described as one of the useful signs for diagnosis,
MR Imaging of the Placenta |
475 |
|
|
a |
c |
b
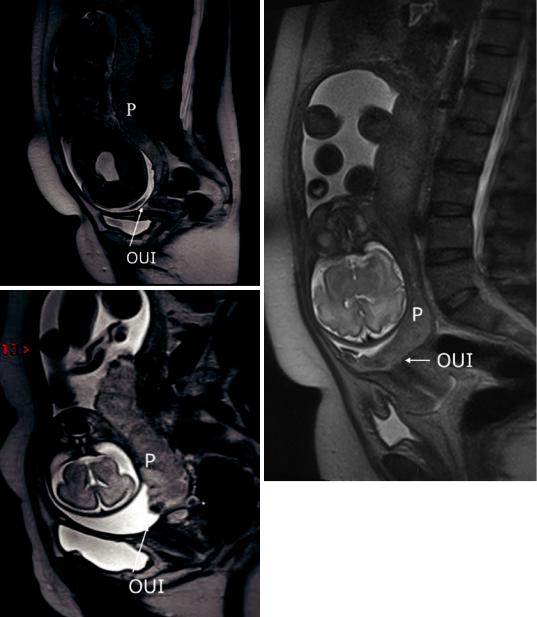
Fig. 7 Spectrum of placenta previa. Sagittal T2-weighted half-Fourier RARE MR images show a low-lying placenta (a) where the placental inferior border is within 0.5 cm of the internal uterine os (OUI), marginal placenta previa (b)
where the placental tip is located immediately at the OUI but does not cover it and central placenta previa (c), where the placenta entirely covers the OUI
this is not specific at all, as a simple uterine scar dehiscence in a placenta previa can produce it. According to some authors, absence of dark placental bands excludes a diagnosis of PAD, but this asseveration is made based on small series. Presence of lobulations is frequent in PAD (Sebire
et al. 2002), although their absence is not an exclusion criteria. For this reason, and as it happens in US analysis, prenatal diagnosis of PAD is based on a group of signs, some of them more predictive of PAD than others. Full area acquisition of MRI allows re-evaluation anytime by
476 |
G. Masselli |
|
|
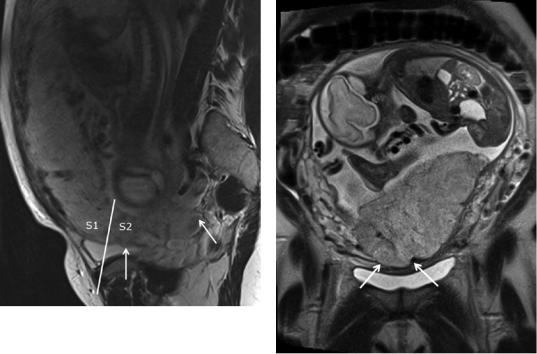
Fig. 8 A 34-year-old woman at 28 weeks’ gestation with complete placenta previa and placenta accreta in posterior lower uterine segment (S2). Sagittal T2-weighted halfFourier RARE MR image shows prominent low-signal- intensity band (arrow) on maternal side of placenta and anteriorly irregular placenta-myometrium interface with placental tissue without surrounding myometrium (small arrow). Perpendicular plane which divides the posterior bladder wall determines areas S1 and S2
Fig. 9 Placenta percreta in a 33-year-old woman with two prior cesarean deliveries. Sagittal T2-weighted halfFourier RARE image a shows a broad outward bulge (arrows) in posterior placental contour. No underlying myometrium can be seen in this region
different observers, a fact that is not usually possible for US, because image acquisition is dependent on the operator.
MR findings of more severe disease (placenta increta and percreta) include: dark placental bands on T2-weighted images, with loss of normal low signal intensity myometrium, disorganized architecture of the adjacent placenta, focal exophytic mass, and, in case of invasion involving the bladder, thinning of the uterine serosabladder interface, focal abnormal signal in the bladder wall, and extension of intermediate signal placental tissue beyond uterine margins with loss of fat planes between uterus and pelvic organs (Fig. 9) (Leyendecker et al. 2012; Masselli et al. 2008; Levine 2006; Warshak et al. 2006; Levine et al. 1997).
However, in some cases it is almost impossible to differentiate between placenta accreta and percreta using MRI, especially if there is no involvement of the adjacent structures. This is
because the myometrium becomes extremely thin as pregnancy progresses, and it becomes difficult to visualize.
The most useful findings are uterine bulging, heterogeneous signal intensity within the placenta, and dark intraplacental bands on T2-weighted images.
This appearance is common at locations where the uterus is compressed by the maternal spine, but it can be diffuse. Uterine contractions commonly cause transient focal low-signal intensity thickening of the uterine wall. Unenhanced T1-weighted images do not provide sufficient differentiation between the placenta and myometrium to be useful for assessment of abnormal placental attachment or invasion, as the placenta and the myometrium are both of homogeneous intermediate signal intensity.
Dynamic contrast-enhanced imaging of the placenta shows early intense lobular enhancement of the placental tissue that becomes

MR Imaging of the Placenta |
477 |
|
|
confluent with time and precedes enhancement of the myometrium (Tanaka et al. 2001).
Several studies have compared the accuracy and effectiveness of sonography versus MRI in the detection of placenta accreta. Warshak et al. (2006) compared pathologic diagnosis to antenatal ultrasound (including use of an endovaginal transducer) and MRI results. This study retrospectively evaluated 453 women with a diagnosis of placenta previa, low-lying placenta with prior cesarean delivery, or myomectomy, of whom 39 had abnormal placentation.
This study revealed 77% sensitivity, 96% specificity, 65% positive predictive value (PPV), and 98% negative predictive value (NPV) for ultrasound compared to 88% sensitivity, 100% specificity, 100% PPV, and 82% NPV for MRI prediction of abnormal placentation. Another study with fewer patients (n = 13) showed the sensitivities of ultrasound to be 33% and MRI to be 38%, stating that both modalities had a poor predictive value in the diagnosis of abnormal placentation (Lam et al. 2002). A multinstitutional study in 2008 by Dwyer et al. (2008) retrospectively evaluated 32 patients who were clinically at high risk for placenta accreta and had undergone both transabdominal sonography and MRI, of whom 15 had confirmed abnormal placentation at delivery. Sonography had 93% sensitivity, 71% specificity, 74% PPV, and 92% NPV, whereas MRI had 80% sensitivity, 65% specificity, 67% PPV, and 79% NPV. This study did not show a statistically significant difference in sensitivity or specificity between sonography and MRI, concluding that both modalities may be complementary – if findings are inconclusive with one, the other modality may be useful for clarifying the diagnosis.
Some authors have suggested that MR imaging is most clearly indicated when there is a posterior placenta or in patients with previous myomectomy (Levine et al. 1997).
We agree that MRI should be reserved primarily when ultrasound findings are equivocal for abnormal placentation or to assess portions of the uterus inaccessible to sonographic examination in patients with risk factors. Even when ultrasound findings are convincing for a diagnosis of
placenta accreta, MRI can be beneficial in planning subsequent management by specifically delineating the extent of an ultrasound diagnosed placenta percreta (Masselli et al. 2008; Palacios Jaraquemada and Bruno 2005).
According to the previous topographic characterization of Palacios et al. (Palacios Jaraquemada and Bruno 2000), these sagittal images obtained through MRI allow the division of anterior placenta invasion into two sectors, delimited by a plane perpendicular to the center of the so-called upper bladder axis. The uterine sectors bordering the upper and lower posterior bladder walls were called S1 and S2, respectively. S1 PADs are generally of easy access and quick hemostasis, whereas S2 PADs – being irrigated by deeply located vessels – often result in a significantly increased surgical complexity and massive hemorrhage.
MRI has another potential benefit compared with US in that it provides a larger field of view, thereby granting an easier evaluation of the topography of placenta invasion and classification of S1 PAD and S2 PAD (Fig. 8).
MRI can detect the presence of new vascularization associated to PAD that indicates a different approach or surgical treatment. Although these differences may be seen by US, it can be difficult to differentiate peripheral placental circulation (lacunae blood flow) from newly formed vessels, especially when the bladder wall is very thin.
This is not a minor issue, because in recent years, many cases of PAD have happened after the first cesarean, so a decision whether or not to perform a hysterectomy must be carefully taken.
6\ Placenta Abruption
Antepartum hemorrhage (vaginal bleeding between 20 weeks’ gestation and delivery) remains an important cause of maternal and fetal morbidity and mortality. Placenta previa and placental abruption account for more than one-half of cases of antepartum hemorrhage and are increasing in prevalence as the rate of cesarean section increases (Sakornbut et al. 2007; Sinha and Kuruba 2008).

478 |
G. Masselli |
|
|
Placental abruption represents premature separation of the placenta from the uterine wall. Although rare (<1% of pregnancies), third-tri- mester abruption is associated with an increased risk of preterm delivery and fetal death (Oyelese and Ananth 2006).
The diagnosis of placental abruption is clinical and is characterized as the premature detachment of the placenta from its implantation site. The condition may be sudden and painful or clinically silent. It may manifest as a placental hematoma as discussed above, without other symptoms such as pain or vaginal bleeding. Placental abruption affects approximately 1% of births and is the leading cause of vaginal bleeding in the final trimester and may manifest as a placental hematoma (Elsasser et al. 2010).
There are three types of placental hematoma, including retroplacental, subchorionic, and subamniotic. Retroplacental hematomas are defined as being posterior to the placenta, representing 43% of hematomas. Subchorionic hematomas are between the chorion and the endometrium, representing approximately 57% of hematomas. Subamniotic hematomas are rare and are located between the amnion and the chorion (Oyelese and Ananth 2006; Elsasser et al. 2010).
US is frequently performed to confirm the presence of abruption and assess the extent of subchorionic or retroplacental hematoma (Nyberg et al. 1987). The presence of blood in large enough volumes to be visible sonographically indicates retained hemorrhage that may remain symptomatic.
However in up to 50% of cases of abruption US is negative for different reasons (Levine and Pedrosa 2005; Sakornbut et al. 2007; Nyberg et al. 1987): (1) Acute hemorrhage echo texture is very similar to that of the adjacent placenta and is therefore very difficult to detect. (2) The sign of
an abnormally thick and heterogeneous placenta is rare, being present only in large acute clots. (3) Many subacute clots result falsely negative since blood dissects out from beneath the placenta and drains trough the cervix.
Diffusion-weighted imaging is an excellent sequence for detecting intrauterine hemorrhagic lesions.
Blood breakdown products cause susceptibility effects and can be accurately demonstrated with the diffusion-weighted sequence (Bonel et al. 2010; Oyelese and Smulian 2006). In our study (Masselli et al. 2008), the diffusionand T1-weighted sequences were more accurate than the T2-weighted half-Fourier RARE and true FISP sequences in the detection of placental abruption; this finding is in agreement with previously reported evidence (Linduska et al. 2009; Verswijvel et al. 2002). T2-weighted half-Fourier RARE and true FISP sequences have high sensitivity in the detection of acute ischemic lesions and good diagnostic accuracy in the detection of placental hematomas, probably owing to the coexisting condition of acute or subacute bleeding and chronic ischemia in abruption (Linduska et al. 2009). Subchorionic or retroplacental hemorrhage typically demonstrates low T2 and intermediate to high T1 signal. Diffusion-weighted imaging (DWI) has been recently demonstrated to be very useful in the detection of retroplacental hematoma (Fig. 10).
T1and T2-weighted sequences are complementary, and both are required for complete tissue characterization. By considering the signal intensity changes on T1-, T2-, and diffusionweighted images, with special reference to the paramagnetic effects of methemoglobin, it is possible to estimate the age of the bleeding and intrauterine hematomas can be accurately classified as follows: hyperacute (first few hours, intracellular
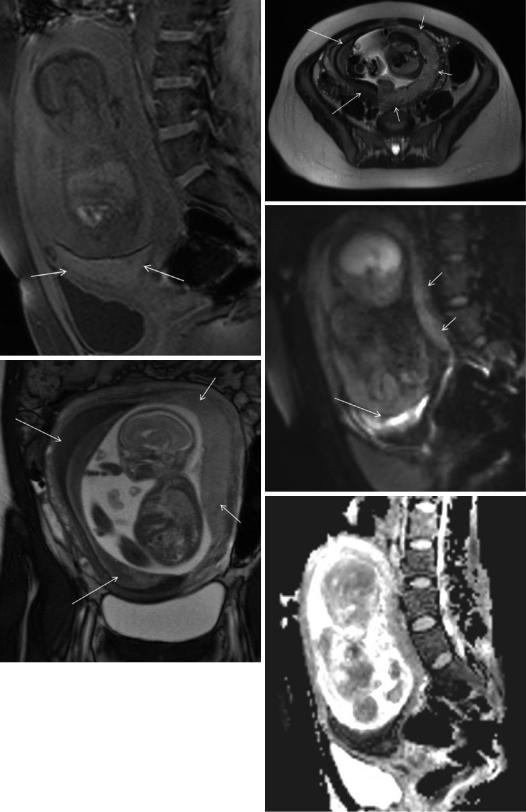
Fig.10 Subchorionic hemorrhage in a 25-year-old woman at 27 weeks’ gestation. Transvaginal gray-scale US scan were suggestive of the presence of placenta previa, whereas MR images correctly depicted the presence of subchorionic hematoma. Sagittal T1-weighted gradient-echo image (a) shows the hyperintense subchorionic hematoma located above the internal os. The intrauterine clot shows heterogeneous signal due to the presence of hypo and hyperintense
areas to placenta on the axial T2-weighted half-Fourier RARE (b) and on coronal true FISP (c) images. (d) Sagittal diffusion-weighted MR image (b value, 800 s/mm2) and ADC map (e) show the hematoma (arrow) has hypoand hyperintense areas. The signal intensity characteristics are suggestive of the presence of hyperacute and subacute bleeding in the hematoma. The placenta (short arrow) is not previa and has normal signal intensity
MR Imaging of the Placenta |
479 |
|
|
a |
b |
d
c
e
