
- •In accordance with the modern rule of transfusiology, it is necessary to transfuse only one-group (according to the ab0 system) and single-rhesus blood.
- •Determination of blood group and Rh factor Determination of blood groups by standard isohemagglutinating sera
- •Intravenous blood transfusion
- •Infiltration anesthesia according to a.V. Vishnevsky combines the positive qualities of infiltration and conduction anesthesia.
- •Intravenous anesthesia
- •Intraosseous anesthesia
- •Intravenous anesthesia
- •Inhalation anesthesia
- •Vomiting, regurgitation
Intravenous anesthesia
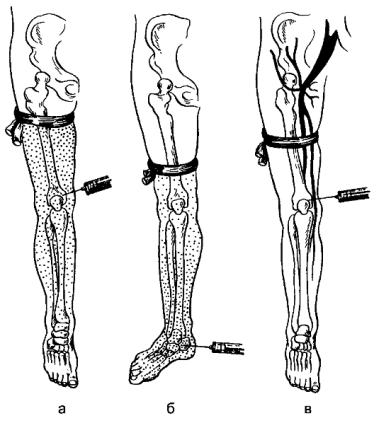
Intravenous anesthesia is used in operations on the extremities (surgical debridement of wounds, reduction of dislocation, reposition of bone fragments, arthrotomy). In modern conditions, this type of pain relief is used extremely rarely. The method is based on local (due to diffusion in the tissue of the anesthetic drug injected into
vein) the effect of an anesthetic substance on the nerve endings of the limb segment, isolated by a tourniquet from the general blood flow (Fig. 17).
By puncture or venesection, the anesthetic is injected into the superficial veins of the forearm or elbow bend, into the large or small saphenous vein of the leg. For the outflow of venous blood, the limbs are raised for 1-2 minutes and an elastic bandage or tourniquet is applied proximal to the intended site of operation to stop arterial blood flow. For operations on the foot, lower leg, knee joint, a tourniquet is applied on the lower third of the thigh, during operations on the hand, forearm, elbow joint - on the lower third of the shoulder. Instead of an elastic bandage, you can use a cuff from a blood pressure (BP) machine, into which air is pumped until arterial blood flow stops. For operations on the upper limbs, 150-200 ml are used, on the lower ones - 200-250 ml of a 0.25% solution of procaine. At the end of the operation, the tourniquet or cuff is removed slowly, Figure: 17. Intravenous anesthesia.
70
Intraosseous anesthesia
Intraosseous anesthesia is a type of intravenous local anesthesia. They are rarely used. Anesthetic substance, injected intraosseously, enters the venous system of the limb, from where it diffuses into the tissues (Fig. 18). Intraosseous anesthesia is used for operations on the extremities. The limb is isolated from the general blood flow by applying an elastic bandage or tonometer cuff. The anesthetic is injected on the upper limb into the condyles of the shoulder, olecranon, hand bones, on the lower limb, into the condyles of the thigh, ankle, and heel bone. For operations on the upper limb, a tourniquet is applied to the shoulder, during operations on the foot - on the lower third of the lower leg, during operations on the lower leg - on the lower third of the thigh, and during operations on the thigh - on its upper third.Figure: 18. Intraosseous anesthesia. The spread of the anesthetic when injected into the femoral condyle (a), into the heel bone (b). With incorrectly superimposed
the tourniquet leaves the anesthetic substance in the general bloodstream (c).
Above the puncture site, the skin is infiltrated with a 0.25% solution of procaine, and then the deep-lying tissues and periosteum are anesthetized with the same needle. A needle with a mandrel for a bone puncture is passed through the skin, tissue, and rotationally penetrate through the cortical plate into the cancellous bone. For operations on the foot and lower leg, use 100-150 ml, on the thigh - 150-200 ml, on the upper limb - 100-150 ml of a 0.25% solution of procaine. After removing the tourniquet, the toxic-resorptive effect of the anesthetic drug (weakness, dizziness, arterial hypotension, nausea, vomiting) may occur.
71
To prevent the toxic effect of procaine (which happens if it quickly enters the general bloodstream after the end of the operation), the patient is injected subcutaneously with 2 ml of caffeine solution before removing the tourniquet, then the tourniquet is slowly removed.
Effect potentiation
The effectiveness of local anesthesia is increased when combined with antipsychotic drugs (droperidol) and narcotic analgesics (fentanyl). With combined anesthesia, including local anesthesia and NLA, the effect of local anesthesia increases with the simultaneous beneficial effect of neuroleptics on the psychoemotional state of the patient.
NLA and central analgesia are used to potentiate the effects of various types of local anesthesia (infiltration, conduction, spinal, epidural), which makes it possible to reduce the dose (and thus the toxic effect) of both local anesthetic and narcotic substances.
Complications
Complications of local anesthesia are associated with allergic reactions to the administration of an anesthetic drug, an overdose of the latter or epinephrine. Individual hypersensitivity to local anesthetic substances manifests itself in the form of skin rash, itching, Quincke's edema, laryngo, or bronchospasm. To stop allergic reactions, antihistamines, glucocorticoids, and antispasmodics are used.
An overdose of the anesthetic substance during local anesthesia occurs when a large amount of the drug enters the bloodstream. Overdose symptoms are anxiety of the patient, skin flushing, increased heart rate, increased blood pressure, convulsions. In severe cases, with increasing intoxication, coma, collapse, respiratory and cardiac arrest develop. Mild manifestations of an overdose can be eliminated by the introduction of barbiturates, narcotics, inhalation of oxygen. In severe cases, cardiac and vasodilating agents are used, transfusions of anti-shock blood substitutes, mechanical ventilation are performed, and in case of cardiac arrest - heart massage.
Prevention of complications of local anesthesia consists in finding out anamnestic data on the tolerability of drugs and compliance with the methodology for its implementation.
Spinal anesthesia
Spinal anesthesia refers to conduction and is carried out by introducing an anesthetic drug into the subarachnoid space of the spinal cord. It is used for operations on organs located below the diaphragm: stomach, intestines, liver and bile ducts, spleen, pelvic organs, as well as on the lower extremities. The anesthetic substance blocks the posterior (sensitive) roots of the spinal cord, which leads to a loss of pain, tactile, temperature sensitivity, and the anterior (motor) roots with the development of motor paralysis (muscle relaxation). Preganglionic sympathetic fibers are also blocked, passing through the anterior roots, which causes changes in vascular innervation, leading to the expansion of arterioles in the innervation zone. During the blockade
72
sympathetic fibers involved in the formation of celiac fibers, the expansion of the vessels of the abdominal cavity, pelvis, lower extremities can lead to the deposition of blood in them and a drop in blood pressure.
For spinal anesthesia, special needles with a well-fitted mandrel, syringes graduated to tenths of a milliliter, with well-fitted plungers are needed. Apply 2% lidocaine solution, 0.5% bupivacaine solution, 5% procaine solution, 0.75% bupivacaine solution in dextrose.
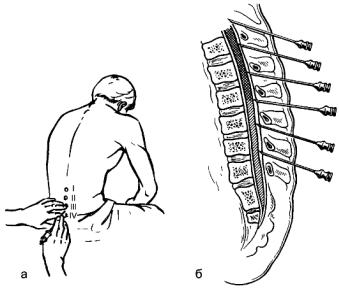
The patient is seated across the table, the legs are placed on a stool, the knees should be raised, the back is bent as much as possible. The nurse stands in front of the patient, bends his shoulders down and helps to maintain the accepted position. When puncture is performed in the supine position, the patient is placed on his side, the back is at the edge of the table, the knees are pulled to the stomach, the chin is pressed to the chest, the back is bent as much as possible. The assistant stands in front of the patient and, holding the patient with one hand by the neck and the other by the pelvis, fixes him in this position, trying to bend the spine where the puncture is performed. Figure: 19. Technique of spinal puncture: a - the choice of the puncture site in the sitting position of the patient; b - direction of advancement of the needle depending on the slope of the spinous
process.
The puncture is usually performed between the spinous processes L III and L IV or L II and L III . The spinous process L IV serves as a reference point, which is located on the line connecting the posterior superior spine of the iliac bones (Fig. 19). The operating field is treated with diethyl ether and alcohol. The skin at the injection site is infiltrated with a 0.25% solution of procaine. The needle is inserted in the midline between the spinous processes with a slight (5-10 °) downward slope. When the needle passes through the interspinous, supraspinous and yellow ligaments, resistance is felt, which disappears when the ligaments are punctured. Another slight resistance is noted with a puncture of the dura mater; after overcoming it, the advance of the needle is stopped, the mandrel is removed, the needle is advanced by rotational movements by 2-3 mm, piercing the inner layer of the dura mater. The appearance of a clear cerebrospinal fluid indicates a correctly performed puncture. In the absence or insufficient flow of fluid, the needle is rotated around the axis and advanced 1-2 mm forward. If fluid does not appear from the needle or blood is shown, the needle is removed and the puncture is repeated between the other spinous processes.
73
After making sure that the puncture was carried out correctly, 2-3 ml of cerebrospinal fluid is drawn into the syringe, mixed with an anesthetic solution and injected into
spinal canal. The patient is immediately placed on the operating table, lowering the head end of the table by 15? (with the introduction of lidocaine or 0.5% bupivacaine solution) or lifting it (with the introduction of procaine or 0.75% bupivacaine solution). Giving the patient the appropriate position allows you to prevent the spread of the anesthetic solution to the higher parts of the spinal cord and medulla oblongata, which depends on the density of the anesthetic substance. The lidocaine solution and 0.5% bupivacaine solution have a lower density than the cerebrospinal fluid, and therefore will spread upward, while the procaine solution and 0.75% bupivacaine solution are of higher density and will spread downward.
Contraindications for spinal anesthesia are traumatic shock, severe intoxication with peritonitis, accompanied by arterial hypotension, inflammatory skin diseases in the back, spinal deformities.
A serious complication of spinal anesthesia is a decrease in blood pressure due to blockade of sympathetic fibers. More often, the complication occurs with anesthesia at the level of the lower thoracic and upper lumbar segments of the spinal cord. With anesthesia at the level of the lower lumbar segments of the spinal cord, arterial hypotension usually does not occur. To prevent hypotension, vasoconstrictor drugs are administered before the operation, and when a complication occurs, they are combined with the transfusion of anti-shock blood substitutes. To centralize blood circulation, the lower limbs are raised and bandaged.
With the spread of the anesthetic drug up the subarachnoid space, it is possible to turn off the nerve fibers that innervate the intercostal muscles, which can lead to respiratory failure or respiratory arrest. In case of respiratory failure, oxygen therapy is used, in case of respiratory arrest - artificial ventilation of the lungs.
In the late period, after spinal anesthesia, headache, motor paresis, and purulent meningitis may appear as a result of aseptic disorders. Due to the complications of spinal anesthesia, its use is limited. Currently, epidural anesthesia is used more widely.
Epidural anesthesia
Epidural anesthesia is a type of nerve block anesthesia. The analgesic effect is achieved by blocking the roots of the spinal cord with an anesthetic drug injected into the epidural space between the dura mater and the periosteum of the vertebrae (Fig. 20). This type of anesthesia has all the positive qualities of spinal pain relief and is devoid of its disadvantages.
The technique of puncture of the epidural space is similar to that of the subdural space during spinal anesthesia. The puncture can be performed at any level of the spinal column, depending on the nature of the operation. It should be remembered about the possibility of puncture of the dura mater and the ingress of anesthetic into the subarachnoid space, which is fraught with serious complications. Puncture is performed with a needle put on a syringe with isotonic sodium chloride solution. The advancement of the needle is accompanied by resistance against pressure on the piston. how
74
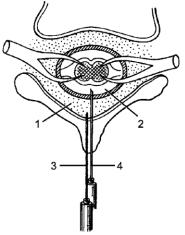
only the needle penetrates through the ligaments into the epidural space, the resistance when pressing the plunger disappears, and the solution is easily injected, the failure of the needle is felt. Another sign of a correctly performed puncture is the absence of a needle leaking from the pavilion of cerebrospinal fluid; when a water pressure gauge is connected to the needle, the determined pressure should be negative. The anesthetic can be administered through a needle or a catheter passed through the lumen of the needle and left on for a long time. To prolong anesthesia, drugs can be delivered fractionally through the catheter. Figure: 20. Puncture of the epidural and subdural space: 1 - epidural space; 2 - subdural space; 3 - a needle in the epidural space; 4
- a needle in the subdural space.
For epidural anesthesia, 2% lidocaine solution, 0.5% bupivacaine solution, 0.75% ropivacaine solution are used. To enhance the analgesic effect during traumatic operations, narcotic analgesics (morphine and fentanyl) are injected into the epidural space. In the postoperative period, long-term epidural blockade is used as an effective method of pain relief, allowing to reduce the dose of narcotic analgesics.
Epidural anesthesia is used for traumatological and orthopedic operations on the lower extremities, operations on the abdominal cavity and pelvic organs. This type of anesthesia is indicated for elderly and senile people, patients with severe diseases of the cardiovascular, respiratory system, metabolic disorders (obesity, diabetes mellitus).
Complications are rare. Possible arterial hypotension and breathing disorders, nausea, vomiting, seizures. In 5% of cases, anesthesia does not occur, which is associated with the presence of bridges in the epidural space, which limit the spread of the anesthetic solution.
Stages of anesthesia
Narcotic drugs cause characteristic changes in all organs and systems. During the period of saturation of the body with a narcotic drug, a certain pattern (staging) is noted in the change in consciousness, respiration, and blood circulation. In this regard, stages are distinguished that characterize the depth of anesthesia. The stages are especially clearly manifested with ether anesthesia.
There are four stages: I - analgesia, II - arousal, III - surgical stage, which is divided into 4 levels, IV - awakening.
76
Analgesia stage (I)
The patient is conscious, but inhibited, dozing, answers questions in monosyllables. There is no superficial pain sensitivity, but tactile and heat sensitivity is preserved. During this period, it is possible to perform short-term interventions (opening phlegmons, abscesses, diagnostic studies). The stage is short, lasts 3-4 minutes.
Arousal stage (II)
At this stage, inhibition of the centers of the cerebral cortex occurs, but the subcortical centers are in a state of excitement: there is no consciousness, motor and speech excitement is expressed. Patients scream, trying to get up from the operating table. The skin is hyperemic, the pulse is frequent, the blood pressure is increased. The pupils are wide, but they react to light, there is lacrimation. Often there is a cough, increased bronchial secretion, vomiting is possible. Surgical manipulations against the background of arousal cannot be performed. During this period, it is necessary to continue saturating the body with a narcotic drug to deepen the anesthesia. The duration of the stage depends on the patient's condition, the experience of the anesthesiologist. Arousal usually lasts 7-15 minutes.
Surgical stage (III) With the onset of this stage of anesthesia, the patient calms down, breathing becomes even, the pulse rate and blood pressure are approaching the initial level. During this period, it is possible to carry out surgical interventions. Depending on the depth of anesthesia, four levels of stage III anesthesia are distinguished.
First level (III 1 ). The patient is calm, breathing is even, blood pressure and pulse reach their initial values. The pupils begin to narrow, the reaction to light is preserved. Smooth movement of the eyeballs, their eccentric arrangement are noted. The corneal and pharyngeal-laryngeal reflexes are preserved. The muscle tone is preserved, therefore, it is difficult to carry out abdominal operations.
Second level (Ш 2 ). The movement of the eyeballs stops, they are located in a central position. The pupils begin to dilate gradually, their response to light weakens. The corneal and pharyngeal-laryngeal reflexes weaken and by the end of level III 2 disappear. Breathing is calm, even. BP and pulse are normal. A decrease in muscle tone begins, which makes it possible to carry out abdominal operations. Usually anesthesia is performed at level III 1 -III 2 .
Third level (Ш 3 ). Deep anesthesia. The pupils are dilated, react only to a strong light stimulus, the corneal reflex is absent. During this period, complete relaxation of the skeletal muscles, including the intercostal muscles, occurs. Breathing becomes shallow, diaphragmatic. As a result of relaxation of the muscles of the lower jaw, the latter can sag, in such cases, the root of the tongue sinks and closes the entrance to the larynx, which leads to respiratory arrest. To prevent this complication, it is necessary to bring the patient's lower jaw forward and maintain it in this position. Pulse at this level is speeded up, small filling. BP goes down. You need to know that carrying out anesthesia at this level is dangerous for the patient's life.
77
The fourth level (Ш 4 ). The maximum dilation of the pupils without their reaction to light, the cornea is dull, dry. Breathing is shallow, carried out due to the movements of the diaphragm due to the onset of paralysis of the intercostal muscles. Pulse threadlike, frequent, low blood pressure or not at all. Deepening the anesthesia to level III 4 is dangerous for the patient's life, as breathing and blood circulation may stop.
Awakening stage (IV)
As soon as the supply of narcotic substances stops, the concentration of the anesthetic in the blood decreases, the patient goes through all the stages of anesthesia in the reverse order, and awakening occurs.
Preparing the patient for anesthesia
The anesthesiologist is directly involved in preparing the patient for anesthesia and surgery. The patient is examined before the operation, while not only paying attention to the underlying disease for which the operation is to be performed, but also finding out in detail the presence of concomitant pathology. If the patient is operated on in a planned manner, then, if necessary, treatment of concomitant diseases, sanitation of the oral cavity is carried out. The doctor finds out and assesses the patient's mental state, allergological history, clarifies whether the patient has undergone surgery and anesthesia in the past, pays attention to the shape of the face, chest, neck structure, and the severity of subcutaneous fat. All this is necessary in order to choose the right method of pain relief and a narcotic drug.
An important rule of preparing a patient for anesthesia is cleansing the gastrointestinal tract (gastric lavage, cleansing enemas).
To suppress the psychoemotional reaction and suppress the functions of the vagus nerve, before the operation, the patient is given a special drug preparation - premedication.The purpose of premedication is to reduce the incidence of intra- and postoperative complications due to the use of medications. Sleeping pills are given at night, tranquilizers (for example, diazepam) are prescribed to patients with a labile nervous system 1 day before the operation. 40 minutes before the operation, narcotic analgesics are injected intramuscularly or subcutaneously: 1 ml of 1-2% solution of trimeperidine or 2 ml of fentanyl. To suppress the functions of the vagus nerve and reduce salivation, 0.5 ml of 0.1% atropine solution is injected. In patients with a burdened allergic history, antihistamines are included in premedication. Immediately before the operation, the oral cavity is examined and removable dentures are removed.
In case of emergency interventions, the stomach is washed before the operation, and premedication is carried out on the operating table, drugs are administered intravenously.
