
Insufficiency, and (b) thyrotoxicosis or myxoedema.
(4) Concealed trauma : (a) Concussion, (b)
self-reduced neck injury, (c) blunt injury to the
heart, and (d) reflex vagal inhibition.
(5) Poisoning : Without microscopic change:
(a) Delayed suboxic or narcotic poisoning; (b)
Anaesthetic overdosage or maladministration; (c)
Neurotoxic or cytotoxic poisons, and (d) Plant
poisoning. .
(6) Miscellaneous : Allergy, drug idiosyncrasy, etc.
Non-medical persons believe that the cause of death can always be determined by autopsy. The police may press the doctor for giving a positive statement with regard to the cause of death. In such cases, the pathologist should admit his inability to give a positive opinion. Such obscure cases require clinical and laboratory investigations and interview with persons who had observed the deceased before he died, to know the signs and symptoms shown by the deceased before his death. Laboratory investigations may be bacteriological, virological, histological, biochemical and toxicological. In the absence of positive findings from these sources, a careful assessment of possible functional causes of death must be made, before any cause of death is given as undetermined. Even in these disappointing cases, the negative morbid anatomical and chemical examination is of great value in excluding injuries or poisons, which may have been alleged to have caused or played some part in the death. The presence of infectious, malignant, occupational and other diseases are also excluded. Though the pathologist cannot establish the cause of death, he can exclude many conditions which have been incorrectly attributed to have caused death.
(1) Natural Causes: Cardiac Lesions : Acute rheumatic carditis may cause sudden death in a young adult. In some such eases, naked-eye changes may be absent, but typical Aschoff bodies of rheumatic fever are found in the myocardium on microscopic examination. Acute toxic myocarditis of diphtheria may cause sudden death, in which the primary lesion in the nose or throat may be overlooked. Idiopathic myocarditis may cause sudden death. Brown atrophy of the heart and senile heart may prematurely fail suddenly. Small coronary thromboses and easily dislodged emboli may be overlooked. Acute occlusion of coronary artery may result from thrombosis or haemorrhage within the wall of the artery. Zones of occlusion are usually less than five mm. in length, and most of the occlusions occur within three cm. of the orifices of the vessels. First part of the anterior descending branch of left coronary artery within two cm. of its origin is commonly affected, followed by the proximal part of the right coronary artery, first part of the circumflex branch of left coronary artery, and the short main trunk of left coronary artery. Fresh thrombi are dark-brown, and attached to the vessel walls. Old thrombi appear as homogeneous yellowish or grey, firm plugs blocking the vessels. Most infarcts occur in the left ventricle in the anterior wall. Posterior infarcts may be due to blockage of either the right vessel or the circumflex branch of the left artery. Infarction usually occurs when the lumen is reduced to twenty percent or less. Right ventricle is involved in less than ten percent cases. Coronary insufficiency from narrowing of the lumen of major vessels may lead to chronic ischaemia and hypoxia of the muscle distal to the stenosis. Hypoxic myocardium is electrically unstable and liable to arrhythmias and ventricular fibrillation, especially at moments of sudden stress, such as exercise or an adrenaline response, such as anger or emotion. There is no need for the ischaemia to be severe enough to produce a myocardial infarct. At autopsy, no naked eye changes are seen for the first 12 to 18 hours. Oedema of the affected area of the muscle is the first sign, and the cut surface looks granular and dull. After 12 hrs to third day, the area becomes better demarcated, and turns yellow and is surrounded by an area of hyperaemia. In one to three days there is a progressive softening and thinning of infarcted area, which is maximum about the tenth day, and rupture may occur. Red streaks appear, a 'tigroid' appearance. From the third week the centre of the infarct becomes gelatinous, translucent and grey. From ten days onwards, the infarct is slowly converted into a fibrous scar, which is completed in three months. Histological changes are not seen before 8 to 12 hours after the onset of infarction. Transitory coronary artery spasm can cause death in persons suffering from angina without narrowing of the coronary arteries and without significant atherosclerosis or congenital anomalies. Severe narrowing of coronary arteries (at least 75%) without thrombosis or myocardial infarction is the common cause of sudden death. A physical or emotional stimulus may demand sudden increase in cardiac effort, and if the circulation of the deceased is unable to satisfy the immediate need for increased oxygen, death may result (acute coronary insufficiency). Sudden death with coronary heart disease usually results from ischaemia induced electrical instability of sudden onset, most often ventricular fibrillation. Fresh thrombotic lesions are seen in less than 25% of the cases, Transitory coronary artery spasm can cause death in persons suffering from angina without narrowing of the coronary arteries and without significant atherosclerosis or congenital anomalies. Lesions, such as myocarditis, fibrosis, and necrosis of conducting tissue may escape detection. A thrombus or an occlusive lesion in the terminal part of the artery may be overlooked. The ostia of the coronary arteries may be occluded by atherosclerosis of the aorta. Spasm of the coronaries may lead to cardiac arrhythmia and death. A ventricle which is overworked and under-nourished may suddenly go into ventricular fibrillation or asystole. This can occur even if the arteries are not completely blocked and is often precipitated by a sudden demand for an increased cardiac output. The lesions of the conducting system of the heart may sometimes cause arrhythmias and death. Any person with a heart in excess of 420 gm. is at risk of sudden death, even though the coronary arteries are normal. In these cases a state of electrical instability occurs from chronic hypoxia, so that sudden stresses, such as exercise or emotion can suddenly cause the arrhythmias.
Primary cardiac arrest during exercise: During or immediately after exercise ischaemia of myocardium, arrhythmias and sudden death can occur. During exercise there is progressive increase of systolic pressure and heart rate, but diastolic pressure is affected very little, and peripheral resistance is decreased. Levels of catecholamine increase, which continue to rise following cessation of exercise, with ten fold increase of epinephrine. Sudden death occurs with ischaemia sensitising the heart to the arrhythmogenic properties of the catecholamines.
Concealed Trauma: (a) Cerebral Concussion : This may cause death without any external or internal marks of injury.
(b) Neck Injury : Cervical spinal fracture-dislocation may occur in diving, fall on head, impact downstair with a wall-facing, from oblique impact or by fall of some object on the head, in such a way as to cause the dislocation especially with the head thrown back. The dislocation may be associated with tears of the ligaments and with the displacement of the skull from the spine. Sudden movements of the head over the spine with displacement may cause contusion and laceration of the spinal cord and rapid death. If death is delayed, there may be oedema, softening and necrosis of the cord. Injury to the spinal cord causes spinal concussion and may cause death. Unconsciousness is not seen in all persons, but all get up with residual tingling, numbness, weakness of arms or legs and gait defects. Routine autopsy and X-ray may not show any abnormality. The dislocation of the cervical segments is often self-reducing, and externally there may not be any injury, or there may be abrasions on the brow or chin. Complete dissection of spine is essential. The spinal cord, cut longitudinally, may show internal bruising. Death may be instantaneous.
(c) Blunt Injury to the Heart : Contusion
of the chest as in steering-wheel impacts, head-on
collisions, from blast or heavy punching, may
temporarily or permanently derange the heart with¬
out much evidence of trauma. Contusion of the
heart may cause death. Trauma may cause arterial
spasm and it is likely that a functional inhibition
or coronary spasm may cause sudden death that
sometimes follow upon blows to the chest.
(d) INHIBITION OF THE HEART: (vagal
inhibition; vaso-vagal shock; reflex cardiac arrest;
nervous apoplexy or instantaneous physiological
death): Sudden dealh occurring within seconds or
a minute or two due to minor trauma or relatively
simple and harmless peripheral stimulation are caused
by vagal inhibition. Pressure on the baroreceptors
situated in the carotid sinuses, carotid sheaths, and
the carotid body causes an increase in blood pressure
in these sinuses with resultant slowing of the heart
rate, dilatation of blood vessels and a fall in blood
pressure. In normal persons, pressure on the carotid
sinus causes minimal effects with a decrease in heart
rate of less than six beats per minute, and only a
slight reduction (less than 10 mm. Hg) in blood
pressure. Some individuals show marked
hypersensitivity to stimulation of the carotid sinuses,
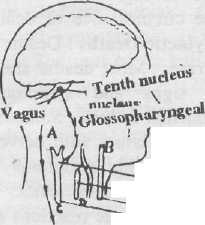
characterised by bradycardia and cardiac arrhythmias ranging from ventricular arrhythmias to cardiac arrest. This mechanism acts through a reflex arc in which the afferent (sensory) nerve impulses arise in the carotid complex of nerve endings, but not in the vagal nerve trunk itself. These impulses pass through glossopharyngeal nerves to the tenth nucleus in the brain stem, then return through the vagus (efferent) supply to the heart and other organs. This reflex arc acts through the parasympathetic side of the autonomic nervous system and is independent of the main motor and sensory nerve pathways. There is wide network of sensory nerves in the skin, pharynx, glottis, pleura, peritoneum covering viscera or extending into the spermatic cord, cervix, urethra, perineum and coeliac plexus. Afferent fibres from these tissues pass into the lateral tracts of the spinal cord, effect local reflex connections over several segments and also pass to the brain. The vagal nucleus is controlled by the synaptic connections in the spinal cord, which may be facilitated from both the sensory central cortex and from the thalamic centres. The latter may be responsible for emotional tone noted in the vagal reflex.
Carotid sinus
Larynx
![]()
Carotid artery
Fig.(6-5). The coarse distribution of the receptor system in vagal inhibition reflexes.
The commonest cause of such inhibition is pressure on the neck particularly on the carotid sinuses as in hanging or strangulation. Unexpected blows to the larynx, chest, abdomen and genital organs and the impaction of food in larynx or unexpected inhalation of fluid into the upper respiratory tract, or the insertion of an instrument into the bronchus, uterus, bladder or rectum, puncture of a pleural cavity usually for producing a pneumothorax, may cause sudden death. It may also be caused by the sudden distension of hollow muscular organs, e.g., during attempts at criminal abortion, when instruments are passed through the cervix or fluids are injected into the uterus. In degenerative diseases of the heart, e.g, sinus bradycardia and partial or complete A-V block, parasympathetic stimulation further depress the heart rate and may induce a Stokes-Adams attack which may be fatal. Cardiac arrest may also result from extensive injuries to the spine or other parts of the body, and from sudden evacuation of pathological fluids, e.g., ascitic or pleural, sudden immersion of body in cold water, alcohol, etc. Sudden terror may precipitate cardiac inhibition. There is great variation in individual susceptibility. Death from inhibition is accidental and caused by microtrauma. The stimulus should be sudden and abnormal for the reflex to occur. The reflex is exaggerated by a high state of emotional tension, and also any condition which lowers voluntary cerebral control of reflex responses, such as a mild alcoholic intoxication, a degree of hypoxia or partial narcosis due to incomplete anaesthesia.
Autopsy : When death results from inhibition, there are no characteristic post-mortem appearances. The cause of death can be inferred only by exclusion of other pathological conditions, and from the accurate observations by reliable witnesses, concerning the circumstance of death.
Anaphylactic Deaths : Deaths due to allergic reactions are rare. Most deaths are rapid and are preceded by signs and symptoms suggesting hyperacute bronchial asthma. Sometimes deaths are delayed for several hours with nervous symptoms, such as coma or with symptoms of circulatory failure resembling traumatic shock.
Aetiology: Allergic reactions may occur due to: (1) Drugs; Penicillin, aspirin, horse-serum products, iodine-containing agents. (2) Insect bites. (3) Foods: fish, shell-fish, eggs, nuts, fruits. (4) . Hormones: insulin, ACTH. (5) Enzymes: trypsin.
When an allergen is injected into the body, the antibodies formed by plasma cells combine with their antigens to form antigen/antibody complexes (allergens), which simulate mast cells to release histamine and similar substances. About 75% of patients dying of penicillin anaphylaxis do not have allergic reactions during earlier course of penicillin therapy. Patients should be observed for half hour after receiving the injection of antibiotics.
The anaphylactic syndrome is caused by local and systemic release of endogenous active substances. These include leukotrienes C, D, E, or histamine. eosinophilic chemotactic factor and other vasoactive substances, such as bradykinin and kallikrein. Anaphylactic shock is due to bronchospasm with contraction of the smooth muscle of the lungs, vasodilation, and increased capillary permeability. Death occurs due to laryngeal oedema, bronchospasm and vasodilation.
Signs and Symptoms: The onset of symptoms is within 15 to 20 min. General: malaise, weakness, sense of illness. Dermal: skin rashes, urticaria, pruritus, erythema. Mucosal: periorbital oedema, nasal congestion, pruritus, angio-oedema, cyanosis. R.S.: sneezing, rhinorrhoea, dyspnoea. Upper airway: laryngeal oedema, hoarseness, stridor, oedema of tongue and pharynx. Lower airway: dyspnoea, acute emphysema, asthma, bronchospasm. G.I: nausea, vomiting, dysphagia, abdominal cramps, diarrhoea C.V.S: tachycardia, palpitation, shock. C.N.S.: anxiety, convulsions.
Autopsy: Findings are non-specific. There is usually oedema of the larynx, emphysema, cyanosis, petechial haemorrhages, congestion and oedema of the lungs, visceral congestion, and infiltration of bronchial walls with eosinophils.
History is very important. In cases of insect bites, Ig E antibodies are found in the serum. Ig E binds to the mast cells and basophils. When the cells interact with specific antigens, they release a number of potent compounds, including histamines and an eosinophilic chemotactic factor, which causes an immediate hypersensitivity reaction.
Diagnosis: To establish diagnosis of death from allergic shock, the following should be established : (1) The injected material must be non-toxic to normal persons. (2) Characteristic allergic symptoms should be present before death. (3) Autopsy should not reveal the presence of any other lesion capable of causing death. (4) By the passive transfer
technique, a specific sensitising substance corresponding to the allergen must be demonstrated. Drug Idiosyncrasy : The administration of drags in amounts which are known to be harmless to normal person may cause death due to drug idiosyncrasy, e.g., many persons are hypersensitive to cocaine. The diagnosis is based mainly on clinical history.
