
- •Cytology
- •The cell
- •Plasma membrane or plasmalemma
- •Intercellular connections
- •The membranous organelles Endoplasmic reticulum (e. R.)
- •Rough e. R. (rEr)
- •Smooth e. R. (sEr)
- •Golgi apparatus
- •Lysosomes
- •Peroxisomes (microbodies)
- •Mitochondria
- •Microtubules
- •Cilia and flagella
- •Filaments
- •Inclusions
- •Nucleus
- •Chromatin
- •Nucleolus
- •Nucleoplasm
- •Cell cycle
- •Mitosis
- •Embryology
- •The spermatozoon
- •Ovums or ovocytes
- •Fertilization
- •Penetration of Zona Pellucida
- •Fusion of Pronuclei
- •Cleavage
- •Blastocyst Formation Compaction
- •Cavitation
- •Gastrulation
- •Human developmental periods
- •Progenesis
- •Derivations of the ectoderm
- •Derivations of the mesoderm
- •Derivations of the endoderm
- •Fetal membranes
- •Placenta
- •Placental barrier
- •Umbilical cord
- •Amniotic fluid
- •Tissues
- •Classification of epithelium
- •Functions of a blood
- •Red blood cells
- •White blood cells
- •Neutrophils
- •Eosinophils
- •Basophils
- •Lymphocytes
- •Monocytes
- •Platelets
- •Hematopoiesis
- •Hematopoiesis in embryonic and fetal life
- •Pluripotential hematopoietic stem cells
- •Connective tissue
- •Loose connective tissue
- •Dense connective tissue
- •Connective tissue (c.T.) with special properties
- •Brown adipose c.T.:
- •Connective tissue fibers
- •Collagen fibers
- •Reticular fibers
- •Elastic fibers
- •Ground substance
- •Connective tissue cells
- •Fibroblasts and myofibroblasts
- •Macrophages
- •Mast cells
- •Hyaline cartilage
- •Fibro cartilage
- •Bone cells Osteoblasts
- •Osteocytes
- •Osteoclast
- •Classification of bone tissue
- •General structures of bones
- •Cartilage Arises From Mesenchyme
- •Bone formation
- •Intramembranous Ossification
- •In Intramembranous Ossification, Bone Is Formed by Differentiation of Mesenchymal Cells Into Osteoblasts
- •Endochondral Ossification
- •Growth of Endochondral Bone
- •Muscle tissue
- •Classification of muscle
- •Skeletal muscle
- •Skeletal muscle fibers
- •Myofibrils and myofilaments
- •Organization of a skeletal muscle
- •Cardiac muscle
- •Smooth muscle
- •Contraction and its control
- •Nervous tissue
- •Dendrites and axons
- •Synapses
- •Axonal transport systems
- •N euroglia
- •Functions of neuroglia
- •Schwann cells and the myelin sheath
- •Literature
Platelets
Figure21. Diagram of the human platelet

Blood platelets (thrombocytes) are nonnucleated, disk-like cell fragments 2-4 μm in diameter. They range in number from 180-320xl09/L of blood. Platelets derive from large cells in the bone marrow, called megakaryocytes.
In the formation of platelets, small bits of cytoplasm are separated from the peripheral regions of the megakaryocyte.
Human platelets have a life span of about 10 days. In stained blood smears, platelets often appear in clumps. Each platelet has a peripheral light blue-stained transparent zone, the hyalomere and a central zone containing purple granules, called the granulomere.
Platelet functions:
1. Primary aggregation
Discontinuities in the endothelium, produced by blood vessel lesions, are followed by absorption of plasma proteins on the subjacent collagen. Platelets immediately aggregate on this damaged tissue, forming a platelet plug.
2. Secondary aggregation.
Platelets in the plug release the content of their alfa and delta granules.
3. Blood coagulation
During platelet aggregation, factors from the blood plasma, damaged blood vessels and platelets promote the sequential interaction (cascade) of approximately 13 plasma proteins, giving rise to a polymer, fibrin that forms a three-dimensional network of fibers trapping red cells, leukocytes and platelets to form a blood clot or thrombus.
4. Clot retraction.
5.Clot removal.
Hematopoiesis
Mature blood cells have a short life span, and consequently the population must be continuously replaced with the progeny of stem cells, produced in the hematopoietic organs.
In the adult, red blood cells, granulocytes, monocytes and platelets are formed both in the red bone marrow, lymphocytes are formed both in the marrow and in the lymphatic tissues.
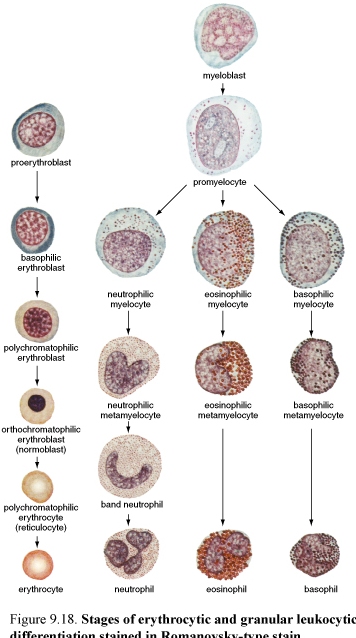
Figure22. Stages of erythrocytic and granular leukocytic differentiation (left) and dynamics of hemopoiesis in embryonic and fetal life (right)
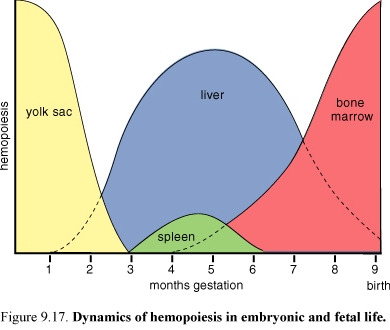
Hematopoiesis in embryonic and fetal life
The first phase of hematopoiesis occurs in “blood islands” in the wall of the yolk sac.
In the second or hepatic phase, hemopoietic centers appear in the liver and lymphatic tissues.
The third phase involves the bone marrow (and other lymphatic tissues).
After birth, hemopoiesis occurs in the red bone marrow and in lymphatic tissues as in adult.
The origin and maturation of the blood cells are termed, respectively, erythropoiesis, granulopoiesis.
Pluripotential hematopoietic stem cells
It is believed that all blood cells arise from a single type of stem cell in the bone marrow. Because this cell can produce all blood cell types, it is called a pluripotential stem cell.
These cells proliferate and form one cell lineage that will become lymphocytes (lymphoid cell) and another lineage that will form the myeloid cells that develop in bone marrow (granulocytes, monocytes, erythrocytes and megakaryocytes).
These unipotential or bipotential progenitor cells generate precursor cell (blasts).
“Illustration of the morphologically recognizable stages of erythrocytic and granular leukocytic differentiation in myeloid tissue”
