
- •In accordance with the modern rule of transfusiology, it is necessary to transfuse only one-group (according to the ab0 system) and single-rhesus blood.
- •Determination of blood group and Rh factor Determination of blood groups by standard isohemagglutinating sera
- •Intravenous blood transfusion
- •Infiltration anesthesia according to a.V. Vishnevsky combines the positive qualities of infiltration and conduction anesthesia.
- •Intravenous anesthesia
- •Intraosseous anesthesia
- •Intravenous anesthesia
- •Inhalation anesthesia
- •Vomiting, regurgitation
ANTIGENIC BLOOD SYSTEMS AND THEIR ROLE IN TRANSFUSIOLOGY
To date, about 500 antigens of blood cells and blood plasma are known, of which more than 250 are erythrocyte antigens. Antigens are linked into antigenic systems. There are more than 40 of them, and half of them are erythrocyte systems. Cell systems play a role in transfusiology. Plasma systems are of no practical importance.
137
Human erythrocytes contain such systems as AB0, Rh-factor, Kell, Kidd, Lutheran, etc. In transfusiology, the AB0 and Rh-factor systems play the main role. The AB0 system includes agglutinogens (antigens) A and B and agglutinins (antibodies) α and β. Agglutinogens are found in erythrocytes, agglutinins - in blood serum. The simultaneous presence in the blood of the same components (A and α, B and β) is impossible, since their meeting leads to the isohemagglutination reaction.
The ratio of agglutinogens A and B and agglutinins determines the four blood groups.
Group I - I (0): there is no agglutinogen in erythrocytes, but there are α and β agglutinins.
Group II - P (A): erythrocytes contain agglutinogen A, serum - agglutinin β.
Group III - III (H): in erythrocytes - agglutinogen B, in serum - agglutinin α.
Group IV - IV (AB): erythrocytes contain agglutinogens A and B, serum does not contain agglutinins.
The varieties of agglutinogen A - A 1 and A 2 are known . Accordingly, group II (A) has subgroups II (A 1 ), II (A 2 ), and group IV (AB) - IV (A 1 B) and IV (A 2 B).
The Rh factor system is represented by six antigens (D, d, C, c, E, e). 85% of people have Rh antigen D in their erythrocytes, and these people are considered Rh positive, 15% of people are Rh negative - their red blood cells do not have this antigen. Antigen D has the most pronounced antigenic properties. If the Rh antigen enters the blood of an Rh-negative person (as can be the case with a transfusion of Rh-positive blood or during pregnancy of a Rh-negative woman with an Rh-positive fetus), antibodies to the Rh factor are produced in his body. When the Rh antigen re-enters the blood of an already sensitized person (blood transfusion, repeated pregnancy), an immune conflict develops. In the recipient, this is manifested by a blood transfusion reaction, up to shock,
In human leukocytes, the cell membrane contains the same systems as in erythrocytes, as well as specific antigenic complexes. In total, about 70 antigens were found, united in a number of systems (HLA, NA-NB, etc.), which are not of particular importance in transfusion practice. The HLA system of leukocytes is important in organ and tissue transplantation. When selecting donors, the compatibility of the donor and the recipient according to the AB0 system, the Rh factor and the HLAgenic complex must be taken into account.
In human platelets contain the same antigens in erythrocytes and leukocytes (HLA), localized in the cell membrane. Platelet antigenic systems Zw, Co, P1 are also known, but in the practice of transfusiology and transplantology they have no clinical significance.
More than 200 antigens were found on the surface of blood plasma protein molecules, which are combined into 10 antigenic complexes (Ym, Hp, Yc, Tf, etc.). For
138
+
In clinical practice, the Ym system associated with immunoglobulins (Ig) is important. Plasma antigens are not considered in practical transfusiology.
Human blood contains constant innate antibodies (α and β agglutinins), all other antibodies are unstable - they can be acquired, formed in the body in response to the intake of various antigens (for example, Rh factor) - these are isoimmune antibodies. Antigens are cold antibodies, their specific action (agglutination) is manifested at room temperature; isoimmune antibodies (for example, anti-rhesus) - heat, they show their effect at body temperature.
Antigen-antibody interaction goes through two stages (phases). In the first phase, antibodies are fixed on the blood cell and cause adhesion of shaped elements (agglutination). The addition of the plasma compliment to the antigen-antibody leads to the formation of an antigen-antibody-compliment complex, which lyses the cell membrane (erythrocytes), hemolysis occurs.
Blood antigens during transfusion can be the reason for its immunological incompatibility. The antigens of the AB0 system and the Rh factor play the main role in this. If in the blood of the recipient to whom the blood is transfused, the antigen of the same name in erythrocytes and antibodies in the plasma are found, then the agglutination of erythrocytes occurs. The same is possible with antigens and antibodies of the same name (A and α, B and β), as well as Rh antigen and anti-rhesus antibodies. For such a reaction, there must be a sufficient amount (titer) of antibodies in the blood serum. Ottenberg's rule is based on this principle ,which states that the erythrocytes of the transfused donor blood are agglutinated, since the agglutinins of the latter are diluted with the recipient's blood and their concentration does not reach the level at which they can agglutinate the erythrocytes of the recipient. According to this rule, all recipients can be transfused with blood of group 0 (I), since it does not contain agglutinogens. Recipients of AB (IV) group can be transfused with blood of other groups, since it does not contain agglutinins (universal recipient). However, when a large amount of blood is transfused (in particular, with massive blood loss), the agglutinins of the transfused othergroup blood entering the body can agglutinate the host's erythrocytes. In this regard, the Ottenberg rule is applicable when transfusing up to 500 ml of donated blood.
The first transfusion of Rh-positive blood to a Rh-negative recipient, not previously sensitized, may proceed without incompatibility, but will lead to the formation of antibodies. Transfusion to a Rh negative woman sensitized during pregnancy with a Rh positive fetus will result in Rh incompatibility. When transfusing Rh-negative blood into re-positive recipients, the production of antibodies to weak antigens of the Rh-factor system contained in the transfused blood is not excluded.
Individuals with Rh-negative blood are simultaneously positive for Rh antigen, this should be taken into account when transfusing Rh-negative blood into a positive recipient, since it is possible to cause sensitization of the recipient and create a risk of post-transfusion complications if the recipient is Rh-negative. In this regard, for transfusion, blood should be used strictly of the same name in terms of the Rh factor, taking into account the test for Rh compatibility of the blood of the donor and recipient.
Plasma transfusion is carried out taking into account the group (AB0) blood belonging. In extreme situations, AB (IV) plasma transfusion is possible to all recipients,
plasma A (II) and B (III) - recipients of group 0 (I). Plasma 0 (I) is transfused into recipients of the same blood group.
In accordance with the modern rule of transfusiology, it is necessary to transfuse only one-group (according to the ab0 system) and single-rhesus blood.
In extreme situations, you can transfuse the blood of a universal donor, use the Ottenberg rule, or transfuse Rh-positive blood in a volume of no more than 500 ml. But this is absolutely unacceptable in children.
Determination of blood group and Rh factor Determination of blood groups by standard isohemagglutinating sera
To determine the blood group, the following equipment is required: two sets of standard hemagglutinating sera of groups I (0), II (A), III (B) of groups of two different series and one ampoule of serum IV (AB) (a dry clean pipette is dipped into each ampoule with serum ), a bottle with isotonic sodium chloride solution with a pipette, a clean, dry plate, glass slides, sterile lance-shaped needles for piercing the skin of a finger, sterile gauze balls, alcohol. The determination is carried out in a room with good lighting, at a temperature of 15 to 25 ° C.
Each ampoule of standard serum must have a passport-label indicating the blood group, batch number, titer, expiration date, place of manufacture. It is prohibited to use an ampoule without a label. Standard sera for determining the blood group according to the AB0 system are produced with a specific color marking: I (0) - colorless, II (A) - blue, III (B) - red, IV (AB) - yellow. The marking is available on the label in the form of colored stripes: there are no stripes on the label of serum I (0), serum II (A) - two blue stripes, serum III (B) - three red stripes and serum IV (AB) - four yellow stripes colors. Serums are stored at a temperature of 4-10 ° C. The serum should be light and transparent, the ampoule should be preserved. The presence of flakes, sediment, turbidity are signs of unsuitable whey. The serum titer must be at least 1:32, activity - high: the first signs of agglutination should appear no later than 30 s. Serums with an expired shelf life are not suitable for use.
The plate is divided into four squares with a colored pencil and in a clockwise direction squares I (0), II (A), III (B) are designated. A large drop of serum of two series I (0), II (A), III (B) groups is applied to the corresponding square of the plate with a pipette. The pad of the finger is treated with alcohol and the skin is punctured with a spear-needle. The first drop of blood is removed with a gauze ball, subsequent drops in different corners of the glass slide are sequentially introduced into the serum drops and stirred thoroughly. A drop of the introduced blood should be 5-10 times less than a drop of serum. Then, by shaking the plate, thoroughly mix the blood and serum. The preliminary results are evaluated after 3 minutes, after which a drop of isotonic sodium chloride solution is added, mixed again by rocking the plate and after 5 minutes the final assessment of the agglutination reaction is carried out (Fig. 37, see col. incl.).
With a positive isohemagglutination reaction, flakes and grains from adhered erythrocytes do not diverge when an isotonic sodium chloride solution is added and
140
stirring. In case of a negative reaction, the drops of whey on the plate are transparent, uniformly pink in color, and do not contain flakes or grains. The following four combinations of agglutination reactions with standard sera of I (0), II (A), III (B) groups are possible.
1. All three sera in both series do not agglutinate. Test blood - I (0) group.
2. The isohemagglutination reaction is negative with serum II (A) of the group of both series
and positive with sera of I (0) and III (B) groups. Test blood - II (A) group.
3. The isohemagglutination reaction is negative with the serum of the III (B) group in both series and positive with the serum of the I (0) and III (A) groups. Test blood - III (B) group.
4. Sera of I (0), II (A), III (B) groups give a positive reaction in both series. The blood belongs to the IV (AB) group. But before giving such a conclusion, it is necessary to carry out an isohemagglutination reaction with standard serum of group IV (AB) by the same method. A negative isohemagglutination reaction makes it possible to finally assign the blood under study to the IV (AB) group.
The identification of other combinations indicates an incorrect determination of the patient's blood group.
Information about the patient's blood group is entered into the medical history, a corresponding note is made on the title page, signed by the doctor who conducted the study, indicating the date of the study.
Errors in determining the group affiliation of blood are possible in situations where, in the actual presence of agglutination, it is not detected, or, conversely, agglutination is detected in its actual absence. Undetected agglutination may be due to: 1) weak activity of standard serum or low agglutinability of erythrocytes; 2) an excess amount of test blood added to the standard serum; 3) a delayed agglutination reaction at a high ambient temperature.
To avoid mistakes, it is necessary to use active, with a sufficiently high titer of serum at a ratio of the volume of the studied blood and standard serum 1: 5, 1:10. The study is carried out at a temperature not higher than 25 ° C, the results should be evaluated no earlier than 5 minutes from the start of the study.
The detection of agglutination in its actual absence may be due to the drying of a drop of serum and the formation of "coin" columns of erythrocytes or the manifestation of cold agglutination, if the study is carried out at an ambient temperature below 15 ° C. Adding a drop of isotonic sodium chloride solution to the blood and serum under study and conducting research at temperatures above 15 ° C, these errors can be avoided. Errors in determining the blood group are always associated with a violation of the research method, therefore, careful observance of all research rules is necessary.
In all doubtful cases, it is necessary to re-study the group affiliation with standard sera of other series or using standard erythrocytes.
141
Determination of the blood group according to the AB0 system using anti-A and anti-B monoclonal antibodies (anti-A and anti-B tsoliclones)
Anti-A and anti-B tsoliklones are used to determine the human blood group according to the AB0 system instead of standard isohemagglutinating sera by detecting antigens A and B in erythrocytes with standard antibodies contained in tsoliclones.
Monoclonal antibodies anti-A and anti-B are produced by two different hybridomas resulting from the fusion of muscle antibody-producing B lymphocytes with murine myeloma cells. The named tsoliclones are a diluted ascitic fluid of hybridoma carrier mice, containing IgM against antigens A and B. The tsoliclones produce a faster and more pronounced agglutination reaction than standard AB0 sera.
Determine the blood group at a temperature of 15 to 25 ° C. On a porcelain plate or a marked plate, one large drop of anti-A and anti-B tsoliclones is applied, a drop of test blood 10 times smaller is applied next to it and mixed with separate sticks or corners of glass slides. Swing the plate slightly and observe the reaction for 2.5 minutes. The reaction usually occurs in the first 3-5 s and is manifested by the formation of small red aggregates, and then flakes. The following variants of the agglutination reaction are possible.
1. Agglutination is absent with anti-A and anti-B tsoliclones, the blood does not contain agglutinogens A and B - the tested blood of group I (0) (Fig. 38, see color incl.).
2. Agglutination is observed with anti-A tsoliclones , erythrocytes of the test blood contain agglutinogen A - the test blood of group II (A).
3. Agglutination is observed with anti-B tsoliclone , erythrocytes of the test blood contain agglutinogen B - the test blood of group III (B).
4. Agglutination is observed with anti-A and anti-B tsoliclones, erythrocytes contain agglutinogens A and B - the blood of group IV (AB) under study (Table 2).
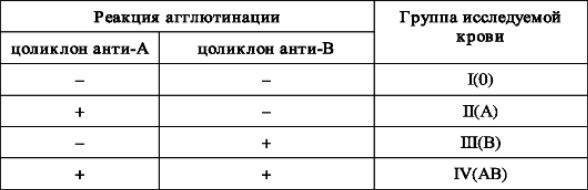
Table 2.
Agglutination reaction of the studied erythrocytes with anti-A and anti-B tsoliclones In the presence of an agglutination reaction with anti-A and anti-B tsoliclones [blood group IV (AB)] to exclude nonspecific agglutination, an additional control study is performed with isotonic sodium chloride solution. A large drop (0.1 ml) of isotonic solution is mixed with a small (0.01 ml) drop of the investigated
142
blood. The absence of agglutination confirms that the blood under study belongs to the IV (AB) group. In the presence of agglutination, the blood group is determined using washed standard erythrocytes.
Anti-A and anti-B cyclones are available in liquid form in ampoules or vials, the liquid is colored in red (anti-A) and blue (anti-B) colors. Store in a refrigerator at 2-8 ° C. Shelf life is 2 years.
Determination of the blood group of the AB0 system by standard washed erythrocytes with a known group affiliation
3-4 ml of blood is taken from the patient's vein into a test tube and centrifuged. On a plate divided into sectors, a drop of serum is applied according to the inscriptions, to which a drop of standard erythrocytes is added 5 times less than a drop of the test serum, the drops are mixed with the angle of the glass slide, the plate is shaken for 3 minutes, then isotonic sodium chloride solution is added drop by drop, continue to mix by rocking and evaluate the results after 5 minutes. There are four options for the agglutination reaction.
1. Agglutination is absent with erythrocytes of the I (0) group and is determined with erythrocytes of the II (A) and III (B) groups - the studied blood of the I (0) group.
2. Agglutination is absent with erythrocytes of groups I (0) and II (A) and is determined with erythrocytes of III (B) group - the blood of group II (A) being examined.
3. Agglutination is absent with erythrocytes of I (0) and III (B) groups and is determined with erythrocytes of II (A) group - the blood of group III (B) being examined.
4. Agglutination is absent with erythrocytes of I (0), II (A), III (B) groups - the studied blood of IV (AB) group.
Determination of the Rh factor
A blood test for Rh-belonging by the conglutination method is carried out using special anti-Rh sera in laboratory conditions. The group affiliation is preliminarily determined (according to the AB0 system).
Equipment: two different series of standard anti-Rh sera corresponding to the blood group to be determined, or group-compatible standard washed single-group Rh-positive and Rh-negative erythrocytes, Petri dish, water bath, serum pipettes, microscope slides or glass rods.
Three large drops of anti-Rh serum of one series are applied in a row to a Petri dish, and three drops of serum of another series are applied in parallel, to obtain two horizontal rows of serums. Then, a small drop of the test blood is introduced into the first vertical row of sera of both series (the ratio of serum and blood is 10: 1 or 5: 1), in the middle row - by the same drop of standard Rh-positive erythrocytes (activity control), in the third row - Rh negative standard erythrocytes (specificity control). Serum and erythrocytes are thoroughly mixed with a separate glass rod or corner of a glass slide for each drop, the cups are closed with a lid and placed in a water bath at a temperature of 46-48 ° C. After 10 minutes
143
take the result into account by viewing the cup in transmitted light. A drop with standard Rh-positive erythrocytes should have agglutination, with Rh-negative ones, it is absent. If agglutination is determined in the drops of both series of sera with the studied erythrocytes, the blood is Rh-positive, if it is absent, the blood is Rh-negative.
It should be remembered that it is strictly forbidden to add an isotonic sodium chloride solution to a drop of serum, as is customary in determining the blood group according to the AB0 system using standard sera, as this may disrupt the agglutination reaction.
Errors in determining the Rh factor may be due to a decrease in the activity of standard anti-Rh sera, a violation of the serum / blood ratio, non-compliance with the temperature regime during the study, a decrease in the exposure time (less than 10 min), the addition of isotonic sodium chloride solution, the absence of control samples for activity, and serum specificity, group discrepancies between standard sera and test and standard erythrocytes.
For the express method for determining the Rh factor, a special reagent is used - serum of anti-Rh IV (AB) group, diluted with 20-30% human albumin solution or 30-33% dextran solution [cf. pier weight 50 000-70 000], used as a substance that promotes the aggregation of erythrocytes at room temperature.
A drop of standard serum anti-Rh IV (AB) group is applied to a glass slide or Petri dish and a drop of Rh negative serum IV (AB) group that does not contain antibodies is applied in parallel. A drop of the test blood is added to them 2-3 times smaller in volume, mixed with the angle of a glass slide, a glass rod or by rocking for 3-4 minutes, after which 1 drop of isotonic sodium chloride solution is added and after 5 minutes the reaction is taken into account. In the presence of agglutination of erythrocytes with anti-Rh serum and its absence with control serum, the blood is Rh-positive, in the absence of agglutination with both sera, it is Rh-negative. In the event of agglutination with both sera, the reaction should be considered doubtful. For emergency transfusion, use only Rh negative blood,
BLOOD TRANSFUSION METHODS
The currently used transfusion following methods: 1) preserved blood transfusion (indirect transfusion); 2) exchange transfusions; 3) autohemotransfusion.
In clinical practice, indirect transfusions are mainly used using canned blood and its components.
 Figure: 39. Direct
blood transfusion using syringes.
Figure: 39. Direct
blood transfusion using syringes.
Direct blood transfusion
Direct blood transfusion from a donor to a recipient is rarely used. The indications for it are: 1) long-term, not amenable to hemostatic therapy of bleeding in patients with hemophilia; 2) disorders of the blood coagulation system (acute fibrinolysis, thrombocytopenia, afibrinogenemia) after massive blood transfusion and in diseases of the blood system; 3) traumatic shock of the III degree in combination with blood loss of more than 25-50% of the BCC and the lack of effect from the transfusion of canned blood.
The donor for direct transfusion is examined at the blood transfusion station. Immediately before the transfusion, the group and Rh belonging of the donor and the recipient are determined, tests for group compatibility and the Rh factor are carried out, a biological test is carried out at the beginning of the transfusion. Transfusion is carried out using a syringe or apparatus. Use 20-40 syringes with a capacity of 20 ml, needles for venipuncture with rubber tubes worn on their pavilions, sterile gauze balls, sterile clamps such as Billroth's clamps. The operation is performed by a doctor and a nurse. The nurse draws blood from the donor's vein into a syringe, squeezes the rubber tube with a clamp and passes the syringe to the doctor, who injects blood into the patient's vein (Fig. 39). At this time, the sister draws blood into a new syringe. The work is carried out synchronously. Before transfusion, 2 ml of a 4% sodium citrate solution are drawn into the first 3 syringes to prevent blood coagulation, and blood is injected from these syringes slowly (one syringe for 2 minutes). In this way, a biological test is performed.
Special devices are also used for blood transfusion.
Exchange transfusion
Exchange transfusion is a partial or complete removal of blood from the bloodstream of the recipient and its simultaneous replacement with the same
145
+
the amount of blood infused. Indications for exchange transfusion are various poisoning, hemolytic disease of the newborn, blood transfusion shock, acute renal failure. With exchange transfusion, poisons and toxins are removed together with the exfused blood. Blood infusion is performed with a replacement purpose.
For exchange transfusion, freshly preserved or preserved blood of short shelf life is used. Blood is poured into any superficial vein, exfusion is carried out from large veins or arteries to prevent blood clotting during a long procedure. Removal of blood and infusion of donor blood is carried out simultaneously at an average rate of 1000 ml for 15-20 minutes. For full blood replacement, 10-15 liters of donor blood is required. BASIC METHODS OF BLOOD TRANSFUSION
