
- •Preface
- •1. Principles of Surgical Physiology
- •2. Essential Topics in General Surgery
- •3. Medical Risk Factors in Surgical Patients
- •4. Principles of Thoracic Surgery
- •5. Chest Wall, Lung, and Mediastinum
- •6. Heart
- •7. Peripheral Arterial Disease
- •8. Venous Disease, Pulmonary Embolism, and Lymphatic System
- •9. Common Life-threatening Disorders
- •10. Esophagus
- •11. Stomach and Duodenum
- •12. Small Intestine
- •13. Colon, Rectum, and Anus
- •14. Liver, Portal Hypertension, and Biliary Tract
- •15. Pancreas
- •16. Thyroid, Adrenal, Parathyroid, and Thymus Glands
- •18. Benign Lesions
- •19. Malignant Lesions of the Head and Neck
- •20. Parotid Gland
- •21. Trauma and Burns
- •22. Spleen
- •23. Breast
- •24. Organ Transplantation
- •25. Urologic Surgery
- •26. Plastic Surgery and Skin and Soft Tissue Surgery
- •27. Neurosurgery
- •28. Orthopedics
- •29. Pediatric Surgery
- •30. Laparoscopic Surgery
Chapter 18
Benign Lesions
Joseph R. Spiegel
Robert T. Sataloff
David A. Zwillenberg
I Introduction
Familiarity with the benign conditions reviewed in this chapter is essential to the physician who must distinguish life -threatening illnesses from those of little consequence, choose appropriate therapy, and avoid injudicious surgery.
A Overview
The most common neck mass is a reactive node, and these masses are most often secondary to bacterial or viral infections of the ear, nose, paranasal sinuses, teeth, tonsils, or skin and soft tissues of the head and neck.
Most neck masses in children are benign.
In adults, neck masses are more likely to be malignant.
The “rule of sevens” is a useful guide:
A mass that has been present for 7 days is inflammatory.
One present for 7 months is malignant.
One present for 7 years is congenital.
B Workup for acquired lesions
(see IV)
The history should be detailed, especially regarding:
Family history of malignancy
Past malignancy in the patient
Risk factors associated with malignancy, such as:
Smoking
Alcohol consumption
Exposure to radiation, certain fumes, sawdust, or other potential carcinogens
Recent relevant illnesses, such as:
Upper respiratory infection, sinusitis, or tonsillitis
Otitis or conjunctivitis
Dental problems
Physical examination should include careful inspection and palpation of the scalp, eyes, ears, nose, mouth (including the teeth and tonsils), hypopharynx, and nasopharynx for signs of infection, ulceration, or unsuspected abnormalities.
Laboratory tests may include:
Complete blood count and differential
Chest radiograph
Tuberculin test for tuberculosis
A heterophil titer (monospot test) for mononucleosis
Thyroid function tests or thyroid scan
Serologic tests for syphilis
Viral titers, especially for Epstein -Barr virus, which is associated with nasopharyngeal carcinoma and Burkitt's lymphoma
Radiologic studies may include soft tissue radiographs of the neck, xeroradiograms, a barium swallow, and a complete gastrointestinal series or scanning procedures such as computed
P.360
tomography (CT), magnetic resonance imaging (MRI), bone scan, or other radioisotope scans.

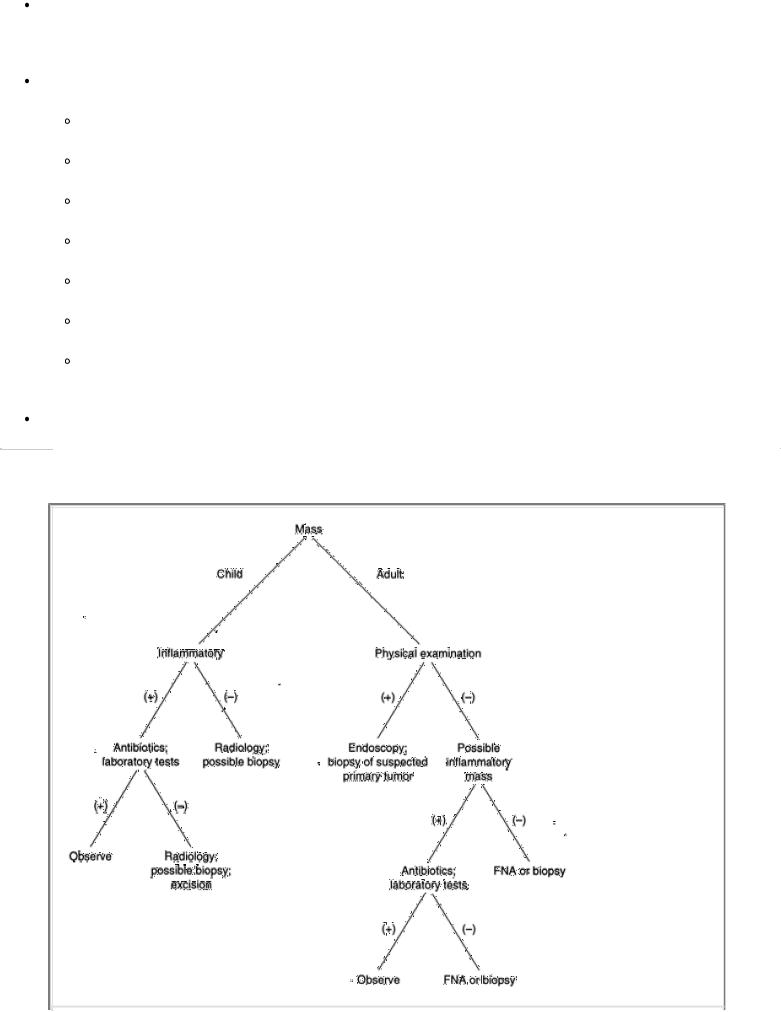
FIGURE 18-1 Algorithm for evaluation and treatment of a neck mass. FNA, fine-needle aspiration; PE, physical examination.
Endoscopy is indicated to search for the tumor if a primary neoplasm is suspected. Endoscopic biopsy and radiologic studies should precede any incision in the neck (see Chapter 19, II B )
Treatment depends on the findings during the workup (Fig. 18 -1).
Antibiotics should be administered if a bacterial infection is suspected.
Antituberculous drugs may be needed.
Consultation with a specialist in another field may be helpful.
A dental consultation may be useful if the teeth seem to be the source of a problem.
If dandruff, scabies, or another dermatologic condition is noted, a dermatology consultation is indicated.
If a mass does not shrink significantly or disappear within a reasonable time (usually 6 weeks), then surgical treatment or biopsy may be indicated.
If cervical adenopathy persists, then:
The presence of enlarged or cryptic tonsils is believed by many to be an indication for tonsillectomy.
Equivocal or abnormal dental findings are an indication for dental treatment.
If a source of infection is not found, then persistent cervical adenopathy is an indication for excisional biopsy after a complete evaluation for malignancy.
A neck mass biopsy is the last step in a proper workup. Fine -needle aspiration can be used to diagnose carcinoma, but it is usually inadequate to define lymphoma.
P.361
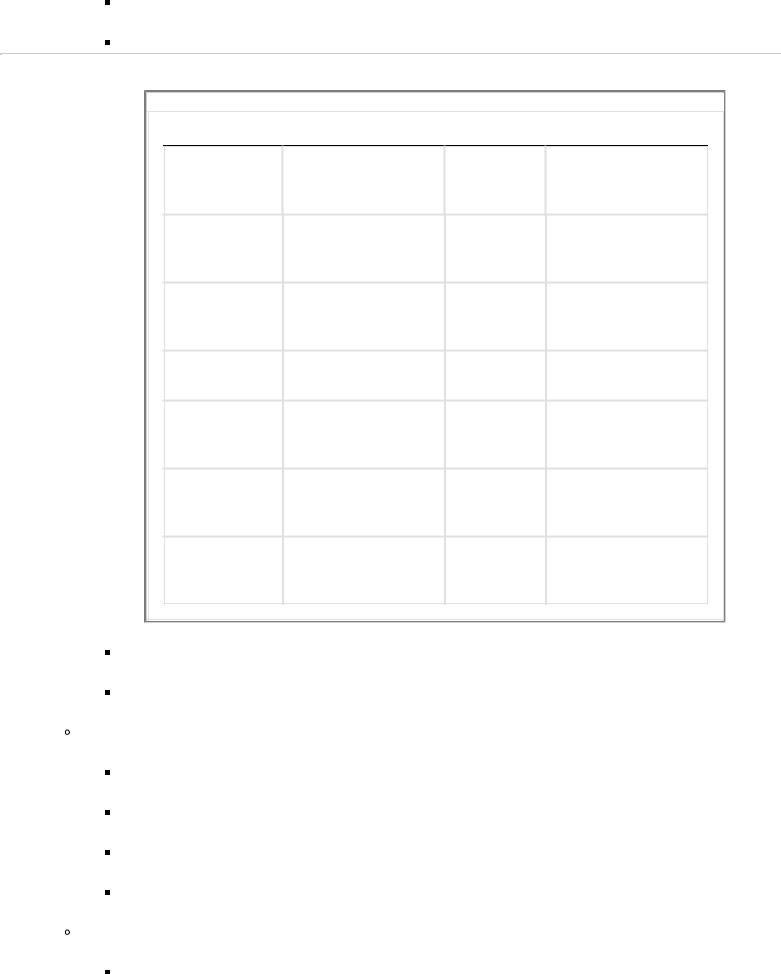
TABLE 18-1 Neck Abscesses
Signs and Symptoms
Pain
Swelling
Dysphagia
Dyspnea
Leukocytosis
Fever
Air in soft-tissue radiograph
Treatment
Airway protection
Incision and drainage
Antibiotics
II Neck Abscesses
A Overview
A patient presenting with fever and a painful, fluctuant neck mass most probably has an abscess (Table 18 -1).
The source of infection should be identified, and drainage should be carried out.
Owing to the danger to the carotid artery, airway, and cranial nerves, deep neck abscesses should be treated only by those knowledgeable in the standard techniques and anatomy of the area. They should be treated on an emergency basis.
B Types of abscesses
Bezold's abscesses are neck abscesses that arise from infection in the middle ear or mastoid.
Ludwig's angina is an abscess that occupies the sublingual space.
It generally arises from a dental source.
It can cause death from airway obstruction and, therefore, frequently requires tracheostomy.
Parapharyngeal space abscesses arise from the posterior teeth or tonsils and can affect the carotid sheath structures and multiple cranial nerves. They can cause mediastinitis and carotid “blowout” (i.e., erosion of the artery wall leading to massive hemorrhage).
Retropharyngeal abscesses arise from infected retropharyngeal nodes or extension from other spaces. They can lead to airway obstruction or mediastinitis.
Peritonsillar abscesses (quinsy) arise as a complication of acute tonsillitis.
They present with ipsilateral palatal edema, contralateral deviation of the uvula, “hot potato” voice, trismus, and dysphagia. The patient may have only a low -grade fever or be afebrile.
They are the most common abscesses in the parapharyngeal space.
III Congenital Masses (Table 18-2)
A Parenchymal cysts
Thymic cysts
Embryology. The thymus arises from the third pharyngeal pouch and migrates caudally and medially to descend into the superior mediastinum.
During this descent, an attachment may remain in the neck.
Thymic tissues may present in the neck as separate nodules of mature thymus or may occur in association with ciliated or columnar epithelial remnants of the pharyngeal outpouching.
Thymic cysts may occur anywhere on a line from the mandibular angle to the suprasternal notch.
Characteristics
Approximately 95% of thymic cysts are unilateral, and 90% of thymic ectopias are cystic.
They are generally found in children, and there is a male predominance.
P.362
TABLE 18-2 Congenital Neck Masses
Type |
Location |
Examination |
Treatment |
Thymic cysts |
Anterior triangle |
Firm, |
Surgical excision |
|
|
nontender |
|
Parathyroid |
Paratracheal |
Firm, |
Surgical excision |
cysts |
|
nontender |
|
Thyroglossal |
Midline |
Firm, |
Surgical excision |
cysts |
|
nontender |
|
Teratoma |
Anywhere |
Firm |
Surgical excision |
Hemangioma |
Anywhere |
Diffuse |
Observation; laser |
|
|
|
treatment |
Cystic |
Posterior triangle |
Diffuse |
Partial excision |
hygroma |
|
|
|
Branchial |
Preauricular |
Firm, |
Surgical excision |
cleft cyst |
anterior triangle |
nontender |
|
They may be unilocular or multilocular.
Loculated cysts generally contain amber to brown fluid, which may be clear or turbid.
Complications
Cysts are often asymptomatic but may be painful if they are infected or if they grow suddenly. Midline cysts may cause dysphagia.
Both benign and malignant hyperplasia have been reported in these cysts.
Myasthenia gravis is not found in association with cervical thymic cysts.
Differential diagnosis
Branchial cleft cysts seldom extend inferiorly to the clavicle and often present with signs of acute inflammation.
Cystic hygromas are lateral, spongy, and more diffuse. They are seen generally in infants.
Treatment. Surgery is the treatment of choice.
Parathyroid cysts
Characteristics
These unusual cysts generally present in adults from 30–50 years of age as a solitary mass at either inferior pole of the thyroid gland.
Tracheal deviation is usual and causes a variable degree of respiratory obstruction.
Hoarseness may occur because of pressure on the recurrent laryngeal nerve.
Treatment consists of surgical excision.
B Lesions of thyroid origin
Overview. The thyroid gland originates at the foramen cecum and descends centrally to the thyroid and cricoid cartilages.
The thyroglossal duct may pass in front of, through, or behind the hyoid bone. It is generally obliterated but may persist.
Elements of thyroidal primordium may remain at any site in its passage.
These elements may give rise not only to cysts and fistulas but also to accessory thyroid tissue and neoplasms.
Most cystic remnants occur in the midline around the hyoid bone.
Solid tumors of thyroglossal duct origin occur almost exclusively within the tongue and above the hyoid bone.
Thyroid rests
Characteristics
Thyroid rests may be lingual or may occur in the neck.
Endotracheal ectopias may occur.
Palpation of the normal position of the thyroid often reveals easily palpable tracheal rings in patients with these rests.
Treatment is dictated by the degree of obstruction present and by the presence of other thyroid tissue.
A thyroid scan should be performed before the removal of lesions suspected of being thyroid rests to ensure that there is functional thyroid tissue in the usual location.
Between 70% and 80% of patients have no other functional thyroid.
P.363
Thyroglossal cysts, sinuses, and fistulas
Anatomy
These occur in the midline, unless previous surgery has produced distortion.
Approximately 20% are suprahyoid, 15% occur at the hyoid, and 65% are infrahyoid.
Characteristics
Fistulas are almost always the result of infection with spontaneous or surgical drainage. Fistulas can drain internally, externally, or both (complete fistulas).
Thyroglossal duct cysts present by age 10 in 50% of cases.
There is no sexual predominance, but there is a racial predominance; the cysts occur most often in whites.
Cysts usually measure 2–4 cm in diameter and gradually increase in size, although the size may fluctuate.
They rise and fall with the larynx during swallowing.
Treatment is total surgical excision (Sistrunk procedure), including the:
Cyst and sinus to the base of the tongue
Whole fistula if one is present
Middle third of the hyoid bone
C
Cutaneous branchiogenic cysts are rare, asymptomatic nodules that are noted soon after birth and gradually increase in size.
Anatomy. They are located in the suprasternal notch.
Treatment is by local surgical excision.
D
Teratomas are growths that consist of multiple tissues that are foreign to the part of the body in which they arise.
Types
Epidermoid cysts, the most common type, are lined by squamous epithelium and have no adnexa.
Dermoid cysts are epithelium-lined cavities containing skin appendages (e.g., hair, glandular tissue, and follicles).
Teratoid cysts are lined with simple stratified squamous epithelium or respiratory epithelium and contain cheesy keratinous material. They are rare in the head and neck.
Cervical teratomas are most commonly present at birth. Appearance after the age of 1 year is rare.
Characteristics
The lesions are usually 5–12 cm in their long axis and are semicystic, although they may be solid. They are usually unilateral.
Infants with cervical dermoids usually have stridor, apnea, or cyanosis because of tracheal compression or deviation. Dysphagia may also be present.
Some infants are asymptomatic at birth but become symptomatic within weeks or months.
Associated anomalies. There is an increased incidence of maternal hydramnios, but affected infants show no increase in associated anomalies.
Treatment. Early excision in infants is mandatory.
Malignant teratomas of the neck are rare and occur exclusively in adults. The prognosis is very poor.
Nasal dermoids are often apparent shortly after birth.
Anatomy. The nasal dorsum is the most common site, but they may occur in the tip of the nose or the columella.
Characteristics
They show a male predominance of 2:1.
They must be differentiated from encephaloceles and gliomas.
Treatment. Early removal is important. Recurrences secondary to incomplete removal are common.
P.364
E Vascular tumors
(see Chapter 26, II B 3 a)
Hemangiomas are the most common tumors of the head and neck in children. Girls are more often affected than boys, and the lesions are usually solitary.
Types
Capillary hemangiomas, such as nevus flammeus (port-wine stain) and strawberry nevus are characteristically found in the dermis.
They rarely appear in adults.
They have an early period of evolution, after which they often regress. They may develop suddenly and grow quite large.
Cavernous hemangiomas are more permanent. Spontaneous regression is more likely for hemangiomas present at birth than in those appearing later.
Arteriovenous hemangiomas occur almost exclusively in adults and have a predilection for the lips and perioral skin.
Invasive hemangiomas occur in the deep subcutaneous tissues, deep fascial layers, and muscles.
These hemangiomas present as neck masses, predominantly in children.
They tend to recur long after excision but do not metastasize.
The masseter and trapezius are the muscles most commonly involved in the head and neck.
Intramuscular hemangiomas most commonly present in young adults as palpable, mobile, noncompressible masses.
They are generally without thrills, pulsations, or bruits.
Pain secondary to compression of other structures is usually present.
Subglottic hemangiomas are usually capillary in type. Owing to their location, they often present at birth (or soon thereafter) with stridor and usually with cutaneous involvement as well.
Treatment
Congenital cutaneous hemangiomas are generally not treated initially.
When patients reach school age, cosmetically deforming lesions may be excised.
Steroids may be used to slow a rapid growth phase if necessary.
Tunable dye and copper vapor lasers have shown promise in the treatment of cutaneous lesions.
Subglottic lesions may require tracheotomy, steroids, and, in some cases, laser excision. Surgery may be needed for extensive lesions.
Radiation therapy has been used to suppress tumor growth. However, radiation alone will not effect a cure, and its use in these lesions is controversial.
Cystic hygromas are found predominantly in the neck and are usually noted at birth or soon thereafter.
Anatomy. They are more common in the posterior triangle.
They may reach up into the cheek or parotid region and down into the mediastinum or axilla.
Large masses extend past the sternocleidomastoid muscle into the anterior compartment and may cross the midline.
They may involve the floor of the mouth and the base of the tongue.
Symptoms and signs may include:
Difficulty in nursing
Facial or neck distortion
Respiratory distress
Brachial plexus compression with pain or hyperesthesia
A sudden increase in size secondary to spontaneous hemorrhage, which can be fatal
Characteristics
There is no predilection for either sex or for either side of the body.
The hygromas can be progressive, static, or regressive.
Small lesions are unilocular and firm.
Large tumors are loculated, shiftable, and compressible.
P.365
The hygromas generally transilluminate.
The cyst walls are usually tense, and because the loculi tend to communicate, rupture of one locule can cause all of them to partially collapse.
Treatment. Surgery is the mainstay of treatment.
Recurrences are common because the cysts insinuate themselves into adjacent structures, so resection is often incomplete.
The greater the lymphangiomatous component of a hygroma, the more likely it is to recur.
Oral and perioral lymphangiomas are relatively common lesions that are usually found at birth or soon thereafter. They behave very much like cystic hygromas.
F Branchial cleft anomalies
Embryology
In the fourth week of gestation, five ridges appear on the ventrolateral surface of the embryonic head, with a groove between each. These ridges and grooves form the branchial arches and clefts, respectively.
The pharyngeal pouches develop internally at the same level as the external grooves.
Types
A sinus , or incomplete fistula , has either an internal or an external opening.

A complete fistula has both an internal and an external opening.
A cyst has neither an internal nor an external opening.
Combinations of any of the preceding types can occur.
Anatomy. Branchial cleft anomalies are generally located along the anterior border of the sternocleidomastoid muscle or deep to it. They can occur anywhere between the external auditory canal and the clavicle.
First branchial cleft anomalies are always superior to the hyoid bone.
If a fistula is present, it courses superiorly to end near the external auditory canal.
The cyst and tract may lie in the parotid gland, with a variable relationship to the facial nerve.
Second cleft anomalies are the most common type.
An external opening, when present, is about two thirds of the way down the sternocleidomastoid anteriorly.
The fistula, if present, ascends with the carotid sheath and crosses over the hypoglossal and glossopharyngeal nerves and between the external and internal carotid arteries to end at the tonsillar fossa.
Third cleft anomalies are rare.
The external opening occurs in the same position as in a second cleft fistula.
The tract ascends along the carotid sheath posteriorly to the internal carotid artery, over the hypoglossal nerve, under the glossopharyngeal nerve, and over the vagus nerve to open in the piriform sinus.
Fourth branchial cleft anomalies have never been seen in their entirety.
Theoretically, they would have an external opening anterior to the sternocleidomastoid muscle in the lower neck.
They would descend along the carotid sheath into the chest, passing under the subclavian artery on the right and the aortic arch on the left, ascend into the neck to cross the hypoglossal nerve, then descend to open into the esophagus.
Characteristics
Branchial cleft cysts are generally smooth, round, nontender masses.
An increase in size during upper respiratory infections is common.
An infected branchial cleft cyst may abscess or rupture spontaneously to form a sinus.
The size and the location of a branchial cleft anomaly determine the symptoms.
Large cysts may cause dysphagia, stridor, and dyspnea.
Small cysts are often not discovered until adulthood because of their slow rate of growth and minor symptoms.
P.366
Treatment
Complete excision without damage to the surrounding vital structures is the definitive treatment. Antibiotics are given if the lesion is infected.
Incision and drainage are avoided, if possible, because they make subsequent excision more difficult.
G
Encephaloceles are congenital brain herniations, which may be confused with nasal dermoids or polyps. Meningitis or cerebrospinal fluid leaks are not uncommon, particularly with manipulation.
Anatomy
They are usually discovered early in life. Approximately 75% are occipital, 15% are sincipital, and 10% enter the nose or nasopharynx.
These lesions may or may not communicate centrally. Communicating lesions increase in size and tension when the infant cries; noncommunicating ones generally do not.
Treatment should include total removal. The lesions do not need to be treated as emergencies if there is no imminent threat of meningitis.
IV Acquired Lesions
A
Leukoplakia and keratosis are white lesions that occur on the mucosa of the mouth, pharynx, or larynx. Erythroplakia is a similar red patch.
Etiology. These lesions are associated with repeated trauma (e.g., from poorly fitting dentures, decayed teeth), smoking, or use of alcohol. There is little correlation between the clinical appearance of the lesions and their histology. Erythroplakia is somewhat more likely to be carcinoma.
Diagnosis. Biopsy, to rule out squamous cell carcinoma, should be performed:
In high-risk patients (smokers and drinkers)
If the lesion persists after the removal of an irritative focus
Treatment. Benign leukoplakic lesions require no treatment but do require continued observation.
B Papillomas
Squamous papillomas of the oral cavity usually occur singly but may be multiple. They are common on the palate and faucial arches.
They are usually pedunculated and cauliflowerlike in appearance.
Recurrence is rare after excision.

Nasal papillomas
Squamous papillomas of the nasal cavity are warts that are similar in appearance and behavior to cutaneous warts elsewhere on the body.
Cylindrical and fungiform papillomas are other forms of benign nasal papillomas.
Inverted papillomas
Anatomy
The lesions typically arise from the lateral nasal wall and can invade the sinuses and orbits.
Grossly, the lesions appear bulky and deep red to gray in color. They vary in consistency.
Unlike nasal polyps of allergic origin (see IV C), they are unilateral.
Characteristics
Patients generally present with nasal obstruction, a postnasal drip, and headaches. A few have epistaxis. These lesions occur mainly in men between 50 and 70 years of age.
The reported incidence of malignant degeneration is about 2%. The incidence of associated malignancy in adjacent tissue is as high as 15%.
Treatment is complete excision. Recurrence is common because excision is often incomplete.
P.367
Laryngeal papillomas are the most common laryngeal tumors of childhood and may be found at any age.
Juvenile type. This type occurs predominantly in childhood and tends to involute at puberty.
Etiology. The etiology is viral.
Characteristics
Multiple papillomas are the most common characteristic. They may involve the airway from the epiglottis to the bronchi. The vocal folds are usually involved.
Hoarseness is an early sign, and obstruction is a later one.
Treatment
A tracheotomy may be necessary but should be avoided if possible because it predisposes to tracheal seeding of the papillomas.
Laryngoscopic removal, often by the use of a carbon dioxide laser, is the mainstay of therapy.
Interferon therapy has not proved to be as useful as early reports predicted. Other medical therapies are under investigation.
Recurrence and spread are currently common.
Adult type. In this form, the papilloma is generally single.
As in the juvenile form, the papilloma tends to recur following excision.
Recurrent lesions can undergo malignant transformation, particularly in patients exposed to radiation.
C
Nasal polyps are rare before 5 years of age and occur more commonly in men.
Etiology. Nasal polyps are believed to be an allergic response, but this etiology has not been clearly established.
They may be associated with asthma and an idiosyncratic reaction to aspirin.
In children, the presence of nasal polyps should prompt a sweat test to rule out cystic fibrosis.
Characteristics
Inflammatory polyps are almost always bilateral and may recur frequently.
Involvement of the paranasal sinuses is common.
Treatment. Polyps are excised if they obstruct the nasal airways or the sinus drainage pathways.
D Fibrous lesions
Nodular (proliferative) fasciitis presents as a rapidly growing, discrete soft tissue mass.
Etiology
Probably a reactive, non -neoplastic response to injury, it may occur at any time from childhood to age 70.
The lesions may be mistaken for sarcoma.
Characteristics. Fascia is the primary tissue involved.
Treatment. The lesions generally do not recur after excision.
Proliferative myositis occurs in adults and appears to be post-traumatic in origin.
Characteristics
Like nodular fasciitis, it can be confused with sarcoma.
The lesion involves muscle diffusely.

Occasionally, spontaneous regression occurs.
Treatment. Lesions do not recur after excision.
Traumatic myositis ossificans, bony deposits in muscle due to trauma, generally presents as a painful mass in the muscle 1–4 weeks after a single severe trauma.
Characteristics
In the head and neck, the masseter or sternocleidomastoid is generally involved.
Radiography reveals feathery opacities or irregular radiodensities.
The condition must be differentiated from myositis ossificans progressiva , which is a progressive, systemic illness that begins early in life and results in the conversion of muscle tissue to bony tissue.
Treatment. Persistent painful masses are excised. Local recurrence is common.
P.368
Desmoid tumors are benign, locally invasive, encapsulated tumors.
Etiology
They arise from the muscle fascia and are often associated with prior trauma.
These tumors are uncommon in the head and neck but, when found, usually arise from the sternocleidomastoid muscle.
Treatment. Complete surgical excision is the treatment of choice.
E Tumors of skeletal muscle
Characteristics
Extracardiac rhabdomyomas have a predilection for the head and neck.
They show a slight male predominance.
Signs and symptoms depend on the site and size of the tumor.
Treatment. Rhabdomyomas are treated with complete surgical excision, if possible, followed by chemotherapy and radiation.
F Tumors of peripheral nerves
(see Chapter 26, II B 6)
Schwannomas are solitary, encapsulated tumors attached to or surrounded by a nerve. They are primarily located centrifugally and are often painful and tender. They are not associated with von Recklinghausen's disease or with malignant change, in contrast to neurofibromas.
Acoustic neuromas constitute a type of schwannoma.
Etiology. They arise from the eighth cranial nerve, usually start within the internal auditory canal, and can involve the cerebellopontine angle.
Characteristics. Signs and symptoms may include hearing loss, tinnitus, imbalance, and vertigo. Asymmetric sensorineural hearing loss is common and requires that acoustic neuroma be ruled out.
Evaluation. Testing includes an audiogram, an auditory brain stem response test, and an MRI with gadolinium enhancement.
Treatment. Early discovery is important because it results in earlier resection, with a consequent decrease in morbidity and mortality.
Von Recklinghausen's neurofibromatosis (NF I)
Etiology. It is caused by a nerve growth factor gene on chromosome 17q11.2. Inheritance is autosomal dominant.
Characteristics
Neurites (axons) pass through the tumor.
Lesions are usually multiple and unencapsulated.
In 8% of patients, neurofibromas undergo malignant changes.
Usually, these lesions are located centripetally and are characteristically asymptomatic.
Café au lait spots, vitiligo, gliomas (especially optic), osseous changes, Lisch nodules (iris hamartomas) meningitis, spina bifida, syndactyly, hemangiomas, axillary or inguinal freckling, NF I in a first -degree relative, or retinal and visceral manifestations may be present.
Central neurofibromatosis (NF II)
Etiology. It is caused by an abnormality on chromosome 22q11.21 -13.1 and involves encoding of a suppressor protein called schwannomin . Inheritance is autosomal dominant, but almost 50% of cases are new mutations.
Characteristics
Classically, slow -growing, bilateral acoustic neuromas or neurofibromas cause hearing loss or dizziness and lead to a diagnosis by age 20.
The diagnosis may also be established by a unilateral eighth nerve mass and:
A relative with NF II or,
Any two of the following: glioma, juvenile posterior subscapular lenticular opacity, meningioma, neurofibroma schwannoma
Café au lait spots, posterior lens cataracts, and cutaneous neurofibromas are uncommon. Lisch nodules are not found.
P.369
Wishart type: Early onset rapid growth, other fibromatous tumors in addition to eighth nerve masses
Gardner type: Later onset, slow growth rate, usually bilateral acoustic neuromas only
Traumatic neuromas are reactive hyperplasias due to a nerve's attempts at regeneration after injury. They are generally oval or oblong, gray, firm, and unencapsulated. Persistent hyperesthesia and tenderness are the usual signs.
Most neurogenous tumors of the head and neck can be excised safely without sacrificing nerves. If an important nerve must be cut, it should be generally reanastomosed or a nerve graft should be interposed.
G Granular cell tumors
Congenital epulis occurs on the gum pads of newborns in the region of the future incisors. The lesion can be quite large, does not recur after excision, and may spontaneously regress. The female:male ratio is 8:1.
Nonepulis form of granular cell tumors occurs mainly in young adults, especially in blacks.
H
Paragangliomas (chemodectomas) can occur in the head or neck (see Chapter 19, XII).
I Nondental lesions of the jaw
Giant cell granuloma
Types. This jaw lesion can occur in two forms:
Central granulomas occur within the jaw.
Peripheral granulomas , occurring on the gingival or alveolar mucosa, are four times more common.
Characteristics. The mucosa is generally intact, but radiographs of the central lesions show radiolucent areas.
Treatment. Excision or curettage is the treatment of choice.
Fibrous dysplasia of the jaw is noted early in life.
Characteristics
It shows active growth in childhood and stabilization in adulthood.
Enlargement of the bone is the most common sign and may be either minor or significant enough to cause obvious facial asymmetry.
The maxilla is more commonly involved than the mandible.
Radiographs reveal sclerosis, lytic lesions, or unilocular lesions.
Treatment
Obvious deformity, pain, or interference with function suggests the need for surgery.
Malignant transformation is possible but uncommon, and conservative resection appears to be the best treatment.
Torus is a benign bony growth, occurring at the midline of the palate (maxillary torus) or bilaterally lingual to the bicuspid (mandibular torus). Tori grow slowly and generally have no significance except that they may interfere with the fitting of dentures.
Osteomas are slow -growing, benign tumors in the sinuses, jaws, or external ear canals. They may require excision if they produce a headache or an occlusion of drainage.
J Laryngeal lesions
Laryngocele is a dilatation of the laryngeal saccule, producing an air sac that communicates with the laryngeal ventricle. Anything that increases intralaryngeal pressure increases the size of a laryngocele (e.g., coughing, straining, playing a wind instrument). A laryngopyocele is an infected laryngocele. It can be fatal if it results in asphyxia or if the purulent contents are aspirated into the tracheobronchial tree.
Anatomy. Laryngoceles may be unilateral or bilateral. They may also be internal (within the larynx), external (presenting in the neck), or both (combined).
An internal laryngocele causes bulging of the false cord and aryepiglottic fold.
An external laryngocele appears as a neck swelling at about the level of the hyoid bone and anterior to the sternocleidomastoid.
P.370
Characteristics
Internal laryngoceles cause hoarseness, breathlessness, and stridor on enlargement.
External laryngoceles increase in size with coughing or the Valsalva maneuver.
They are tympanic to percussion.
A hissing may be heard as the laryngocele empties air into the larynx when the air pressure is reduced.
Diagnosis
Plain films may show cystic spaces that contain air.
Tomograms may help to demonstrate the continuity between the internal and external components.
CT and MRI scans show these lesions well.
Treatment
Symptomatic laryngoceles are treated by surgical excision.
Laryngopyoceles should be treated by incision, drainage, and subsequent excision. Antibiotics
are also appropriate.
Laryngeal webs
Characteristics
They may be congenital or may follow bilateral vocal fold trauma.
When extensive, they present with stridor, weak phonation, and feeding problems in infants.
Treatment. Excision or division is now generally the preferred treatment, and placement of a stent or keel is often required.
Vocal nodules
Anatomy. Vocal nodules are bilateral benign masses that usually occur at the junction of the anterior and middle thirds of the true vocal folds.
Etiology. They are associated with vocal abuse.
Treatment
Vocal nodules are best treated by modifying the patient's speaking or singing technique through voice therapy.
Surgery is rarely necessary and is generally performed only after failure of voice therapy.
Vocal polyps
Characteristics. Vocal polyps are usually unilateral and often do not regress with speech therapy— two important points in distinguishing the polyps from vocal nodules.
Treatment
The recommended therapy is careful excision with microscopic visualization and avoidance of injury to the underlying lamina propria.
In selected cases, the laser may be helpful.
Laryngeal granulomas
Anatomy. Laryngeal granulomas occur over the vocal processes of the arytenoid cartilages.
Etiology. They are generally the result of trauma, usually from an endotracheal tube, and are usually associated with reflux laryngitis. Voice abuse may be a factor.
Treatment
Antireflux therapy is often helpful.
They can regress as a result of treatment with antireflux medication and speech therapy.

They are best treated by excision of persistent granulomas after a period of voice and medical therapy.
Botulinum toxin is used for selected, recurrent cases.
Arytenoid dislocation
Etiology. Arytenoid dislocation generally is the result of endotracheal tube or external trauma.
Characteristics. A soft, breathy voice after extubation should arouse suspicion.
Treatment. Prompt reduction is advisable; otherwise, the arytenoid usually becomes fixed in the dislocated position. However, late reduction (after months or years) can be successful and should be attempted when diagnosis or treatment has been delayed.
P.371
Contact ulcers
Anatomy. Contact ulcers are mucosal disruptions usually located posteriorly on the vocal folds.
Etiology. They sometimes result from trauma (e.g., from intubation), occasionally from vocal abuse, and often from gastric reflux laryngitis or heavy coughing.
Treatment with antireflux medication and behavioral changes such as elevation of the head of the bed; avoidance of caffeine, chocolate, late -night snacks, and fried or fatty foods; and antacid therapy will usually result in prompt resolution of the ulcers. Antibiotics may be helpful.
V Infections of the Head and Neck
A
Common head and neck infections (e.g., otitis media, mastoiditis, and sinusitis) are now controlled with antibiotics, which must be given at high doses and over long periods for these sequestered spaces.
B Tonsillar and adenoidal hypertrophy and infection
Tonsillectomy with adenoidectomy was once the most common operation performed in the United States. It remains quite prevalent but is now performed for these specific indications:
Obstructive hypertrophy
Patients benefiting from tonsillectomy with adenoidectomy are those with airway obstruction, sleep apnea, cor pulmonale, dysphagia, or failure to thrive.
Adenoidectomy is performed in children with chronic nasal obstruction, especially when they also demonstrate chronic serous otitis media or orthodontic problems.
Recurrent infection. Patients with documented recurrent adenotonsillitis are improved after tonsillectomy with adenoidectomy. A history of three to six episodes annually is a relative indication.
Tonsillectomy is often suggested after treatment for peritonsillar abscess in patients with a history of previous tonsillitis.
C
Atypical mycobacteria infection presents as an inflamed mass or draining sinus in the head and neck. It is most common in children and adolescents.

Pulmonary involvement is rare.
It is commonly associated with the parotid or submandibular glands, but it is not isolated to these sites.
Fixation of overlying skin and sinus formation are common. Biopsy can lead to a chronically draining sinus tract.
Treatment is by surgical excision or curettage and drainage. Antimycobacterial drug therapy is not indicated.
